 |
 |
- Search
| Clin Shoulder Elb > Volume 21(3); 2018 > Article |
Abstract
Background
In a previous study undertaken to quantify capsular volume in rotator cuff interval or axillary pouch, significant differences were found between controls and patients with instability. However, the results obtained were derived from two-dimensional cross sectional areas. In our study, we sought correlation between three-dimensional (3D) capsular volumes, as measured by magnetic resonance arthrography (MRA), and multidirectional instability (MDI) of the shoulder.
Methods
The MRAs of 21 patients with MDI of the shoulder and 16 control cases with no instability were retrospectively reviewed. Capsular areas determined by MRA were translated into 3D volumes using 3D software Mimics ver. 16 (Materilise, Leuven, Belgium), and glenoid surface area was measured in axial and coronal MRA views. Then, the ratio between capsular volume and glenoid surface area was calculated, and evaluated with control group.
Multidirectional instability (MDI) of the shoulder is a complex condition that causes excessive motion and translation in more than one direction. Its underlying pathology is increased capsular laxity and rotator cuff interval elongation [1-3]. Magnetic resonance arthrography (MRA) is a known gold standard method for evaluating shoulder instability, and is highly sensitive at detecting capsular laxity and redundancy [4,5]. In a previous study undertaken to find relations between capsular areas using two-dimensional (2D) cross-sectional areas (CSA) and various instability conditions of the shoulder, significant difference was found between control and instability patients [1].
In our study, three-dimensional (3D) volume measurements were performed in MDI patients and control groups, and the difference between them was significant and the differences from previous 2D results were examined.
An informed consent was taken from all study participants and the study has been approved by Institutional Review Board of Chosun University Hospital. Patients who underwent MRA examination in Chosun University Hospital from August 2010 to August 2013 were included in this study. Of the total 78 patients, 21 were diagnosed with MDI and the remaining 57 were not diagnosed with MDI. The exclusion criteria applied to all 41 study members were; glenoid bony deficiencies, engaging Hill-Sachs lesions and degenerative arthritic changes, rotator cuff tear, traumatic dislocation or previous surgery on the involved shoulder. Finally, 16 patients were used for the analysis as a control group.
The MRAs of 21 patients with mean age of 25.5 years (range, 17ŌĆō38 years) with MDI were reviewed in a computerized search of radiologic and clinical files of Chosun University Hospital. All patients had a diagnosis of MDI based on clinical history, physical examination, MRA. And the patient was diagnosed with MDI having persistent instability symptom of the shoulder and global instability in physical examination. All patients had capsular stretch and no labral tear in MRA.
A control group of 16 cases with mean age of 29.8 years (range, 16ŌĆō48 years) without clinical instability were identified. Members of the control group had no history of shoulder trauma and no evidence of instability by physical examination.
Contrast medium for MRA was injected using the rotator interval approach. Briefly, a 22-gauge spinal needle was placed in the glenohumeral joint and with 20 ml of normal saline with contrast media was instilled. Magnetic resonance imaging (MRI) was performed with the patientŌĆÖs arm adducted and the hand in a neutral position.
All patients underwent MRA examinations using a 1.5-T unit (Avanto; Siemens, Erlangen, Germany) equipped with a phased-array HD shoulder coil. All subjects were imaged supine. The following MRA imaging sequences were used: axial, oblique coronal and oblique sagittal proton density turbo spin echo sequences.
Capsular areas in images were converted into 3D capsular model using 3D software Mimics ver. 16 (Materilise, Leuven, Belgium) (Fig. 1). The 3D boundary of the uniform high signal area corresponding to contrast material in the capsule was drawn automatically. Small amount of extra-capsular leakage of contrast material was removed manually to facilitate volume calculations. Capsular 3D volumes were measured automatically by the same program, and reference measurements of glenoid articular surface area was made by simply multiplying largest anterior to posterior (AP) distance in axial view by the largest superior to inferior (SI) dimension of the glenoid in coronal view (Fig. 2). Glenoid dimensions were measured using a PACS using a cursor, lengths were calculated automatically. These reference measurements were used to correct for variances in glenoid size by calculating ratios between glenoid articular surface areas and capsular fluid pocket volumes.
The capsular volume to glenoid surface area ratios were compared using the StudentŌĆÖs t test. Statistical charts were generated using Excel 2007 (Microsoft, Redmond, WA, USA). Inter-group comparisons were conducted by using SPSS ver. 13.0 software (SPSS Inc., Chicago, IL, USA) and power analysis was performed using PASS 2008 software (NCSS, Kaysville, UT, USA). p-values of <0.05 were considered significant and values of <0.01 as highly significant.
Mean capsular volume was 26.248 ┬▒ 5.664 cm3 in the instability group and 19.028 ┬▒ 6.047 cm3 in the control group (Fig. 3). Mean glenoid surface area was 7.45 ┬▒ 1.29 cm2 in the instability group and 7.41 ┬▒ 1.43 cm2 in the control group (Table 1). The 3D capsular volume to glenoid surface area ratios were significantly different between the instability and control groups (3.59 ┬▒ 0.83 cm3/cm2 and 2.53 ┬▒ 0.62 cm3/cm2, respectively; (p<0.01) with instability group showing the higher ratios.
MDI of the shoulder is a complex problem to diagnose and treat [6]. Various diagnostic methods have been suggested, but they are diagnosed by the clinical symptoms of the patient and physical examination of the physician, which may be subjective. There are various studies on the pathogenesis of MDI, studies on cadavers have found that an excessively redundant capsule is one of the important reasons for symptomatic laxity in MDI [7,8]. There have been attempts to diagnose MDI through objective radiological examinations. Some authors have tried to assess capsular width using MRA to facilitate objective evaluation [9,10]. Dewing et al. [1] attempted to correlate capsular CSA, measured by MRA, with specific conditions like anterior, posterior, and MDI of the shoulder, and used maximum capsular distension distance and the size of the humeral head to correct for variances. Ng et al. [11] evaluated the relationship between capsular width and number of dislocations, type of capsular attachment, presence of antero-inferior labral tear, and patient sex. They also compared the sensitivities and specificities of MRI and clinical tests in instability of the shoulder. However, radiologic examinations have played an additional role in the diagnosis of MDI and have not become a definitive diagnostic method. In a previous study undertaken to find relations between capsular areas using 2D CSA, the attempt to measure the increased joint volume in 2D would have been limited method.
We believe that the value accurate 3D volumetric measurements. We investigated the 3D volume measured by this method that is useful for MDI diagnosis. For each individual, the size of the joints may vary according to body type and body size. To correct this, we measured glenoid surface area in addition to the joint volume. The results showed that there was no significant difference in the glenoid surface between the MDI patients and the control group, but 3D capsular volume to glenoid surface area ratios was increased.
Nevertheless, our study has several limitations. First, only a limited number of patients were recruited, and the date doesnŌĆÖt follows the normal distribution curve. Furthermore, reference point which distinguishes the two groups couldnŌĆÖt be presented through this method. Thus, we suggest that a prospective study of larger scale needs to be conducted to determine the significance of intergroup differences. Second, we multiplied the AP and SI dimensions of the glenoid surface area, but it would be more accurate to calculate values based on 3D data. However, this was not possible because the glenoid surface was too indistinct in MRA images to measure accurately. Higher definition MRA would probably allow the accurate calculation of glenoid surface areas. Third, this study was performed retrospectively, and the diagnosis of MDI patients diagnosed by one expert may be inaccurate. Lastly, there is a limitation in that in a retrospective study, no shoulder can be defined as completely normal as opposed to MDI while setting the control group.
We suggest that the measurement of 3D volume through MRA can be an useful measurement method for MDI diagnosis. In addition, we can present a more objective diagnostic value through a larger scale prospective study. We think that it can be used to evaluate the results after surgical treatment such as arthroscopic thermal shrinkage management, arthroscopic capsular plication and open capsular shift. In addition, if multiple 3D images were superimposed, they might show the direction of capsular expansion, which would be helpful for surgical planning [12]. The 3D volume process through MRA will be worth researching.
Fig.┬Ā1.
Capsular areas of arthrograms axial veiws (A) were translated in terms of three-dimensional volume (B) using image-processing software.

Fig.┬Ā2.
Glenoid surface area was measured using axial (A) and coronal (B) magnetic resonance arthrography images.
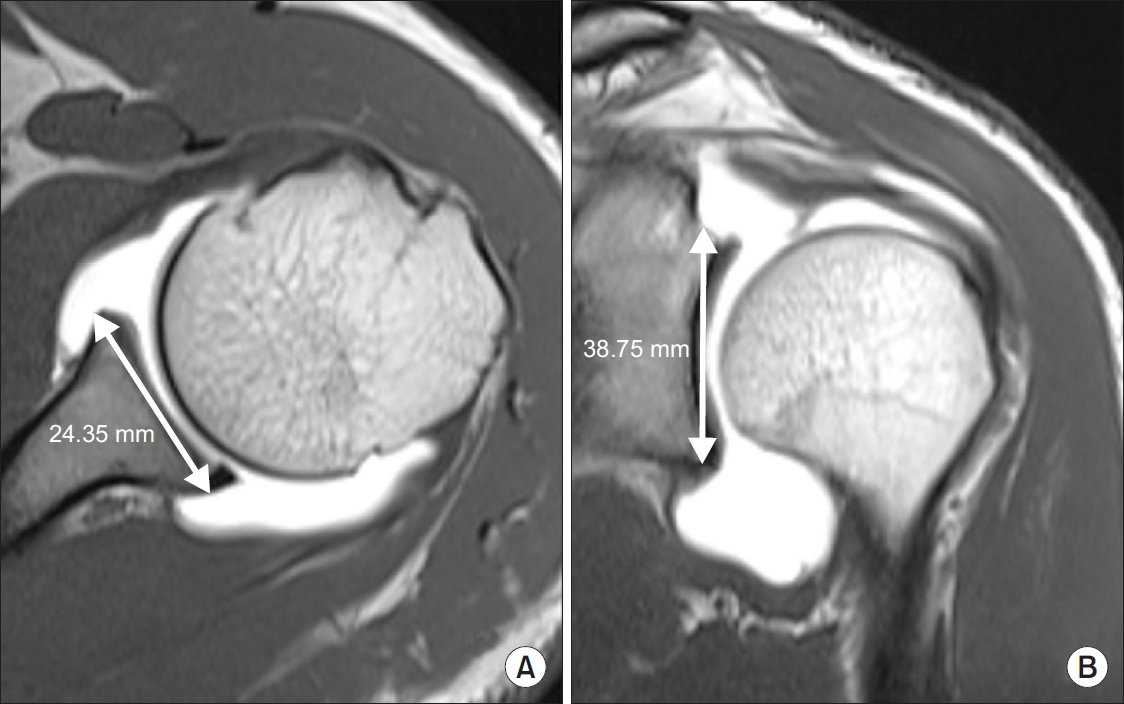
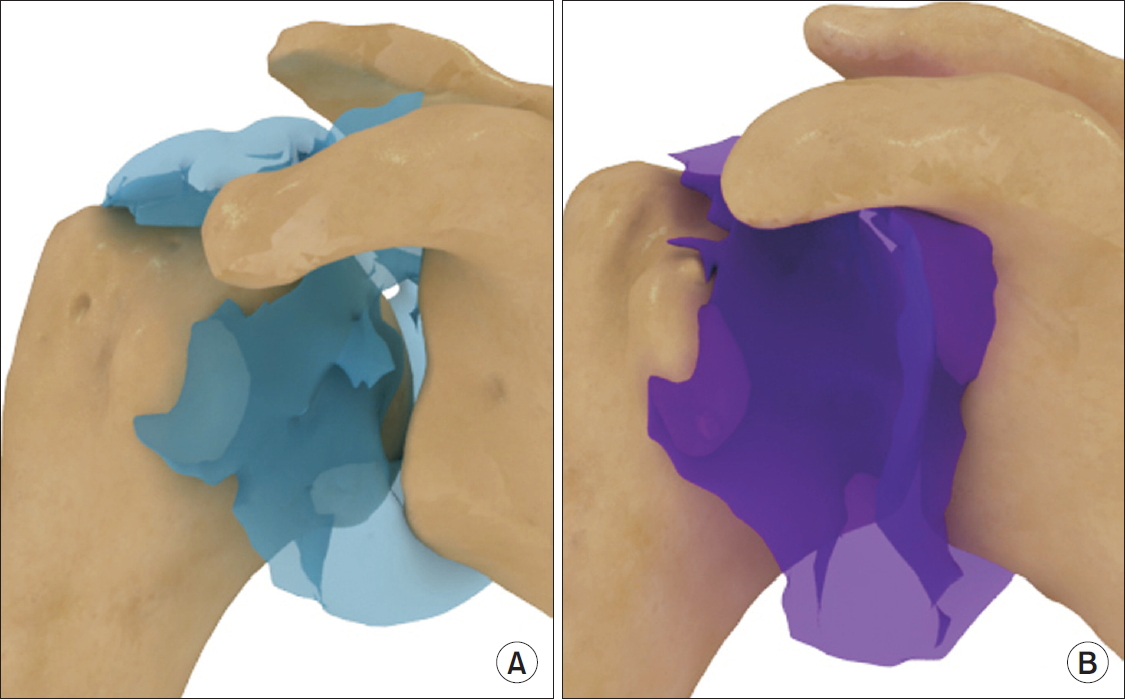
Fig.┬Ā3.
Reconstructed three-dimensional model from the shoulder magnetic resonance arthrogram in normal (A) and in multidirectional instability of the shoulder (B). It is showing expansion of the capsular volume inferior pouch, especially.
Table┬Ā1.
Three-dimensional Capsular Volume and Glenoid Surface Area in Multidirectional Instability of the Shoulder
References
1. Dewing CB, McCormick F, Bell SJ, et al. An analysis of capsular area in patients with anterior, posterior, and multidirectional shoulder instability. Am J Sports Med 2008;36(3):515ŌĆō22.


2. Provencher MT, Dewing CB, Bell SJ, et al. An analysis of the rotator interval in patients with anterior, posterior, and multidirectional shoulder instability. Arthroscopy 2008;24(8):921ŌĆō9.


3. Schenk TJ, Brems JJ. Multidirectional instability of the shoulder: pathophysiology, diagnosis, and management. J Am Acad Orthop Surg 1998;6(1):65ŌĆō72.


4. Lee HJ, Kim NR, Moon SG, Ko SM, Park JY. Multidirectional instability of the shoulder: rotator interval dimension and capsular laxity evaluation using MR arthrography. Skeletal Radiol 2013;42(2):231ŌĆō8.


5. Morag Y, Jacobson JA, Shields G, et al. MR arthrography of rotator interval, long head of the biceps brachii, and biceps pulley of the shoulder. Radiology 2005;235(1):21ŌĆō30.


6. Kim SH. Multidirectional instability of the shoulder: current concept. Sports Med Arthrosc Rehabil Ther Technol 2009;1(1):12.



7. Lubiatowski P, Ogrodowicz P, Wojtaszek M, Breborowicz M, D┼éugosz J, Romanowski L. Arthroscopic capsular shift technique and volume reduction. Eur J Orthop Surg Traumatol 2012;22(6):437ŌĆō41.


8. Wiater JM, Vibert BT. Glenohumeral joint volume reduction with progressive release and shifting of the inferior shoulder capsule. J Shoulder Elbow Surg 2007;16(6):810ŌĆō4.


9. Rand T, Trattnig S, Breitenseher M, Wurnig C, Marschner B, Imhof H. The postoperative shoulder. Top Magn Reson Imaging 1999;10(4):203ŌĆō13.


10. Tirman PF, Stauffer AE, Crues JV 3rd, et al. Saline magnetic resonance arthrography in the evaluation of glenohumeral instability. Arthroscopy 1993;9(5):550ŌĆō9.


- TOOLS
-
METRICS

-
- 2 Crossref
- 15,399 View
- 52 Download
- Related articles in Clin Should Elbow
-
Arthroscopic Global Capsular Release in the Refractory Frozen Shoulder 1998 December;1(2)








