|
 |
- Search
| Clin Shoulder Elb > Volume 25(2); 2022 > Article |
|
Abstract
Background
Rotator cuff tears cause pathologies of the long head of the biceps tendon (LHBT). One of the surgical treatments for such a tear is LHBT tenodesis to the humerus. This study aims to compare simultaneous rotator cuff repair and LHBT tenodesis with or without detachment of the proximal end of the LHBT (PELHBT) from its site of adhesion to the glenoid.
Methods
This retrospective study involved patients affected by LHBT pathology with rotator cuff tear. The patients were divided into two groups, with or without PELHBT detachment from the glenoid. Therapeutic outcomes were investigated by evaluation of patient satisfaction, pain based on visual analog scale, shoulder function based on Constant score and simple shoulder test, and biceps muscle strength based on the manual muscle testing grading system before surgery, at 6 months, and at the final visit after surgery.
Results
Groups 1 and 2 comprised 23 and 26 patients, respectively, who showed no significant differences in demographic characteristics (p>0.05). Shoulder function, biceps muscle strength, pain, and satisfaction rate improved over time (p<0.05) but were not significantly different between the two groups (p>0.05). No post-surgical complication was found in either group.
Biceps tendon pathology usually is accompanied with rotator cuff tears. Such tears can cause intense pressure and friction on the tendon of the biceps muscle [1]. This pressure damages the biceps muscle and causes pathology in up to 76% of patients who have undergone arthroscopic rotator cuff repair [2].
Commonly, this problem is treated by biceps tenodesis or tenotomy [3,4]. Long head of the biceps tendon (LHBT) tenodesis refers to connection of this tendon to the proximal end of the humerus. This is performed to maintain resting muscle length, minimize cramping, prevent cosmetic deformity and muscle atrophy, and maintain elbow flexion and supination strength [5,6]. Tenodesis is suggested for young and active patients with loss of less than 50% of tendon fibers and internal sublocations of the biceps tendon muscle [7,8].
LHBT tenodesis is a reliable treatment for rotator cuff repair. Among more than 15 techniques for tenodesis [9], intra-articular tenodesis of the LHBT was conducted in this study. The biceps muscle tendon, which is between the site of LHBT tenodesis and its attachment to the supraglenoid, was considered the proximal end of the LHBT (PELHBT). There is no consensus on performance of tenodesis with or without PELHBT detachment. Kandeel [10] reported that, although biceps tenodesis without PELHBT detachment can be accompanied by disadvantages such as range deficits in external rotation and relatively high prevalence of post-surgery tenderness and pain, the final results are acceptable. On the other hand, detachment of the tendon can cause instability, dysfunction, and significant upward migration of the humerus to the subacromial space [11,12].
As few studies have compared the results of tenodesis with or without detachment of the PELHBT, the need for such detachment is not known. This study aims to compare the results of tenodesis with or without detachment of PELHBT from the supraglenoid tubercle to determine the optimal surgical method.
The protocol for this study was approved by the Institutional Review Board of Islamic Azad University (IRB No. 3521). All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975 in its most recently amended version. Informed consent was obtained from all patients included in the study
This is a cross-sectional retrospective study performed Poursina Hospital, Rash, I.R. Iran. All patients with a background of LHBT pathology (tenosynovitis, partial dislocation, dislocation, and tendon tear) accompanied by full thickness rotator cuff tear were included in the study at least 2 years after surgery. Patients with a history of shoulder surgery, psychological diseases, unwillingness to participate in the study, lack of complete surgical repair of the rotator cuff, neurological diseases involving the affected shoulder, pain in both shoulders, and a life expectancy of less than 2 years were excluded from the study. Finally, 57 patients (57 shoulders) were included in the study. All the patients had results available for at least a positive biceps test (biceps instability or active comparison test, speed test, or YergasonŌĆÖs test). The patients also had at least one of the following lesions requiring surgery: inflammatory lesion, partial tear, dislocation, superior labrum anterior, or posterior lesion. All patients underwent MRI before arthroscopic cuff repair and LHBT tenodesis. However, the decision to perform tenodesis was based on biceps pathology during surgery.
After arthroscopic repair and LHBT tenodesis in patients who underwent surgery during 2014 to 2016, the PELHBT was detached from its adhesion (group 1). In years between 2017 and 2019, it was assumed that PELHBT was needed for shoulder joint stabilization and prevention of humerus head migration, and detachment was not performed (group 2).
Demographic information (age, sex, involved shoulder, and dominant hand) and radiographic findings including acromial type were extracted from the patientsŌĆÖ medical files. Therapeutic outcomes were investigated by evaluation of patient satisfaction rate and pain based on visual analog scale (VAS), shoulder function status according to the Constant score (CS) and simple shoulder test (SST), and biceps muscle strength based on the manual muscle testing (MMT) grading system before surgery, at 6 months, and at the final visit after surgery. Biceps muscle strength during elbow flexion and forearm supination was assessed by another surgeon (Kamran Asadi) and reported as the average.
All surgeries were performed under general anesthesia in a beach-chair position by a shoulder surgeon (MMK). The shoulder joint condition, rotator cuff level, and tendon lesions of the two arms were observed in both groups through a lateral portal. After arthroscopic cuff repair, LHBT tenodesis was performed by passing an anchor suture thread (Arthrex, Naples, FL, USA) through the LHBT in an intra-articular manner and attaching it to the greater humeral tuberosity. In group 1, the PELHBT adhesion site to the superior glenoid was detached using a biter; this was not conducted in group 2.
Post-surgical rehabilitation followed the same protocol in both groups. In the first 6 weeks after surgery, a sling was used with an abduction pad. Active elbow flexion and extension were allowed, but terminal extension was prohibited. Passive external rotation was started from the day after surgery and continued as far as the patient felt comfortable. Overhead flexion was prohibited for 6 weeks to prevent any damage to the repaired site. After 6 weeks, the sling was removed, and overhead flexion was started by a rope and pulley. Strengthening of the isotonic muscles stabilizing the rotator cuff, deltoid, and scapula was started 10 to 12 weeks after surgery and continued for 6 months. Complex hand movements and overhead functions were allowed after strengthening the muscles for 6 to 10 months after surgery.
In this study, independent t-test compared quantitative variables such as age and VAS, SST, MMT grading system, and CS scores in the two groups (distribution of quantitative variables was assessed by Shapiro-Wilk and Q-Q plot; all variables had a normal distribution). Meanwhile, the chi-square test was used to compare the qualitative variables (sex, dominant hand, involved shoulder, history of trauma, and follow-up period) in the two groups. Repeated measures analysis of variance was performed to study the changes in scores within the measurement intervals at a significance level of p<0.05. All data were analyzed using IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA).
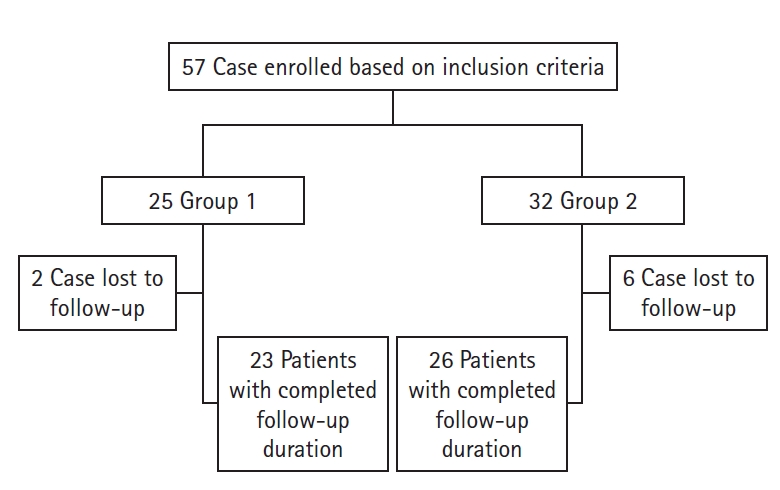
Among the 57 studied patients after tenodesis, 25 were members of group 1 and 32 were members of group 2. Two patients of group 1 and six patients of group 2 were excluded from the study due to follow-up loss. Finally, 23 and 26 patients were included in groups 1 and 2, respectively (Fig. 1).
In general, the mean┬▒standard deviation of patient age was 58.04┬▒4.09 years (range, 48ŌĆō66 years), 29 patients (59.2%) were male, and 20 (40.8%) were female. Table 1 presents the patient demographic information and radiological findings, showing no significant difference between the two groups in any characteristics.
The results of the two groups in the three measurement intervals showed that the shoulder function (CS, SST), satisfaction rate with shoulder function (VAS), and biceps muscle strength (MMT) improved over time, and pain severity (VAS) decreased significantly (p<0.05). However, these changes were not significant upon comparison of the two groups in the evaluation intervals (p>0.05) (Table 2). No post-surgical complication (infection, bleeding, auxiliary nerve injury, and deltoid muscle detachment) was observed in the two groups.
Our findings showed that both groups improved in terms of shoulder function and biceps muscle strength scores. Also, previous studies showed that tenodesis with and without detachment of the PELHBT can improve the final treatment results [10,13,14]. This finding is consistent with our results. Therefore, it seems that both methods can provide acceptable results over time. Comparison of the results between the two groups did not show any significant difference. Ko et al. [15] showed no difference in final short-term result of tenodesis with or without detachment of the PELHBT from the supraglenoid tubercle. This finding is consistent with our results. Franceschi et al. [16] reported similar findings to our study, suggesting no difference between the two groups in terms of shoulder function at 4 years of follow-up. In our study, the outcomes of surgery in both groups were investigated in the long- and short-term. In the two studies mentioned, Ko et al. [15] and Franceschi et al. [16], shoulder function was assessed by University of California at Los Angeles; in our study, shoulder function was assessed by CS and SST. Furthermore, in our study, shoulder satisfaction and biceps muscle strength were evaluated for the first time.
Neither group reported post-surgical complication, consistent with Franceschi et al. [16]. Regarding the results of this and other studies, treatment with or without PELHBT detachment does not cause any complication or risk for patients.
Although the results of treatment with or without PELHBT detachment did not cause any difference in shoulder function, biceps muscle strength, pain, or satisfaction rate, previous studies have suggested the use of the PELHBT as a graft for blood carriage to a hypovascular area of the rotator cuff, providing labral strings of the suprascapular artery supply blood for the LHBT [17]. Also, anatomical studies have shown that the LHBT has a major role in glenohumeral stability [18].
It has been shown experimentally and clinically that the PELHBT can increase the torsional rigidity of the glenohumeral joint and function as a dynamic anterior and posterior stabilizer [11,19-21]. Kuhn et al. [22] have shown that the PELHBT plays a major role in restraining dynamic external rotation in the abducted shoulder. Kumar et al. [23] have reported that PELHBT detachment leads to instability and dysfunction of the glenohumeral joint and significant upward migration of the head of the humerus. Although the PELHBT plays a major role in shoulder dynamism and stability, the results of our and other studies [15,16] have shown that detachment of the PELHBT from the supraglenoid tubercle with biceps tenodesis to the greater tuberosity of humerus tuberosity does not have any effect on the final result. In other words, treatment with or without PELHBT detachment from the glenoid adhesion site causes no complication. Therefore, detachment of this tendon is not necessary. However, in our study, the patients were 48ŌĆō66 years old and did not perform regular exercise. In two similar studies, the patients were older than 40 years and also were not professional athletes [15,16]. Based on activity intensity, it is possible that lack of statistical difference between patient satisfaction rate in this study is related to lack of regular exercise. Therefore, it is important to note that detachment of the PELHBT from the glenoid site can affect the activity and return to exercise of professional athletes who more frequently use their shoulder muscles, causing instability of the shoulder joint and disturbances in dynamics, especially in longer follow-up. Thus, we suggest conducting a subsequent study involving athletes with RCT and LHBT pathologies.
In general, there are few studies in this area. We studied patients in short- and long-term periods, though the small sample size was one of the constraints of this study. The probability that PELHBT detachment can prevent superior migration of the humeral head should be validated in long-term investigation. As other factors are involved in improvement of shoulder function, including age, underlying diseases especially diabetes, and nutrition status, additional studies are recommended to investigate these factors.
There was no difference between the final outcomes of tenodesis with or without detachment of the PELHBT from the supraglenoid tubercle. Therefore, it seems that tendon detachment is not necessary.
NOTES
Table┬Ā1.
Demographic characteristics and pretreatment findings
Table┬Ā2.
Functional outcome scores
REFERENCES
1. Gill TJ, McIrvin E, Mair SD, Hawkins RJ. Results of biceps tenotomy for treatment of pathology of the long head of the biceps brachii. J Shoulder Elbow Surg 2001;10:247ŌĆō9.


2. Chen CH, Hsu KY, Chen WJ, Shih CH. Incidence and severity of biceps long head tendon lesion in patients with complete rotator cuff tears. J Trauma 2005;58:1189ŌĆō93.


3. Burkhead WZ. The biceps tendon. In: Rockwood CA, Matsen FA, Wirth MA, Lippitt SB, eds. The shoulder. 4th ed. Philadelphia, PA: Saunders; 2009. p. 791ŌĆō836.
4. Checchia SL, Doneux PS, Miyazaki AN, et al. Biceps tenodesis associated with arthroscopic repair of rotator cuff tears. J Shoulder Elbow Surg 2005;14:138ŌĆō44.


5. McDonald LS, Dewing CB, Shupe PG, Provencher MT. Disorders of the proximal and distal aspects of the biceps muscle. J Bone Joint Surg Am 2013;95:1235ŌĆō45.


6. Wittstein JR, Queen R, Abbey A, Toth A, Moorman CT 3rd. Isokinetic strength, endurance, and subjective outcomes after biceps tenotomy versus tenodesis: a postoperative study. Am J Sports Med 2011;39:857ŌĆō65.


7. Murthi AM, Vosburgh CL, Neviaser TJ. The incidence of pathologic changes of the long head of the biceps tendon. J Shoulder Elbow Surg 2000;9:382ŌĆō5.


8. Ozalay M, Akpinar S, Karaeminogullari O, et al. Mechanical strength of four different biceps tenodesis techniques. Arthroscopy 2005;21:992ŌĆō8.


9. Zhang Q, Zhou J, Ge H, Cheng B. Tenotomy or tenodesis for long head biceps lesions in shoulders with reparable rotator cuff tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc 2015;23:464ŌĆō9.


10. Kandeel AA. Is it a must to tenotomize the biceps intraarticular origin during tenodesis? A prospective case series study of biceps tenodesis without tenotomy. Curr Orthop Pract 2021;32:161ŌĆō8.

11. Warner JJ, McMahon PJ. The role of the long head of the biceps brachii in superior stability of the glenohumeral joint. J Bone Joint Surg Am 1995;77:366ŌĆō72.


12. Landin D, Thompson M, Jackson MR. Actions of the Biceps Brachii at the Shoulder: A Review. J Clin Med Res 2017;9:667ŌĆō70.



14. Snir N, Hamula M, Wolfson T, Laible C, Sherman O. Long head of the biceps tenodesis with cortical button technique. Arthrosc Tech 2013;2:e95ŌĆō7.



15. Ko SH, Jung KH, Kang HK. Comparison of clinical outcomes of arthroscopic biceps long head tenodesis with or without tenotomy. Arthrosc Orthop Sports Med 2015;2:23ŌĆō9.

16. Franceschi F, Longo UG, Ruzzini L, Papalia R, Rizzello G, Denaro V. To detach the long head of the biceps tendon after tenodesis or not: outcome analysis at the 4-year follow-up of two different techniques. Int Orthop 2007;31:537ŌĆō45.


17. Wolfgang GL. Surgical repair of tears of the rotator cuff of the shoulder: factors influencing the result. J Bone Joint Surg Am 1974;56:14ŌĆō26.

18. Elser F, Braun S, Dewing CB, Giphart JE, Millett PJ. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy 2011;27:581ŌĆō92.


19. Itoi E, Newman SR, Kuechle DK, Morrey BF, An KN. Dynamic anterior stabilisers of the shoulder with the arm in abduction. J Bone Joint Surg Br 1994;76:834ŌĆō6.


20. Rodosky MW, Harner CD, Fu FH. The role of the long head of the biceps muscle and superior glenoid labrum in anterior stability of the shoulder. Am J Sports Med 1994;22:121ŌĆō30.


21. Blasier RB, Soslowsky LJ, Malicky DM, Palmer ML. Posterior glenohumeral subluxation: active and passive stabilization in a biomechanical model. J Bone Joint Surg Am 1997;79:433ŌĆō40.

- TOOLS