1. Fehringer EV, Sun J, VanOeveren LS, Keller BK, Matsen FA 3rd. Full-thickness rotator cuff tear prevalence and correlation with function and co-morbidities in patients sixty-five years and older. J Shoulder Elbow Surg 2008;17(6):881–5.


2. Silver MD, Daigneault JP. Symptomatic interarticular migration of glenoid suture anchors. Arthroscopy 2000;16(1):102–5.


3. Gaenslen ES, Satterlee CC, Hinson GW. Magnetic resonance imaging for evaluation of failed repairs of the rotator cuff. Relationship to operative findings. J Bone Joint Surg Am 1996;78(9):1391–6.


4. Benson EC, MacDermid JC, Drosdowech DS, Athwal GS. The incidence of early metallic suture anchor pullout after arthroscopic rotator cuff repair. Arthroscopy 2010;26(3):310–5.


5. Barber FA, Snyder SJ, Abrams JS, Fanelli GC, Savoie FH 3rd. Arthroscopic Bankart reconstruction with a bioabsorbable anchor. J Shoulder Elbow Surg 2003;12(6):535–8.


6. Athwal GS, Shridharani SM, O’Driscoll SW. Osteolysis and arthropathy of the shoulder after use of bioabsorbable knotless suture anchors. A report of four cases. J Bone Joint Surg Am 2006;88(8):1840–5.

7. Freehill MQ, Harms DJ, Huber SM, Atlihan D, Buss DD. Poly-L-lactic acid tack synovitis after arthroscopic stabilization of the shoulder. Am J Sports Med 2003;31(5):643–7.


8. Kelly JD 2nd. Disintegration of an absorbable rotator cuff anchor six weeks after implantation. Arthroscopy 2005;21(4):495–7.


9. Mastrokalos DS, Paessler HH. Allergic reaction to biodegradable interference poly-L-lactic acid screws after anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft. Arthroscopy 2008;24(6):732–3.


10. Speer KP, Warren RF, Pagnani M, Warner JJ. An arthroscopic technique for anterior stabilization of the shoulder with a bioabsorbable tack. J Bone Joint Surg Am 1996;78(12):1801–7.


12. Suchenski M, McCarthy MB, Chowaniec D, et al. Material properties and composition of soft-tissue fixation. Arthroscopy 2010;26(6):821–31.


13. Nho SJ, Provencher MT, Seroyer ST, Romeo AA. Bioabsorbable anchors in glenohumeral shoulder surgery. Arthroscopy 2009;25(7):788–93.


14. Barber FA, Dockery WD, Cowden CH 3rd. The degradation outcome of biocomposite suture anchors made from poly L-lactide-co-glycolide and β-tricalcium phosphate. Arthroscopy 2013;29(11):1834–9.


15. Kim SH, Kim DY, Kwon JE, Park JS, Oh JH. Perianchor cyst formation around biocomposite biodegradable suture anchors after rotator cuff repair. Am J Sports Med 2015;43(12):2907–12.


16. Randelli P, Compagnoni R, Aliprandi A, et al. Long-term degradation of poly-lactic co-glycolide/β-tricalcium phosphate biocomposite anchors in arthroscopic bankart repair: a prospective study. Arthroscopy 2014;30(2):165–71.


17. Yang IC, Kim SY, Kang HC, Lee HY, Kwon JY, Kim SM. A study on evaluation of bioabsorbable anchor (PLGA+β-TCP) through mechanical test under moisture difference. J Med Devices 2016;10(3):1–2.
18. Chung SW, Kim JY, Kim MH, Kim SH, Oh JH. Arthroscopic repair of massive rotator cuff tears: outcome and analysis of factors associated with healing failure or poor postoperative function. Am J Sports Med 2013;41(7):1674–83.


19. Aziz SR. The division of oral and maxillofacial surgery at columbia presbyterian medical center: a.k.a. HSDM South. Harv Dent Bull 1999;8(1):26–8.

20. DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am 1984;66(4):563–7.


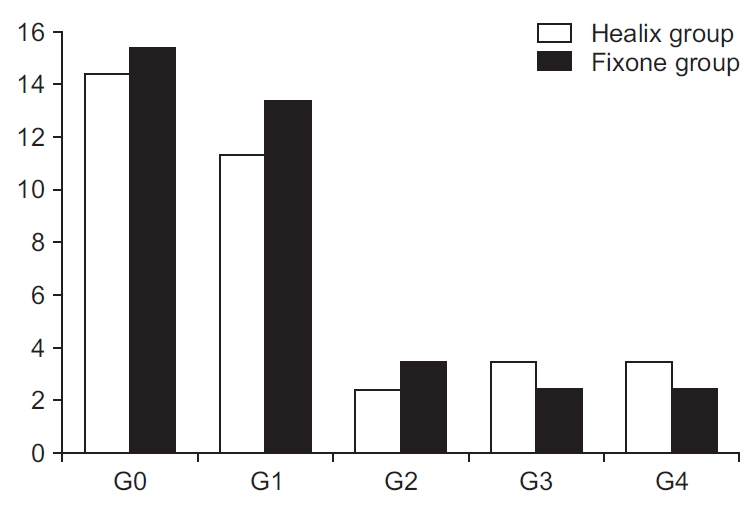
21. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994;(304):78–83.

22. Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg 1999;8(6):599–605.


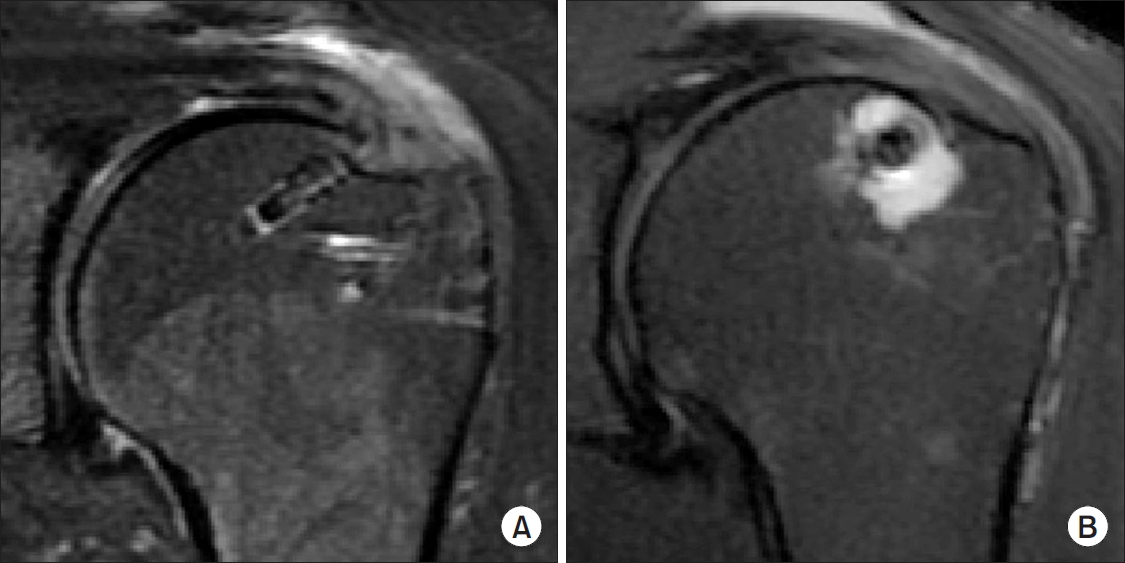
23. Kim SH, Oh JH, Lee OS, Lee HR, Hargens AR. Postoperative imaging of bioabsorbable anchors in rotator cuff repair. Am J Sports Med 2014;42(3):552–7.


24. Uhthoff HK, Seki M, Backman DS, Trudel G, Himori K, Sano H. Tensile strength of the supraspinatus after reimplantation into a bony trough: an experimental study in rabbits. J Shoulder Elbow Surg 2002;11(5):504–9.


25. Cho NS, Yi JW, Lee BG, Rhee YG. Retear patterns after arthroscopic rotator cuff repair: single-row versus suture bridge technique. Am J Sports Med 2010;38(4):664–71.


26. Glueck D, Wilson TC, Johnson DL. Extensive osteolysis after rotator cuff repair with a bioabsorbable suture anchor: a case report. Am J Sports Med 2005;33(5):742–4.


28. Magee T, Shapiro M, Hewell G, Williams D. Complications of rotator cuff surgery in which bioabsorbable anchors are used. AJR Am J Roentgenol 2003;181(5):1227–31.


29. Barber FA, Spenciner DB, Bhattacharyya S, Miller LE. Biocomposite implants composed of poly(Lactide-co-Glycolide)/β-tricalcium phosphate: systematic review of imaging, complication, and performance outcomes. Arthroscopy 2017;33(3):683–9.