|
 |
- Search
| Clin Shoulder Elb > Volume 27(1); 2024 > Article |
|
Abstract
Background
Deficiency in scapular muscle endurance (SME) is a risk factor for rotator-cuff-related shoulder pain (RCRSP). However, the exact relationship among SME, pain, and functionality remains unclear. This study aims to compare SME, pain, and functionality in RCRSP patients to those in age-sex-matched healthy controls.
Methods
Twenty-three patients with RCRSP and 23 age-sex matched healthy controls were included in the study. SME was measured using a 1-kg dynamometer. Self-reported pain level was assessed using a visual analog scale. The Functional Impairment Test-Hand, Neck, Shoulder, and Arm (FIT-HaNSA) was also used to assess functional impairment.
Shoulder pain is the third most commonly reported musculoskeletal condition in the general population, after only back and knee pain, with 18%–26% of individuals experiencing it at least once in their lives [1]. Disorders of the rotator cuff constitute 70% of all shoulder pain diagnoses [2]. Symptoms associated with the rotator cuff and related tissues (shoulder impingement syndrome, rotator cuff tendinopathy, and rotator cuff tears) have been defined as rotator-cuff-related shoulder pain (RCRSP). RCRSP refers to the clinical presentation of pain and impairment of shoulder movement and function usually experienced during elevation [2-4]. Although consensus is needed to define appropriate terminology, terms like subacromial, rotator cuff pain syndrome, or RCRSP are useful [3].
Genetic factors, hormonal changes, habits such as smoking and alcohol consumption, biochemical and sensory-motor cortex changes, psychological factors, and biomechanical changes are possible causes of RCRSP [5]. Although RCRSP is most likely multifaceted, one of the major reported causes is decrease of the subacromial space and compaction of the subacromial soft tissues [5,6]. A loss of coordination between the rotator cuff and scapular muscles decreases shoulder neuromuscular control, which may explain population-level increases in shoulder joint narrowing and limited range of motion (ROM) [7].
The scapula and scapular muscles (trapezius and middle and lower serratus anterior) are the essential parts of scapular stabilization and glenohumeral joint movements, as these are the links along the kinetic chain that allow a proximal-to-distal distraction energy transfer in the upper extremity [8,9]. Simultaneously fatiguing these scapular muscles may affect the shoulder's normal kinematics, reducing the subacromial space and subsequently increasing the risk of RCRSP [9,10]. Thus, evaluation of scapular muscle endurance (SME) should be a crucial part of examining RCRSP patients.
Although no standard procedure exists, isometric [11-14] and isokinetic tests [15,16] are performed to provide a general idea of SME. Evaluation of the isolated endurance of the scapular muscles by objective tests is clinically challenging, and factors such as regional anatomy, patient positioning, and severe pain during evaluation make SME evaluation difficult. The number of studies on this topic in the literature is limited [11-16]. To our knowledge, no studies have evaluated SME in patients with RCRSP.
Therefore, we aimed to compare SME and function in patients with RCRSP to age- and gender-matched healthy controls. Our second aim was to examine the correlation between SME, pain, and shoulder function in RCRSP patients. We hypothesized that patients with RCRSP would exhibit decreased SME and upper extremity function compared with healthy controls. Also, we hypothesized that low SME scores would be associated with pain and functional impairment in patients with RCRSP.
This study was approved by Research Ethics Committee of Gazi University (No. 25901600-577) and registered in ClinicalTrials.gov (NCT03XXX). Informed consent was obtained from all patients participating in the study, and signed publication approvals were acquired from those patients whose photographs are featured in Fig. 1.
Initially, 89 patients were evaluated. Sixty-six patients did not fit the inclusion criteria, leaving 23 patients (13 males and 10 females; mean age, 48.5 years; standard deviation [SD], 10.3 years) included in the study. For comparison, an age-matched group of 23 healthy individuals (13 males, 10 females) with a mean age of 48 years (SD, 10.5 years), no history of shoulder surgery for labral or rotator cuff pathology, and no complaints of elbow or shoulder pain that limited or restricted recent participation served as a control group. All evaluations for each participant were performed by the same investigator at the same time of day and in one session.
Clinical examination, patient self-report, ROM (shoulder flexion, abduction, external rotation, and internal rotation), and magnetic resonance imaging (MRI) were used to diagnose RCRSP. Patients with RCRSP must have a history of nontraumatic onset of shoulder discomfort and pain on examining the rotator cuff tendons. Involvement and retraction of the rotator cuff tendons were assessed with standard, non-contrast coronal, axial, and sagittal MRI sequences, as described by Boileau et al. [17]. Clinical and MRI evaluations (tendinosis, subacromial effusion, partial rotator cuff tear, and calcific tendinitis) were performed by an orthopedic surgeon with 20 years of experience.
The study inclusion criteria were: (1) positive sign in two or more specific shoulder clinical tests (Neer, Hawkins, painful arc, Lag sign, Jobe, drop-arm, and Gerber lift-off); (2) findings of RCRSP on MRI; (3) at least 120° of shoulder flexion, 25° of abduction, and 30° of external rotation; (4) right arm dominance; and (5) no surgical history in the shoulder area. Patients with shoulder pathology other than RCRSP, such as glenohumeral instability, acromioclavicular joint osteoarthritis, bicipital tendon lesions, adhesive capsulitis, glenohumeral osteoarthritis, shoulder or cervical surgery history, or bilateral shoulder complaints; neurological diseases; pregnancy; and those who underwent shoulder-related physiotherapy were excluded.
Edmondston et al. [18] developed the SME test, which is based on an exercise designed to improve the activity of the serratus anterior and trapezius muscles. Patients stood against the wall with their shoulders and elbows extended to 90° during the test. While both scapulae were in a neutral position, an 18–36-cm stick was placed between the elbows, and the patients were instructed to hold the dynamometer (Feta 137 F0202 1 kg/10 N) between their hands. The participants were asked to externally rotate their shoulders until the dynamometer read 1 kg load capacity and to maintain this position (Fig. 1A) [13,14]. The test was continued until the participants' 90° shoulder flexion movement was disrupted due to major pain and the stick dropped. The test was performed twice (with 60 seconds of rest between tests), and the average results were recorded in seconds. Immediately after completion of the tests, patient pain intensity was measured, and the averages were recorded.
Pain intensity was assessed on a 100-mm visual analog scale (VAS) according to pain during activity, nighttime, and after SME and Functional Impairment Test-Hand, Neck, Shoulder, and Arm (FIT-HaNSA) testing (0=no pain, 10=excruciatingly painful) [19].
The FIT-HaNSA protocol, developed by MacDermid et al. [20], was used to evaluate the functional performance of the upper extremities when performing activity in three phases. In phase 1, a shelf was put in at waist height, with a second shelf 25 cm above it. The patient used the injured arm to lift three containers, one at a time, from one shelf to the other at a rate of 60 beats per minute, as regulated by a metronome (Fig. 1B). In phase 2, a shelf was placed at the patient's eye level, and the other was 25 cm below it. Patients were asked to raise three containers between shelves at a rate of 60 beats per minute (Fig. 1C). In phase 3, a shelf with an attachable plate perpendicular was positioned at the subject's eye level. Subjects were required to repeatedly screw and unscrew bolts into the plate in a pattern (Fig. 1D). The rest period after each test was 30 seconds. Subjects were instructed to perform each phase for five minutes or until a stop criterion was met. In cases of extreme pain, when patients used the torso or whole body instead of limbs for five consecutive repetitions, when they had difficulty following the metronome, in cases with the possibility of injury, or upon patient choice, the test was terminated. Results were recorded in seconds for each phase. A total score was calculated by averaging the recorded time for the three phases [21]. During the measurements, a wooden material of the same size as the original equipment, developed by the Job Sim System (JTECH Medical), was used [20,21]. The severity of pain felt immediately after the end of the test was recorded according to VAS.
Data were analyzed using IBM SPSS 22.0 (IBM Corp.). Normal distribution of the data was verified with the Kolmogorov-Smirnov test and visual inspection of the histograms. Independent t-tests (for normally distributed) and Mann-Whitney U-tests (for non-normally distributed) were used to compare the two matched groups. Chi-square tests were applied for categorical data. Mean differences and 95% confidence intervals (CIs) were calculated as additional parameters. The Pearson correlation coefficient was applied to assess the hypothesized relationship among SME, pain, and function. Correlations were considered weak for values between 0.3–0.49, moderate for values between 0.5–0.74, and strong for values greater than 0.75 [22,23]. The criterion for statistical significance was set at P<0.05.
In a post-hoc power analysis performed with G*Power software (version 3.1.9.4), based on the difference between group SME scores, the study power was estimated to be 85% with an effect size of 0.48 and a type-1 error rate of 0.05. Thus, we determined that the sample sizes of the RCRSP (n=23) and control (n=23) groups were sufficient.
While there was no significant difference in demographic data (age, body mass index, sex, tested side) between the groups (P>0.05), there was a significant difference in ROM values between the two groups (P<0.05) (Table 1). Matched controls had significantly higher SME scores than patients with RCRSP (95% CI, –47.86 to –17.73; P<0.001) (Table 2). Comparisons between the RCRSP and matched control groups for the FIT-HaNSA scores are listed in Table 2. Patients with RCRSP also had lower waist level (phase 1: 95% CI, –159.09 to –76.64; P<0.001), shoulder level (phase 2: 95% CI, –135.72 to –54.53; P<0.001), eye level (phase 3: 95% CI, –155.53 to –70.46; P<0.001), and total functionality level (95% CI, –147.52 to –69.43; P<0.001) compared with controls (Table 2).
In the RCRSP group, SME was strongly correlated with activity pain (r: –0.775, P=0.000) and FIT-HaNSA scores (phase 1: r=0.933, P=0.000), (phase 2: r=0.961, P=0.000), (phase 3: r=0.967, P=0.000), (total score: r=0.968, P=0.000) and was moderately correlated with night pain (r=–0.523, P=0.010), SME measurement pain (r=–0.587, P=0.003), and FIT-HaNSA measurement pain (r=–0.643, P=0.001). Additionally, SME was weakly correlated with FIT-HaNSA phase 2 (r=0.443, P=0.034), phase 3 (r=0.384, P=0.070), and total score (r=0.470, P=0.024) in the matched-healthy group (Table 3).
The most important finding of this study was that, compared with healthy controls, patients with RCRSP had lower SME and functional scores, and SME was associated with varying degrees of pain intensity and upper-extremity function. The results strongly supported our hypotheses. SME weakness may be a mechanism for shoulder diseases by changing scapular movements and requiring compensation by other shoulder muscles [24]. In this respect, determination of SMEs can provide additional information at the clinical decision-making stage; however, the research on SMEs consists of studies carried out on healthy people and textile workers with painful shoulders [12-16]. The isometric SME evaluation method was used in this study, and it was found valid and reliable by Edmondston et al. [18]. Before deciding on the SME test protocol, a preliminary study was performed (including 10 patients and unpublished data), and the protocol developed by [18] was preferred because the patients could not perform the other test position [11,12], which required 135° abduction, due to pain. To the best of our knowledge, this is the only study that evaluates SMEs in patients with RCRSP.
Eraslan et al. [14] evaluated SMEs using the method that was used in this study and found that SME was significantly lower in textile workers with painful shoulders (41.02 seconds) than that in healthy workers (61.49 seconds). In a study performed by Cools et al. [15], among professional athletes and sedentary individuals, SME was measured with an isokinetic dynamometer, and, although the fatigue index of athletes (19.9%) was less than that of sedentary individuals (26.3%), there was no statistically significant difference between the two groups. In another study that assessed SME with the same method, SME was statistically significant in patients with lateral epicondylitis (54 seconds) compared with healthy individuals (85 seconds) [11]. This study recorded the lowest SME scores for a patient group (36.95 seconds) and the highest for a control group (69.76 seconds). We think that the different study results are due to differences in measurement, patient diagnosis, and study methodology.
Muscle endurance was identified as a risk factor for musculoskeletal pain [25]. Because shoulder kinematics are greatly affected by the surrounding muscles, fatigue in any of them might result in a change in the scapulohumeral rhythm. Impairment in scapulohumeral rhythm is likely to cause rotator cuff pathologies and pain [26]. A literature investigation found that studies mostly analyzed the relationship between the endurance of the muscles surrounding the shoulders and pain [27-29]. In the only study investigating shoulder pain and SME, no correlations were reported between these two variables [15]. In contrast, varying degrees of correlations were found between SME and activity (strong), night, and SME/FIT-HaNSA measurement pain (moderate) in the patient group in this study. These results are thought to be related to the SME test protocol, which requires long-term static contraction activity, such as shoulder flexion and external rotation. Additionally, the presence of pain is one of the most critical factors affecting test results (SME/FIT-HaNSA), and the most common reason for test termination in the patient group in our study was pain.
Shoulder function requires coordinated, continuous muscular activity that both maintains adequate proximal control and allows a wide range of pain-free movement to complete daily tasks [21]. Scapular muscle weakness, in particular, can result in early fatigue, insufficient scapular stability, and functional deficits [25,30]. However, no previous study has objectively evaluated the functional impairments caused by scapular muscle weakness. In this study, a positive and strong relationship between SME and RCRSP and a positive and weak relationship between SME and FIT-HaNSA (phase 1, phase 2, phase 3, total) were found in all groups.
This study has some limitations that should be considered when interpreting the data. First, some patients with RCRSP could not be included due to their failure to meet the test criteria, which limited the patient group. Second, because the patients had pain, it is possible that pain was a central driving factor for endurance, muscle strength, and function measures. These are reasonable directions for future research in this area.
Increases in SME may reduce pain and improve upper-extremity functionality in patients with RCRSP. SME assessment is recommended in patients with RCRSP to provide clinicians with objective information to guide clinical decision-making. Future studies should investigate the short- and long-term efficacy of treating SME deficits as part of a comprehensive program for patients with RCRSP.
NOTES
Fig. 1.
(A) Scapular muscle endurance test. (B) Functional Impairment Test-Hand, Neck, Shoulder, and Arm (FIT-HaNSA) phase 1. (C) FIT-HaNSA phase 2. (D) FIT-HaNSA phase 3.
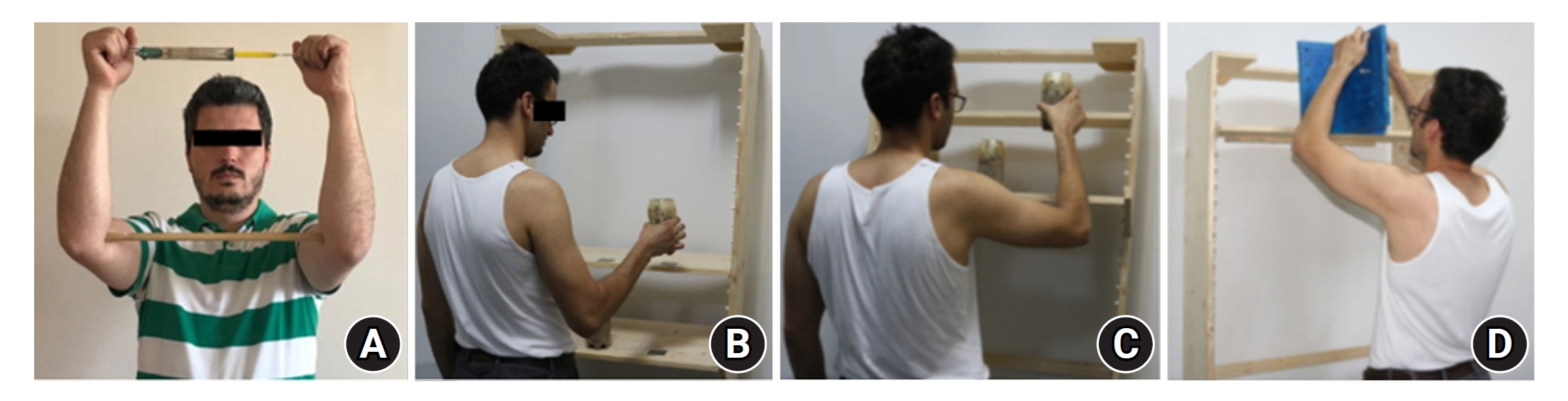
Table 1.
Demographic and clinical characteristics of the patients
| Variable | RCRSP (n=23) | Control (n=23) | 95% CI | P-value |
|---|---|---|---|---|
| Age (yr) | 49±10 | 48±11 | –5.63 to 6.67 | 0.865* |
| Body mass index (kg/m2) | 29.3±4.9 | 28.1±2.6 | –1.16 to 3.55 | 0.314* |
| Sex (female:male) | 10:13 | 10:13 | - | 1.000† |
| Tested side (affected side) | 0.753† | |||
| Right | 16 | 15 | - | |
| Left | 7 | 8 | - | |
| Range of motion (°) | ||||
| Flexion | 148.3±19.1 | 178.9±2.4 | –38.6 to –22.5 | 0.001* |
| Abduction | 117.3±26.9 | 179.2±2.2 | –73.3 to –50.5 | 0.001* |
| External rotation | 59.30±19.9 | 78.9±12.3 | –29.5 to –9.8 | 0.001* |
| Internal rotation | 58.7±20.4 | 84.3±10.2 | –35.2 to –15.3 | 0.001* |
| MRI lesion (positive:negative) | - | |||
| Subacromial-subdeltoid effusion | 10:13 | NA | - | - |
| Supraspinatus tendinosis | 17:6 | NA | - | - |
| Supraspinatus partial tear | 13:10 | NA | - | - |
| Calcific tendinitis in supraspinatus | 2:21 | NA | - | - |
| Infraspinatus tendinosis | 3:20 | NA | - | - |
| Infraspinatus partial tear | 1:22 | NA | - | - |
| Teres minor tendinosis | 0:23 | NA | - | - |
| Teres minor partial tear | 0:23 | NA | - | - |
| Subscapularis tendinosis | 4:19 | NA | - | - |
| Subscapularis partial tear | 0:23 | NA | - | - |
| Shoulder clinical tests (positive:negative) | ||||
| Hawkins test | 21:2 | 0:23 | - | - |
| Neer test | 18:5 | 0:23 | - | - |
| Painful arc test | 13:10 | 0:23 | - | - |
| Jobe test | 13:10 | 0:23 | - | - |
| Drop-arm test | 0:23 | 0:23 | - | - |
| Lag sign test | 2:21 | 0:23 | - | - |
| Gerber lift-off test | 3:20 | 0:23 | - | - |
Table 2.
Descriptive scores of SME pain and FIT-HaNSA
| Variable | RCRSP (n=23) | Control (n=23) | 95% CI | P-value* |
|---|---|---|---|---|
| SME (sec) | 28.0 (24.5–55.0) | 61.5 (54.0–69.0) | –47.86 to –17.73 | <0.001 |
| Pain intensity (VAS) | ||||
| Activity | 5.0±1.8 | - | - | - |
| Night | 5.4±1.9 | - | - | - |
| After SME | 4.9±1.5 | - | - | - |
| After FIT-HaNSA | 4.5±1.2 | - | - | - |
| FIT-HaNSA (sec) | ||||
| Task 1 | 124.0 (94.0–300.0) | 300.0 (300.0–300.0) | –159.09 to –76.64 | <0.001 |
| Task 2 | 98.0 (60.0–189.0) | 221.0 (180.0–273.0) | –135.72 to –54.53 | <0.001 |
| Task 3 | 111.0 (80.0–271.0) | 289.0 (253.0–300.0) | –155.53 to –70.46 | <0.001 |
| Total score | 114.0 (76.6–260.6) | 271.0 (244.0–291.0) | –147.52 to –69.43 | <0.001 |
Table 3.
Correlation between SME test scores, pain intensity, and FIT-HaNSA
REFERENCES
1. Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis 1998;57:649–55.



2. Smythe A, Rathi S, Pavlova N, et al. Self-reported management among people with rotator cuff related shoulder pain: an observational study. Musculoskelet Sci Pract 2021;51:102305.


3. Lewis J. Rotator cuff related shoulder pain: assessment, management and uncertainties. Man Ther 2016;23:57–68.


4. Dehqan B, Delkhoush CT, Mirmohammadkhani M, Ehsani F. Does forward head posture change subacromial space in active or passive arm elevation. J Man Manip Ther 2021;29:227–34.


5. de Oliveira FC, Bouyer LJ, Ager AL, Roy JS. Electromyographic analysis of rotator cuff muscles in patients with rotator cuff tendinopathy: a systematic review. J Electromyogr Kinesiol 2017;35:100–14.


6. McClure PW, Michener LA, Karduna AR. Shoulder function and 3-dimensional scapular kinematics in people with and without shoulder impingement syndrome. Phys Ther 2006;86:1075–90.


7. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part III: the SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy 2003;19:641–61.


8. Hsu JE, Hulet DA, McDonald C, Whitson A, Russ SM, Matsen FA. The contribution of the scapula to active shoulder motion and self-assessed function in three hundred and fifty two patients prior to elective shoulder surgery. Int Orthop 2018;42:2645–51.


9. Chopp-Hurley JN, O'Neill JM, McDonald AC, Maciukiewicz JM, Dickerson CR. Fatigue-induced glenohumeral and scapulothoracic kinematic variability: implications for subacromial space reduction. J Electromyogr Kinesiol 2016;29:55–63.


10. Harrison N, Garrett WZ, Timmons MK. Serratus anterior fatigue reduces scapular posterior tilt and external rotation during arm elevation. J Sport Rehabil 2021;30:1151–7.


11. Day JM, Bush H, Nitz AJ, Uhl TL. Scapular muscle performance in individuals with lateral epicondylalgia. J Orthop Sports Phys Ther 2015;45:414–24.


12. Day JM, Bush H, Nitz AJ, Uhl TL. Arm dominance does not influence measures of scapular muscle strength and endurance in healthy individuals. Physiother Pract Res 2015;36:87–95.

13. Hazar Kanik Z, Pala OO, Gunaydin G, et al. Relationship between scapular muscle and core endurance in healthy subjects. J Back Musculoskelet Rehabil 2017;30:811–7.


14. Eraslan U, Gelecek N, Genc A. Effect of scapular muscle endurance on chronic shoulder pain in textile workers. J Back Musculoskelet Rehabil 2013;26:25–31.


15. Cools AM, Geerooms E, Van den Berghe DF, Cambier DC, Witvrouw EE. Isokinetic scapular muscle performance in young elite gymnasts. J Athl Train 2007;42:458–63.


16. Van de Velde A, De Mey K, Maenhout A, Calders P, Cools AM. Scapular-muscle performance: two training programs in adolescent swimmers. J Athl Train 2011;46:160–9.



17. Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal. J Bone Joint Surg Am 2005;87:1229–40.


18. Edmondston SJ, Wallumrød ME, Macléid F, Kvamme LS, Joebges S, Brabham GC. Reliability of isometric muscle endurance tests in subjects with postural neck pain. J Manipulative Physiol Ther 2008;31:348–54.


19. Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 1983;17:45–56.


20. MacDermid JC, Ghobrial M, Quirion KB, et al. Validation of a new test that assesses functional performance of the upper extremity and neck (FIT-HaNSA) in patients with shoulder pathology. BMC Musculoskelet Disord 2007;8:42.



21. Kumta P, MacDermid JC, Mehta SP, Stratford PW. The FIT-HaNSA demonstrates reliability and convergent validity of functional performance in patients with shoulder disorders. J Orthop Sports Phys Ther 2012;42:455–64.


22. Cohen J. Statistical power analysis for the behavioral sciences. Routledge; 2013.
23. Portney LG, Watkins MP. Foundations of clinical research: applications to practice. Prentice Hall; 2000.
24. Szucs K, Navalgund A, Borstad JD. Scapular muscle activation and co-activation following a fatigue task. Med Biol Eng Comput 2009;47:487–95.


25. Roy JS, Ma B, Macdermid JC, Woodhouse LJ. Shoulder muscle endurance: the development of a standardized and reliable protocol. Sports Med Arthrosc Rehabil Ther Technol 2011;3:1.



26. McQuade KJ, Dawson J, Smidt GL. Scapulothoracic muscle fatigue associated with alterations in scapulohumeral rhythm kinematics during maximum resistive shoulder elevation. J Orthop Sports Phys Ther 1998;28:74–80.


27. Beach ML, Whitney SL, Dickoff-Hoffman S. Relationship of shoulder flexibility, strength, and endurance to shoulder pain in competitive swimmers. J Orthop Sports Phys Ther 1992;16:262–8.


28. Harrington S, Meisel C, Tate A. A cross-sectional study examining shoulder pain and disability in Division I female swimmers. J Sport Rehabil 2014;23:65–75.