Clinical and Radiological Outcomes of Modified Phemister Operation with Coracoclavicular Ligament Augmentation Using Suture Anchor for Acute Acromioclavicular Joint Dislocation
Article information
Abstract
Background
Modified Phemister operation has been widely used for the treatment of acute acromioclavicular (AC) joint dislocation. Additionally, the use of suture anchor for coracoclavicular (CC) fixation has been reported to provide CC stability. This study was conducted to evaluate the clinical and radiological results of a modified Phemister operation with CC ligament augmentation using suture anchor for acute AC joint dislocation.
Methods
Seventy-four patients underwent the modified Phemister operation with CC ligament augmentation using suture anchor for acute AC joint dislocation and were followed-up for an average of 12.3 months. The visual analogue scale (VAS), range of motion, Constant score, and Korean shoulder scoring system (KSS) were used for clinical assessment. Acromioclavicular interval (ACI), coracoclavicular distance (CCD), and acromioclavicular distance (ACD) were obtained to evaluate the radiological assessments.
Results
At the last follow-up, the mean VAS Score was 1.7 points, the mean joint range of the forward flexion was 164.6°, external rotation at the side was 61.2°, and internal rotation to the posterior was a level of T12. The mean Constant score and the mean KSS was 82.7 points and 84.2 points, respectively. At the mean ACI, CCD, and ACD, significant differences were found preoperatively and at the last follow-up. When the ACI, CCD, and ACD were compared with the contralateral unaffected shoulder at the last follow-up, the affected shoulders had significantly higher values.
Conclusions
The modified Phemister operation with CC ligament augmentation using suture anchor is clinically and radiologically effective at acute AC joint dislocation.
Introduction
Acromioclavicular (AC) joint injuries are common, accounting for 9% to 12% of all shoulder girdle injuries [1,2]. High-grade injuries (Rockwood type IV, V, and VI) of the AC joint are treated surgically, and in the case of type III injuries, indication for surgery is based on the patient’s functional demand [3-5]. Many operative techniques for acute AC joint injury have been developed over the years, including the Phemister [6] or modified Phemister technique [7,8], Bosworth technique [9], Weaver–Dunn technique [10], Wolter plate, conventional hook plate, and locking hook plate fixation [11]. Recently, the arthroscopic reduction technique using Tightrope (Arthrex, Naples, FL, USA) [12,13] has gained popularity. However, there is no ‘gold standard’ technique for surgical treatment of AC joint dislocation [3,5].
Among numerous surgical methods, the relatively simple modified Phemister technique with Kirschner wire (K-wire) is a surgical technique that has commonly been used for the last few decades in acute AC joint dislocation, and many studies have reported clinical results of this technique [14-16]. However, there are several complications associated with this technique owing to the long fixation period of K-wire and it does not solve coracoclavicular ligament injuries [14,17,18].
Recently, the use of suture anchors has been described for the treatment of AC joint injuries. These devices offer the potential advantages of technical ease of use and reduced risk of neurovascular injury, as well as improved pullout strength, which have led to their widespread use in treatment [19,20]. However, only a few studies have reported the clinical and radiologic outcomes of coracoclavicular ligament augmentation using suture anchor devices for treatment of acute AC joint injury [21].
Therefore, this study was conducted to evaluate the clinical and radiological outcomes of modified Phemister operation and additional coracoclavicular ligament augmentation using suture anchors for acute AC joint dislocation. In addition, the clinical and radiological outcomes were evaluated retrospectively. We hypothesized that modified Phemister operation and coracoclavicular ligament augmentation using suture anchors provide satisfactory restoration of shoulder function and radiological outcomes.
Methods
Patient Selection
From July 2007 to March 2018, a consecutive series of 74 patients receiving modified Phemister operation with coracoclavicular ligament augmentation using suture anchor for acute AC joint dislocation were studied retrospectively (Table 1).
Inclusion criteria of patients were (1) radiographically confirmed, acute Rockwood type III or higher AC dislocation (2) underwent surgery within 2 weeks. Exclusion criteria were (1) subacute (more than two weeks since injury) or chronic AC joint dislocation, (2) previous history of surgery on the affected shoulder, (3) concomitant fracture around the ipsilateral shoulder.
A total of 72 males and two females with a mean age of 48.0 years (range, 17–68 years) were included in this study. The mean duration of follow-up from surgery was 12.3 months (range, 8–24 months). According to Rockwood’s classification [22], there were 13 type III lesions (17.6%) and 61 type V lesions (82.4%). All patients underwent surgery within a mean of four days (range, 1–9 days). All patients in our series had coracoclavicular ligament injuries. Patients with type V lesions were immediately addressed to surgical treatment, while indication for surgery for patients with type III lesions was determined based on the patient’s functional demand. All patients were operated on by the same surgeon and provided informed consent to be included in the study.
Surgical Technique
Under general anesthesia, all patients underwent surgery in the 30° beach chair position on an ordinary operating table. A vertical incision was made just lateral to the coracoid along the Langer lines extending from the posterior edge of the AC joint to the coracoid process. The lateral end of the clavicle, the acromion, and the AC joint were exposed. The attachment of the torn coracoclavicular ligament was usually seen at the ‘tip’ of the coracoid process. One suture anchor (Super Revo; Conmed, Largo, FL, USA) was placed into the base of the coracoid process, and the sutures were pulled manually several times to ensure appropriate seating and secure fixation. After the anchor was deployed, two drill holes were made across the bone in the insertion site of the coracoclavicular ligament in the clavicle, and looped wires were passed through the created holes. The clavicle was then reduced by the surgical assistant and confirmed by fluoroscopy. To maintain the obtained reduction, K-wires were trans-articularly inserted through the AC joint under fluoroscopic guidance and bent to prevent forward migration. When a satisfactory reduction was achieved, the joint was stabilized with sutures passing through the created holes and sutures were tied over the clavicle (Fig. 1, 2). Postoperatively, the treated arm was supported with a sling. K-wires were removed at 8 weeks after AC joint stabilization.

Intraoperative radiographs. (A) Suture anchor was fixed at the original site of the coracoclavicular ligament in the coracoid process. (B) Looped wires were passed through the holes created in the insertion site of coracoclavicular ligament in the clavicle. (C) Reduction of acromioclavicular joint with two Kirschner wires transfixation. (D) Sutures were tied over the clavicle and the radiograph shows anatomical reduction of the acromioclavicular joint.

Intraoperatve photographs. (A) The lateral end of the clavicle, the acromion, and the acromioclavicular joint were exposed. (B) The looped wires were passed through the two created holes. (C) One suture anchor was placed into the base of the coracoid process. (D) When a satisfactory reduction and K-wires fixation were achieved, the joint was stabilized with sutures passing through the created holes.
Clinical Assessment
Postoperative clinical evaluations were performed regularly on an outpatient basis (at 4 weeks, 6 weeks, 2 months, and 6 months following surgery and at the last follow-up). The results of the evaluations at the last follow-up were analyzed. At the time of follow-up, all patients were evaluated using the visual analogue scale (VAS) for subjective pain. Postoperative shoulder ranges of motion (ROM), including forward flexion (FF), external rotation at the side (ERs), and internal rotation to the back (IRp) were assessed. The Constant score and Korean shoulder scoring system (KSS) were used for clinical assessments [23,24].
Radiological Assessment
Anteroposterior radiographs of the affected and contralateral unaffected AC joint in neutral rotation made with the patient in a standing position were obtained immediately postoperatively and at each follow-up examination. Acromioclavicular interval (ACI) was defined as the perpendicular distance between the clavicle distal end and acromion, while coracoclavicular distance (CCD) was defined as the perpendicular distance between the upper border of the coracoids process and the inferior cortex of the clavicle, and acromioclavicular distance (ACD) was defined as the perpendicular distance between the line passing the upper border of the acromion and the line parallel to the upper border of the lateral part of the clavicle. All radiographs were analyzed by two authors who reached a consensus. p-values of less than 0.05 were considered significant.
Results
Clinical Outcomes
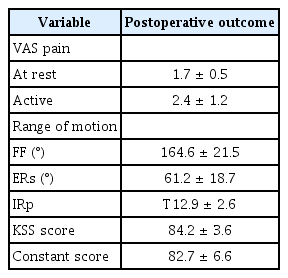
The clinical and radiological outcomes are presented in Table 2. The VAS, ROM, Constant, and KSS score were evaluated as clinical factors at the last follow-up. The mean VAS score while resting was 1.7 ± 0.5 points and that while active was 2.4 ± 1.2 points. The mean joint range of the FF was 164.6° ± 21.5°, while ERs was 61.2° ± 18.7°, and IRp was T12.9 ± 2.6. The mean Constant score was 82.7 ± 6.6 points, while the mean KSS score was 84.2 ± 3.6 points. All cases achieved a satisfactory outcome.
Radiologic Outcomes
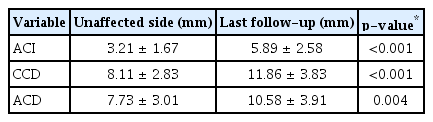
Significant differences were observed between the average ACI, CCD, and ACD in the preoperative stage and that on the last follow-up radiographs of the affected shoulder (Table 3). The average ACI, CCD, and ACD were significantly reduced on the last follow-up. The average decrease of ACI was 3.1 mm (9.03 ± 3.02 mm vs. 5.89 ± 2.58 mm, p<0.001), while that of CCD was 5.8 mm (17.59 ± 4.50 mm vs. 11.86 ± 3.83 mm, p<0.001), and that of ACD was 7.1 mm (17.66 ± 5.70 mm vs. 10.58 ± 3.91 mm, p<0.001) based on evaluation of the radiographs.

Radiologic Outcomes of Modified Phemister Operation with Coracoclavicular Ligament Augmentation Using Suture Anchor
Comparison of the ACI, CCD, and ACD values of the contralateral unaffected shoulder and affected shoulder at the last follow-up revealed that the affected shoulders had significantly higher average ACI (3.21 ± 1.67 mm vs. 5.89 ± 2.58 mm, p<0.001), CCD (8.11 ± 2.83 mm vs. 11.86 ± 3.83 mm, p<0.001), and ACD (7.73 ± 3.01 mm vs. 10.58 ± 3.91 mm, p=0.004) values (Table 4).
Complications
There were four cases (5.4%) of skin irritation, migration of the K-wire occurred in three (4.1%) patients and breakage occurred in eight patients (10.8%). When K-wire migration or breakage occurred, hardware was removed after AC joint stabilization was confirmed. These patients did not complain of pain after hardware removal. At the time of K-wire removal, we had no case of immediate secondary re-dislocation of the AC joint. Follow-up radiographs showed AC osteoarthritis in two patients (2.7%). No patients had intraoperative or postoperative clavicular or coracoid fracture, infection, or revision surgery.
Discussion
The principal finding of the present study was that modified Phemister operation using augmentation of the coracoclavicular ligament by suture anchor for the treatment of acute AC joint dislocation successfully restored the stability of the AC joint. Satisfactory clinical and radiologic outcomes were simultaneously achieved in this study. At the final follow-up, the mean VAS score was 1.7 ± 0.5 points, the Constant score was 82.7 ± 6.6 points, and the KSS score was 84.2 ± 3.6 points. An acceptable joint alignment was achieved in all the patients after surgery. Furthermore, the authors found no problems achieving AC joint stabilization by this technique. In addition, the technique was simple with low hardware costs.
Over the last decade, numerous surgical procedures have been described for the management of acute AC joint dislocation [4,5]. Despite the use of various methods of surgical treatment of acute AC joint dislocations such as K-wire, hook-plates, screws, synthetic sling materials, and ligament reconstruction, no technique has been shown to be clinically superior to another [4,10,25-27]. Among these methods, the modified Phemister technique with K-wire is relatively simple, fast, and inexpensive. Additionally, the use of a suture anchor offers the advantage of quick fixation of the coracoclavicular ligament to bone while minimizing extensive soft tissue exposure [20,28].
Rolf et al. [29] reported the outcomes of 29 patients treated with a modified Phemister technique that included augmentation of the coracoclavicular ligaments with polydioxanone suture. Specifically, an additional polydioxanone cord was passed around the base of the coracoids and formed into a figure-8-shaped sling through a hole drilled in the lateral clavicle. After a follow-up of 53 months (range, 20 to 92 months), the authors showed clinical results statistically favoring the early treatment of injuries. Corella et al. [30] reviewed the outcomes of type III and type V AC dislocations treated using the Phemister technique and found good results in the immediate postoperative period, but long-term relapses in 66% of the cases, despite a high level of subjective satisfaction reported by patients. Moon et al. [21] conducted a retrospective study of 14 patients who underwent a modified Phemister procedure with a suture anchor added for augmentation of the conoid ligament in cases of acute dislocation of the AC joint. At the mean follow-up (14 months), functional results were good/excellent with a Constant score of 90.8 and KSS score of 91. In our study, we observed good clinical and functional results at the follow-up examination with respect to the ROM, strength and pain discomfort. Moreover, the Constant and KSS scores showed global satisfaction with the procedure.
Rhee et al. [16] reported good radiologic outcome in a retrospective study that compared the K-wire transfixation group and the locking hook plate group. Overall, they showed that the K-wire transfixation group had an average increase in ACI of 2.2 mm, CCD of 2.0 mm, and ACD of 1.8 mm upon comparison of the contralateral unaffected shoulder and affected shoulder at the last follow-up. Verdano et al. [31] used a modified Phemister technique that combined loop augmentation, coracoclavicular ligaments repair and transarticular stabilization with K-wire for acute AC joint dislocation. In their study, at the time of radiological follow-up, three patients maintained the reduction (21.4%), while nine (64.3%) showed a partial recurrence of the dislocation (<3 mm) and two (14.3%) showed complete re-dislocation. Kim and Chun [32] compared use of tans-acromial fixation and the AO hook plate for the treatment of acute AC joint dislocation and found that the K-wire trans-acromial fixation group had a significantly greater CCD than the AO locking hook plate group. In the current study, the average ACI, CCD, and ACD was significantly reduced at the last follow-up and all patients maintained an acceptable reduction of the AC joint.
Leidel et al. [15] described K-wire migration in 4% (n=3) and secondary dislocation of the AC joint in 11% (n=8) of cases after wire removal. None of the 70 patients who underwent surgery for type III injuries became infected. Mayr et al. [33] reported a loss of reduction rate of 28%, with a less satisfactory outcome in patients who underwent the modified Phemister procedure. Calvo et al. [34] used the modified Phemister technique in 32 surgically treated type III AC dislocations and found that only 50% of the AC joints were reduced in long-term follow-up, with a significantly higher incidence of osteoarthritis (81.2%) and coracoclavicular ligament ossification (59.4%). In the present study, all K-wires were inserted bicortically to provide more stable fixation and they were bent to prevent forward migration. Moreover, efforts were made to provide coracoclavicular ligament augmentation, which helped reduce the incidence of complete failure or re-dislocation.
It should be noted that this study has several limitations. First, being retrospective in nature, our study has limitations similar to other retrospective studies. Second, the follow-up period was relatively short and the incidence of arthritis in the AC joint would be different in long-term follow-up. However, the strengths of this study include that the procedure was relatively simple, fast, and inexpensive; and all operations were performed by a single surgeon.
Conclusion
The modified Phemister operation with coracoclavicular ligament augmentation using a suture anchor led to satisfactory clinical and radiological outcomes and was found to be safe, showing a low complication rate in acute dislocations of the AC joint. This surgical technique also has a low learning curve procedure with low hardware costs. Our data suggest that the modified Phemister procedure for the surgical treatment of acute AC joint dislocations is a reliable technique for restoration of shoulder girdle.
Notes
Research Ethics
IRB approval: Kyung Hee University Hospital at Gangdong (No. KHNMC 2019-04-009).
Conflict of interest
None.
Financial support
None.