Physicians developed reverse total shoulder arthroplasty (RTSA) to treat rotator cuff tear arthropathy accompanied by glenohumeral arthritis caused by massive rotator cuff tear in elderly patients [1]. As favorable outcomes have been reported in terms of pain abatement and function, the range of applicability for RTSA has broadened; as a result, physicians are performing more of these procedures, which has led to increase in complications [2]. The most common problem of this technique is scapular notching, which is seen often in cases of reverse shoulder implant based on the Grammont design. Complications that require additional surgery such as revision arthroplasty include instability, infection, and implant loosening [3], and physicians usually perform revisions using the same type of implant as used previously. The authors of the present study performed a partial revision in a case involving instability with scapular notching and glenoid aseptic loosening using glenoid and humerus components from different manufactures and achieved favorable outcomes.
CASE REPORT
Owing to the retrospective design of this study, approval of the Institutional Review Board was waived. Before surgery, consent was obtained from the patient for this study.
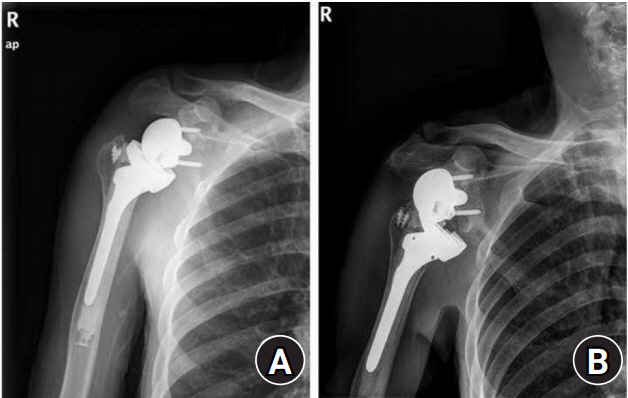
A 71-year-old man was admitted for instability in the right shoulder that had gradually worsened. The patient was very anxious about possible dislocation of his right shoulder from minor trauma, such as coughing. A review of his medical history showed arthroscopic cuff repair and debridement 6 years prior for massive rotator cuff tear and mini-open cuff repair for cuff re-tear. However, because there was no improvement in his symptoms, he underwent RTSA on his right shoulder in October 2010, using a shoulder replacement system (Zimmer Inc., Warsaw, IN, USA) based on Grammont’s design (Fig. 1A).
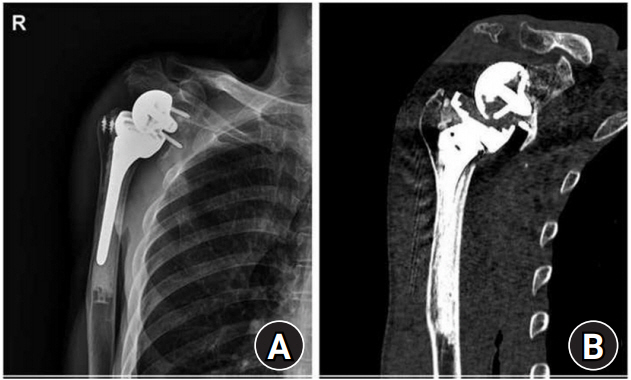
The patient had no other symptoms when he suffered a dislocation. He underwent manual reduction in the emergency room and was discharged. However, the same dislocation occurred four more times in 6 months (Fig. 1B). At the time of admission, his range of motion consisted of active forward flexion of 80° and abduction of 40°, while internal rotation was identified as the greater trochanter of the femur. On radiologic examination, the glenoid surface was located superiorly during the first RTSA, baseplate loosening was accompanied by superior migration after recurrent dislocation, and progressive scapular notching (grade 4, Nerot-Sirveaux grading system) was identified [4]. Other than these problems, the humerus implant appeared to be stable (Fig. 2). A revision surgery was planned to address the recurrent dislocation and accompanying glenoid side problem. For recovery of stability through appropriate recovery of tension in the deltoids, the humerus was planned to be moved to a more distal and lateral position. For the glenoid side, the plan was to prevent inferior scapular notching and implant loosening by increasing the inferior tilt of the glenoid and positioning the baseplate more inferiorly. Due to a large bone defect due to glenoid notching, use of the existing baseplate would have required a large autologous bone graft.
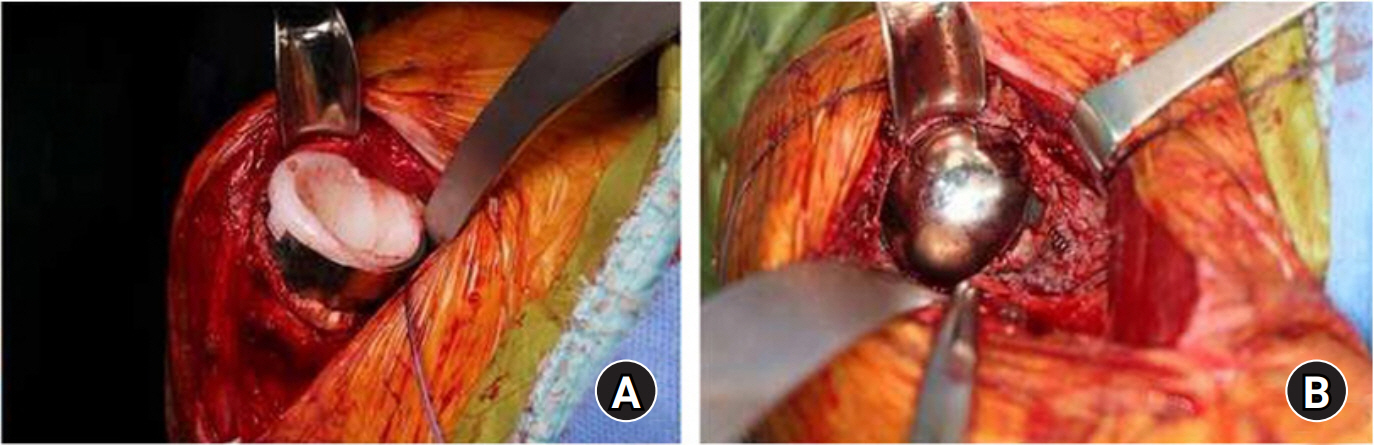
However, it was determined that using the same size or larger baseplate after applying a large amount of autologous bone graft may cause unstable fixation. Thus, a DJO Surgical Reverse Shoulder Prosthesis (DJO Surgical, Austin, TX, USA) that has a smaller baseplate than the existing one but the same glenoid hemisphere size was chosen as the implant. Moreover, because the DJO Surgical Reverse Shoulder Prosthesis is an implant that has its center of rotation closer to the anatomical center than the existing implant based on the Grammont design, it is expected to contribute to shoulder stabilization by providing lateral movement by the humerus. The deltopectoral approach that had been used previously was employed with the patient in the beach chair position under general anesthesia. Culture tests on tissues and frozen biopsy were performed to test for infection. Since humeral implant loosening was not observed, it was left intact, and the polyethylene liner and socket were removed for the glenoid side approach. During the removal process, polyethylene liner wear was confirmed (Fig. 3A). After separating the glenoid hemisphere from the baseplate, the screws and baseplate were removed. Step-like bone defect from impingement on the inferior glenoid and a central peg hole were identified (Fig. 3B). The central hole was filled by an autologous iliac bone graft, and the baseplate was positioned as inferiorly as possible during fixation to the glenoid to produce an inferior tilt.
Reduction was performed after confirming that the thickness was appropriate by inserting a polyethylene trial into the humeral implant. The suitability of polyethylene thickness was evaluated by considering the tension of the conjoint tendon when the humerus was externally rotated and tracted downward. After inserting the metallic spacer and thick polyethylene, the subscapularis tendon and anterior soft tissues were re-sutured (Fig. 4). After surgery, the patient wore an abduction brace for 6 weeks, during which only pendulum exercise was allowed in the shoulder. After surgery, the patient wore an abduction brace for 6 weeks, during which only pendulum exercise was allowed in the shoulder. Active exercise was recommended for the elbow, wrist, and hand to control for swelling. After 6 weeks, the brace was loosened, and active assistive joint exercise was performed. From postoperative 3 months, movements necessary for activities of daily living were allowed based on pain tolerance. When the patient visited 6 months later, he reported no discomfort; at postoperative 4 years, he showed active forward flexion of 150°, abduction of 100°, and internal rotation of L2, increases from preoperative levels (Fig. 5). No other postoperative complication was found.
DISCUSSION
Complications after RTSA include scapular notching, postoperative instability, infection, periprosthetic fractures, glenoid or humerus implant loosening or fracture, screw loosening, acromion or scapular spine fractures, hematoma, heterotrophic ossifications, and nerve damage [2]. Among these, scapular notching is the most common and occurs due to mechanical impingement between the inner surface of the humeral cup and the lateral scapula pillar below the glenoid hemisphere, and the Grammont design tends to induce such impingement [4]. Some results indicate that scapular notching may have a negative impact on surgical outcome, but most indicate that it does not affect surgical outcome; the findings are inconsistent [5]. Unlike the Grammont design, the DJO Surgical Shoulder Prosthesis has a center of rotation close to the anatomical center and appears capable of preventing glenoid notching [3].
Instability is one of the major complications requiring surgical treatment [3]. Some authors have reported that the deltopectoral approach has a negative effect [6], but the observation of subscapular tendon rupture, fat degeneration, and brachial angulation in the reported cases, so we can suggest that the approach will not be a significant factor [3]. Another cause is dislocation from loosening of the tension in the deltoids. It is believed that this is due to preoperative deltoid dysfunction, humeral shortening from various factors that cause proximal humeral defect, or medial translation of the humerus [2]. Therefore, when planning revision surgery, humeral shortening or medial translation should be assessed and confirmed from radiologic examination of the humerus bone and should be measured to make the necessary preoperative preparations [7]. Moreover, to induce adequate tension in the deltoids during revision, it is necessary to insert a humeral implant metallic spacer, a thick polyethylene liner, or an even longer humeral implant to lengthen the humerus or to use a hemisphere that is bigger or located more laterally to position the humerus more laterally [2].
In the present case, the existing glenoid implant was implanted into the patient with a superior tilt, allowing glenoid implant dissociation from shearing forces, resulting in instability from bone loss caused by joint notching and dislocation. Because the patient underwent RTSA on both sides, assessment of the humerus on both sides by preoperative radiologic examination was difficult, and appropriate tension on the deltoids was only assessed intraoperatively. Although the humeral length could be increased by inserting a metallic spacer or a thick polyethylene liner, because it was accompanied by a glenoid side bone defect, it was difficult to use a large hemisphere. Thus, an implant that can use a smaller baseplate and has a center of rotation more lateral than the implant based on the Grammont design was selected to achieve stability by shifting the humerus more laterally. When using the two types of implants, the glenoid hemisphere and polyethylene cup sizes were the same. Although conformity may vary, we believe that there will not be any problem with wear since the shoulder is not a weight-bearing joint. Instability after RTSA can be treated by inserting appropriate implants to prevent inferior capsular notching and glenoid side loosening.