Rotator cuff retear after repair surgery: comparison between experienced and inexperienced surgeons
Article information
Abstract
Background
We hypothesized in this study that the characteristics of retear cases vary according to surgeon volume and that surgical outcomes differ between primary and revision arthroscopic rotator cuff repair (revisional ARCR).
Methods
Surgeons performing more than 12 rotator cuff repairs (RCRs) per year were defined as high-volume surgeons, and those performing fewer than 12 RCRs were considered low-volume surgeons. Of the 47 patients who underwent revisional ARCR at our clinic enrolled in this study, 21 cases were treated by high-volume surgeons and 26 cases by low-volume surgeons. In all cases, the interval between primary surgery and revisional ARCR, degree of “acromial scuffing,” number of anchors, RCR technique, retear pattern, fatty infiltration, retear size, operating time, and clinical outcome were recorded.
Results
During primary surgery, significantly more lateral anchors (p=0.004) were used, and the rate of use of the double-row repair technique was significantly higher (p<0.001) in the high- versus low-volume surgeon group. Moreover, the “cut-through pattern” was observed significantly more frequently among the cases treated by high- versus low-volume surgeons (p=0.008). The clinical outcomes after revisional ARCR were not different between the two groups.
Conclusions
Double-row repair during primary surgery and the cut-through pattern during revisional ARCR were more frequent in the high- versus low-volume surgeon groups. However, no differences in retear site or size, fatty infiltration grade, or outcomes were observed between the groups.
INTRODUCTION
Rotator cuff retear after arthroscopic rotator cuff repair (ARCR) significantly lowers the likelihood of a good clinical outcome and is therefore clinically important [1]. Rotator cuff retear rate ranges from 7.2% to 94% [2-5]. The risk factors for rotator cuff retear are larger initial tear size, older age, and degree of fatty degeneration [6,7]. The retear rate for ARCR is reported to be higher than that for primary ARCR [8]. Some studies have compared surgical outcomes according to surgeon volume [9,10], but not for revisional ARCR. In this study, we hypothesized that the surgical findings and outcomes of revisional ARCR differ according to the surgical volume of the surgeon who performed the primary ARCR.
METHODS
This study was approved by the Institutional Review Board of Konkuk University Medical Center (IRB No. KUMC2019-11-062). Informed consent was waived due to retrospective nature of this study.
Patient Selection
Of the 53 patients who underwent revisional ARCR from January 2009 to February 2019, this study included 47: three were excluded because their medical records did not include the primary surgeon, two because there were no arthroscopic images of the revision ARCR, and one because there was no preoperative magnetic resonance imaging (MRI) scan. The median age at the time of revisional ARCR was 61 years (range, 41–78 years). Thirty cases (63.8%) involved the right shoulder and 17 (36.2%) involved the left shoulder. The median follow-up period after revisional ARCR was 34 months (range, 18–78 months). Four of the 47 patients underwent open rotator cuff repair (RCR) and 43 underwent ARCR. The median interval between primary surgery and revisional ARCR was 20.5 months (range, 12–149 months).
Shoulder Surgeon Volume
The Health Insurance Review and Assessment Service was consulted to determine the number of RCR operations per year were conducted by each primary surgeon. The average number of RCRs per year was determined from the first year in which primary surgeons started to perform RCR onward. Weinheimer et al. [10] defined high-volume surgeons as those who performed at least 5 arthroplasties and at least 12 ARCRs per year. In this study, surgeons who performed 12 or more ARCRs per year were defined as high-volume surgeons and those who performed fewer than 12 as low-volume surgeons.
Radiologic Assessment
Preoperative MRI images were used to evaluate fatty infiltration, the number and location of anchors, the primary operative technique, and the retear pattern. Fatty infiltration was classified according to the highest Goutallier stage among the supraspinatus, infraspinatus, and subscapularis muscles [11]. Anchors were counted on the medial and lateral sides of the rotator cuff footprint. The primary surgical technique was considered as single-row when there were only medial anchors and as double-row when there were both medial and lateral anchors. In accordance with Cho et al. [12], the retear pattern was classified as type 1 when no rotator cuff tissue was visible in the rotator cuff footprint and as type 2 when remnant cuff tissue was present. The retear was classified as “extra only” if the retear did not affect the previous surgical area [13].
Arthroscopic Finding
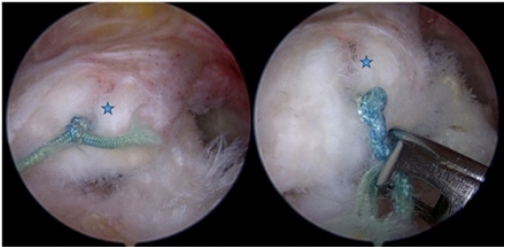
All revisional ARCRs were performed by the senior surgeon (JYP) with the patient under general anesthesia in the beach-chair position. All surgical findings were added to the patients’ medical records, including photographs. Retear size was recorded to the millimeter based on arthroscopic images. The associations of radiologic findings, the primary RCR technique used, and the retear pattern were assessed. The degree of scuffing of the acromial undersurface (hereafter, “acromial scuffing”) was evaluated using the Copeland–Levy classification (A0–A1, minor; A2–A3, major) (Fig. 1) [14]. The “cut-through pattern” is defined by the presence of tendon tissue torn longitudinally by the suture knot (Fig. 2) [15,16].
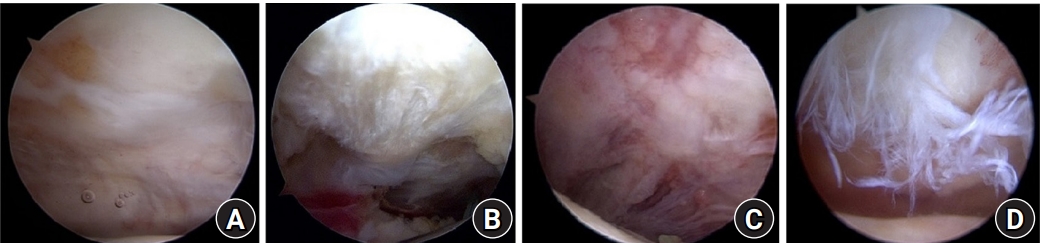
Arthroscopic images: (A) no scuffing (A0), (B) minor scuffing (A1), (C) major scuffing and fibrillations (A2), and (D) acromial bare bone exposure (A3).
Clinical Assessment
Preoperative status and postoperative outcomes were determined by reference to the medical records using a visual analog scale (VAS), the American Shoulder and Elbow Surgeons (ASES) score, the Korean Shoulder Scoring (KSS) system, and the Constant-Murley Score (CMS). Shoulder abduction power (kg) was also recorded [17].
Statistical Analysis
Data are provided as mean and standard deviation and were checked for normality using the Kolmogorov-Smirnov test. All data, except the number of anchors and Goutallier stage, followed a normal distribution. Normal data were analyzed using paired and unpaired t-tests. Non-normally distributed data were analyzed using the Mann-Whitney U-test and Wilcoxon signed-rank test. All analyses were performed with SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA). A p-value <0.05 was considered significant.
RESULTS
Of the 47 revisional ARCR cases, 21 surgeries were conducted by high-volume surgeons and 26 by low-volume surgeons. No differences in sex, age, or follow-up duration were observed between the high- and low-volume groups (Table 1). The time between primary and revision surgery (p=0.534), acromial scuffing (p=0.853), number of medial anchors (p=0.397), total number of anchors (p=0.228), retear pattern (Rhee type) (p=0.061), number of cases with extralesional tears only (p=0.158), fatty infiltration (Goutallier stage) (p=0.284), retear size (p=0.545), and operating time for revision (p=0.528) were not different between the two groups. The number of lateral anchors and frequency of use of the double row operating technique were significantly higher in the high- versus low-volume group (p=0.004 and p=0.000, respectively). However, cases were omitted from the analysis if the repair technique could not be clearly identified based on the MRI or arthroscopic images. The cut-through pattern was observed more frequently in the high- versus low-volume group (p=0.008) (Table 2).
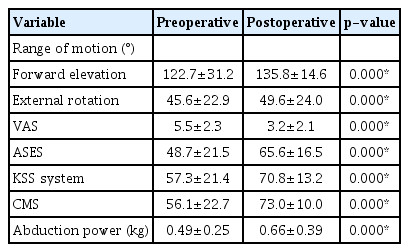
The VAS, ASES, KSS, and CMS scores, range of motion, and abduction power were significantly different at the final follow-up after revision surgery compared to preoperatively (all p=0.000) (Table 3). The preoperative VAS (p=0.545), ASES (p=0.596), KSS (p=0.556), and CMS scores (p=0.714), range of motion (forward elevation, p=0.064; external rotation, p=0.269), and abduction power (p=0.077) were not significantly different between the high- and low-volume groups (Table 4). The postoperative VAS (p=0.343), ASES (p=0.099), KSS (p=0.805), CMS scores (p=0.100), range of motion (p=0.199), and abduction power (p=0.402) were not significantly different between the high- and low-volume groups (Table 5).
DISCUSSION
Rotator cuff tears account for a significant proportion of all shoulder problems in the general population, and their prevalence increases with age [18]. A full-thickness rotator cuff tear, or a partial tear >50%, is an indication for RCR [19]. The open and arthroscopic surgical results of RCR have been reported to be good [2,20,21].
Several systematic reviews have assessed outcomes by surgeon volume. Weinheimer et al. [10] reported that surgery time, cost, complications, and length of stay increase when the volume of the shoulder surgeon is small. Shervin et al. [9] reported that the hip dislocation rate was lower after hip arthroplasty by high- versus low-volume surgeons; for other outcomes there was no difference by surgeon volume, or the results were inconclusive. A high frequency of double-row repairs during primary RCR and a higher frequency of the cut-through pattern were observed in the high-volume group in this study. No other outcomes differed between the surgeon volume groups.
No consensus has not been established regarding the indications or optimal surgical approach for acromioplasty [22]. We investigated whether the rate of performance of acromioplasty differed by surgical volume. However, there were insufficient data to determine the rate of performance of acromioplasty as the primary operation according to the extent of acromial scuffing. Studies have shown that the double-row repair technique confers benefits in terms of tendon healing and has a lower retear rate than single-row repair [23-25]. However, other studies showed no significant difference in clinical outcomes between the techniques for small-to-medium-sized cuff tears [26,27].
There was a correlation toward a higher incidence of the Rhee type 2 retear pattern in our high- versus low-volume group (p=0.061) [12]. This may be related to the large number of double row repairs performed by the high-volume surgeons. In cases with tears outside of the previous surgical site (extralesional only), the previous rotator cuff surgical site may be intact, which would tend to produce a more favorable result. However, further study is needed to confirm this.
No study has assessed the mechanism or risk factors for the cut-through rotator cuff retear pattern. The cut-through pattern leads to longitudinal tears in the medial part of the rotator cuff due to the suture anchors on footprint. Therefore, this pattern should not be used in cases of Rhee type 2 retear in which retear occurs in the medial aspect of the medial anchor. However, further study is needed to validate this [12].
In this study, many outcomes showed no difference by surgeon volume. Thus, even surgeons performing fewer than 12 shoulder surgeries per year could be considered for rotator cuff retear. An insufficient number of cases was a limitation of this study: the amount of data on certain outcomes, such as extralesional, Rhee type 2, and cut-through tear patterns, was relatively small so further studies are needed. Also, no distinction was made between open and arthroscopic surgery for primary ARCR. In this study, we were interested in how the initial cuff tear size varied according to surgeon volume but could not obtain sufficient surgical records or MRI images of the primary surgeries to quantify the tear sizes. Thus, we tried to indirectly determine the sizes of the cuff tears according to the number of medial anchors used; although the number of medial anchors tended to higher in the high-versus low-volume group, the difference was not significant (p=0.397). Furthermore, the number of anchors may have been counted inaccurately in some cases: biocomposite anchors used for primary ARCR are difficult to detect on MRI images, and some of the images were of insufficient quality to detect the anchors. Furthermore, some anchors have metal components which can impair image quality, while open repair can be performed without using any suture anchors.
Based on our results, the conclusion that all high-volume surgeons are distinctive to low-volume surgeons cannot be made. Although surgeon experience is an important factor, Guttman et al. [28] found no significant difference in surgical time after the first 10 cases. This finding suggests that not only the annual average number of operations, but also the cumulative number, is meaningful. Further study is needed to explore this issue. High-volume surgeons frequently employed double-row repair as the primary RCR technique, and the cut-through pattern was more prevalent in the high- versus low-volume group. However, there were no group differences in retear site or size, fatty infiltration grade, or any other outcome.
Notes
Financial support
None.
Conflict of interest
None.