 |
 |
- Search
| Clin Shoulder Elb > Volume 25(3); 2022 > Article |
|
Abstract
Background
This study aimed to examine the preliminary clinical results of the infraspinatus rotational transfer procedure for irreparable posterosuperior rotator cuff tears.
Methods
This study included 34 patients (mean age, 68.4 years). Their mean tear width and length measurements were 50.9 mm and 50.6 mm, respectively. The functional outcomes, including physician-determined and patient-reported scores, were evaluated before and at 1 year after surgery. The structural outcomes determined using the magnetic resonance imaging examination results were also assessed.
Results
The clinical scores significantly improved after surgery compared with the scores before surgery: the Constant-Murley score (53.3±21.1 to 76.8±10.5), University of California at Los Angeles Shoulder score (15.6±3.6 to 27.8±6.7), American Shoulder and Elbow Surgeons Shoulder score (51.8±18.3 to 89.1±13.5), and WORC score (925.0±436.8 to 480.3±373.2) (all p<0.001). Postoperative re-tears were noted in two patients (5.9%).
Full-thickness rotator cuff tears (RCTs) tend to be larger in patients under 60 years of age [1], and the tear size progresses to approximately 50% after an average of 2 years; consequently, surgery may be considered at an early stage [2]. Several randomized controlled trials and meta-analyses have shown that in RCTs, surgical repair is associated with better clinical outcomes compared with non-surgical treatment [3-5].
There has been controversy regarding the best treatment for irreparable large and massive RCTs. Several alternative surgical procedures have been applied: partial repair [6], tendon transfer (latissimus dorsi tendon [7], pectoralis major [8], and lower trapezius [9]), superior capsular reconstruction (SCR) [10], and balloon arthroplasty [11]. Moreover, no specific treatment strategies are currently recommended because of the paucity of high-quality clinical studies available for guiding the management of irreparable massive RCTs [12]. Therefore, the definition of an irreparable RCT remains controversial. The irreparability of the tendon is typically multifactorial and includes both imaging findings and patient factors. In addition, Warner et al. defined an irreparable RCT as an injury where the tendon stump does not reach the footprint after soft tissue mobilization [13]. Consistently, this study defined an irreparable RCT as described above.
Morihara et al. [14] reported the results of a modified Debeyre-Patte procedure for irreparable large and massive RCTs. In their study, the re-tear rate was 23% and was significantly associated with the degree of general fatty degeneration index. Asato et al. [15] modified and developed a novel surgical procedure from the Japanese literature for irreparable posterosuperior RCTs termed “infraspinatus rotational transfer.” They applied this procedure in patients with more severe infraspinatus (ISP) fatty degeneration (n=12) and demonstrated a re-tear rate of 0% after surgery. However, no studies in the English literature have reported the clinical results of infraspinatus rotational transfer (IRT) for irreparable large and massive RCTs. We have carried out the IRT procedure to treat irreparable posterosuperior large/massive RCTs since 2018. Thus, we hypothesized that this procedure leads to acceptable clinical outcomes postoperatively. The purpose of this study was to evaluate the clinical results of IRT for irreparable posterosuperior large/massive RCTs at 1 year postoperatively.
This study was approved by the Health Sciences Institutional Review Board of Fukuoka Shion Hospital (IRB No. 13-012). Informed consent to participate in this study was obtained from all participants.
The inclusion criteria were as follows: (1) patients with large (3.0–5.0 cm) or massive (>5.0 cm) RCTs who had undergone arthroscopic repair, (2) those who were available for magnetic resonance imaging (MRI) preoperatively, (3) those who underwent the appointed postoperative rehabilitation program, and (4) those who were available for a postoperative follow-up after 1 year. However, the exclusion criteria were as follows: (1) patients who had a successful primary repair during surgery, (2) those who had irreparable SSC tears (> Lafosse classification type 2), (3) those who had other orthopedics-associated or systemic diseases, and (4) those who could not be followed-up.
From 2017 to 2020, 179 patients with RCTs underwent arthroscopic rotator cuff repair. According to our criteria, those with small/medium-sized tears (n=100), those who experienced primarily repaired large or massive tears (n=79), those who had a successful primary repair during surgery (n=37), those with RCTs that had subscapularis tendon involvement (>Lafosse classification type 2, n=5), patients with other orthopedics-associated or systemic diseases (n=2), and those who could not be followed-up (n=1) were excluded. Consequently, 34 patients who met the inclusion criteria were examined and then included in the present study. There were 3 large and 31 massive tears; their mean width and length were 50.9 mm and 50.6 mm, respectively. The mean age at the time of surgery was 68.4 years (range, 57–76 years), with a mean follow-up period of 12.6 months (range, 12–18 months). Further details are shown in Table 1.
After the induction of general anesthesia, the patients were placed in the beach chair position. The tendon stumps in all patients were proximally retracted beyond the glenoid edge (Fig. 1A). Despite thorough mobilization, including capsular/coracohumeral ligament release, these stumps did not reach the footprint of the greater tuberosity (Fig. 1B). Next, an approximately 4-cm straight incision was made on the scapula spina. The interface between the subcutaneous tissue and the infraspinatus (ISP) was released digitally. Using fingers and metal instruments, the margin of the ISP was gently separated from the medial border of the scapula, the posterior margin of the glenoid, the superior portion of the teres minor, and the scapula body (Fig. 2A). These procedures allowed the tendon stumps to easily reach the superior facet area near the bicipital groove (Fig. 2B). Finally, the approximated tendon was fixed using the suture bridge technique with two anchors in the medial row (Healix Advance; DePuy Synthes, Raynham, MA, USA) and two anchors in the lateral row (SwiveLock; Arthrex, Naples, FL, USA) (Fig. 1C).
In cases with osteophytes in the subacromial space, acromioplasty was performed (75.7%). Tenotomy of the long head biceps tendon was carried out when a tear of half or more of the width was present (45.9%). Partial tears of the upper subscapularis tendon were treated by shaving, not by repair; in our series, no full-thickness tears of this tendon were detected. The mean operative time was 115±23.2 minutes. Further details are shown in Table 1.
After surgery, the patients were placed in an immobilization sling in a neutral position for 8–10 weeks. All patients underwent postoperative regimens under the strict supervision of a physical therapist. We began passive elevation exercises and external/internal rotations in a supine position one week postoperatively. Active exercises were subsequently initiated in the sitting or standing position at 8–10 weeks postoperatively. Strength exercises were started at 4–5 months postoperatively, and the patients resumed their previous work activities 6 months postoperatively.
The functional outcomes were assessed by the Constant-Murley Score (Constant), University of California at Los Angeles (UCLA) Shoulder Score, and Japanese Orthopaedic Association (JOA) scores. Patient-reported outcomes were assessed using the Shoulder Index of the American Shoulder and Elbow Surgeons (ASES), Western Ontario Rotator Cuff Index (WORC), and JOA Shoulder 36 score version 1.3 (Shoulder 36). Range of motion (ROM) was evaluated before the surgery and then again at 12 months postoperatively using the active elevation, external rotation, and internal rotation. The internal rotation was measured as the highest vertebral body that the patient could reach with the thumb of the affected arm. The degree of pain (in motion and at night) was assessed using a visual analog scale (0–100 mm). Muscle strength was evaluated using a handheld dynamometer (MicroFET2; Hoggan Health Industries, Draper, UT, USA) in a sitting position with the hips and knees at 90° flexion. Measurements of the strength of the 40° abductor and the 90° abductor were performed in the shoulder joint’s internal and external rotation positions, respectively, along with the external rotation and internal rotation strength in the 0° abduction position. Each measurement was taken three times, and the average value was calculated. These functional evaluations were performed both before and at 12 months after the surgery.
Preoperatively, the tear size was measured by MRI as the maximum anteroposterior tear width on T2-weighted sagittal images and the maximum mediolateral tear length on T2-weighted oblique-coronal images [16]. Preoperative fatty infiltration of the rotator cuff muscles was assessed using the Goutallier Classification [17]. The postoperative cuff integrity was evaluated with MRI 12 months after surgery; images with Sugaya classification Types 4 or 5 were considered re-tears [18]. Subsequently, two observers blinded to this study independently assessed the structural outcomes. Reproducibility between these two observers showed “good” interrater reliability (ICC [3, 1]=0.85) and “excellent” intrarater reliability (ICC [1, 2]=0.92).
We used statistical software (R version 2.8.1; R Foundation for Statistical Computing, Vienna, Austria) to analyze the data. After confirming a normal distribution using the Shapiro-Wilk test, a paired t-test or Wilcoxon rank-sum test was utilized. The Wilcoxon rank-sum test was used to compare the Constant, UCLA, JOA, ASES, WORC, and Shoulder 36 scores, ROM, pain level, and muscle strength both before and after surgery. A p-value <0.05 was considered statistically significant.
Compared with the preoperative scores, the mean scores significantly improved 12 months postoperatively as follows: Constant (53.3±21.1 to 76.8±10.5), UCLA (15.6±3.6 to 27.8±6.7), ASES (51.8±18.3 to 89.1±13.5), and WORC (925.0±436.8 to 480.3±373.2) (all p<0.001). Although the range of motion of active elevation significantly improved after surgery (95.6°±51.1 to 146.9°±14.5; p<0.001), these improvements were not observed for external or internal rotation (Table 2). Additionally, while 44.1% of all patients exhibited pseudoparalysis before the surgery, they all had improved 1 year after surgery.
This study included 15 patients with preoperative pseudoparalysis (15/34, 44.1%) who experienced significant improvements in their functional and patient-reported outcomes after surgery. We observed no re-tears in these 15 patients. The results also showed that the preoperative pain level while in motion and at night significantly improved after surgery (41.4±25.2 to 6.7±14.9 mm and 21.8±24.8 to 4.3±10.3 mm; p<0.001), respectively (Table 2).
Additionally, the 40° abductor muscle strength during external rotation improved from 53.0±24.4 to 63.3±19.5 N (p=0.028), while the internal rotation improved from 60.9±24.0 to 70.7±20.4 N (p=0.042); however, these improvements were not observed at the other positions. These data are summarized in Table 2.
At the 1-year postoperative evaluation, the Sugaya’s classifications were type I in 8 patients, type II in 15 patients, type III in 9 patients, type IV in 1 patient, and type V in 1 patient (Table 2). Consequently, postoperative re-tears were noted in two shoulders (5.9%) that were types IV and V.
As a muscle advancement procedure for treating irreparable RCTs, Asato et al. [15] developed the IRT technique in which the ISP muscle is fully separated from the surrounding tissues and then advanced to the footprint without creating too much tension. They reported successful outcomes without any postoperative re-tears in the Japanese literature. However, no English literature regarding this technique has been published. The present study investigated the preliminary outcomes of the IRT technique in patients with irreparable posterosuperior RCTs. Both physician-based and patient-based functional outcomes were significantly improved, with a re-tear rate of 5.9% 1 year after surgery, including preoperative pseudoparalysis cases (15/34, 44.1%). Thus, we believe that the IRT technique is a useful surgical option for irreparable posterosuperior RCTs.
Developed by Asato in 2010, IRT focuses on the anatomical restoration of ISP function rather than SSP function. Mochizuki et al. [19] reported that, compared with the SSP, the ISP covers most of the greater tuberosity, indicating the higher importance of repairing the ISP in RCTs. In our series, IRT improved the strength and ROM of elevation after surgery but failed to show significant improvement of the external rotation range and strength at 1 year postoperatively, except for recovery of muscle strength with the arm abducted 40°. This finding may imply that advancement of the ISP leads to a “spacer effect,” which helps to exert deltoid function effectively, but not to full recovery of the range and strength of external rotation. In other words, IRT may function to depress and center the humeral head in the glenoid and help the deltoid muscle to elevate the arm, as reported in biomechanical studies of SCR [20] and balloon spacer [21] procedures.
Various alternative procedures for irreparable RCTs have been reported. The lower trapezius transfer technique using an Achilles tendon allograft was reported to improve the clinical outcome in 90% of patients. However, two patients underwent reverse shoulder arthroplasty, and two experienced traumatic rupture of the transfer at 14 months postoperatively [22]. The latissimus dorsi transfer technique has a high rupture rate of 38% [23]. In this study, when we compared patients aged ≤ 55 years and ≥ 75 years, the re-tear rates were 33% and 26%, respectively, but there was no significant difference in the clinical outcomes and satisfaction rates, suggesting that it is a useful procedure for patients aged ≥75 years [24]. SCR has been increasingly investigated and reported in recent years. In a systematic review, graft tears in the dermal allograft and the autograft fascia lata were reported to be 13.9% overall [25]. A wide range of failure rates has been reported, depending on the type of graft: 5%–32% for the fascia lata autograft and 20%–70% for the human dermal allograft. Irrespective of the tissue source, the clinical results after 12 months postoperatively were reported to be excellent [26]. The present preliminary study successfully demonstrated acceptable functional results with a relatively low re-tear rate (2/34, 5.9%).
For irreparable posterosuperior RCTs, similar procedures have been reported so far (Morihara et al. [14] and Yokoya et al. [27]). Except for the presence of fascial continuity to the surrounding muscles, these two procedures consistently comprise the following techniques: (1) release of the supraspinatus from the supraspinatus fossa; (2) release of the ISP from the ISP fossa; and (3) attachment of these released muscles to the original location. Specifically, the ISP rotation exclusively included the ISP release, after which this tendon was rotated toward the superior to the middle facet because of the supraspinatus tendon’s irreparability. In our series, the overall re-tear rate was 5.9%, which decreased to 2.9% when the fatty infiltration level in ISP was Goutallier’s stage 3 or less.
IRT uses a relatively low tension at the repair site since the ISP is freed from its attached area and advanced to the footprint. However, re-tearing occurred in 2 of the 34 cases after surgery (5.9%). These results indicate that biological factors of tendon/bone (other than tension) affected the postoperative re-tear rate. Shirachi et al [28]. showed that the procollagen type I and III mRNA expression level at the edge of the ruptured rotator cuff tendon was significantly correlated with the postoperative rotator cuff integrity. Clinical research has also reported that a high signal intensity at the tendon edge on MRI is associated with a high possibility of re-tearing after surgery [29]. The levels of mesenchymal stem cells present in the greater tuberosity of patients with a RCT decreases as a function of a number of clinical factors, including the lag time from the tear onset to the treatment, the tear size, the number of tears, and the stage of fatty infiltration, among others [30]. Thus, biological intervention in the tendon-bone interface may further enhance the healing rate after IRT.
Some limitations were present in this study. First, the study was a retrospective cohort type, where the 1-year postoperative follow-up was conducted with only a few cases. Second, no biomechanical or anatomical support for the Asato technique (the IRT) was found. Finally, this study did not include a control group. However, we believe our preliminary study is worth reporting because no report currently exists like those described in this study.
In conclusion, this preliminary study examined the clinical outcomes of the IRT technique for irreparable RCTs. At 1 year postoperatively, the clinical scores significantly improved, and the re-tear rate was low at 5.9%. Further follow-up studies are needed to determine whether the ISP muscle works as well as the original external rotators after being advanced using the IRT technique.
Fig. 1.
(A) A massive rotator cuff tear in the right shoulder of a 73-year-old man. Viewed from the posterolateral portal. (B) After mobilization of the infraspinatus (ISP), the three stay sutures placed at the tendon’s edge were pulled antero-superiorly. However, the tendon stumps failed to reach the footprint beyond the anatomical neck of the humerus. (C) After rotational ISP transfer. Once released from the surrounding tissues by the “rotational ISP transfer” technique, the ISP tendon’s edge was fixed using the suture bridge technique. SSP: supraspinatus, SF: superior facet, MF: middle facet.
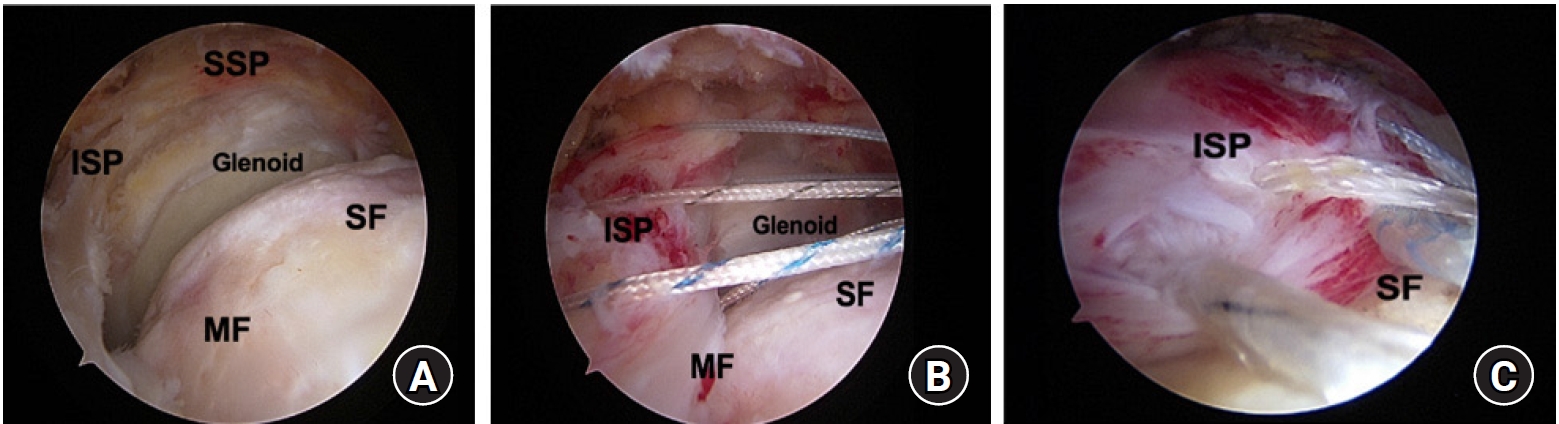
Fig. 2.
Scheme of rotational infraspinatus (ISP) transfer. (A) The ISP was released from the surrounding tissues. White lines indicate the margin between the ISP and the surrounding tissue. (B) Anterosuperior advancement of the released ISP (white arrow). SSP: supraspinatus.
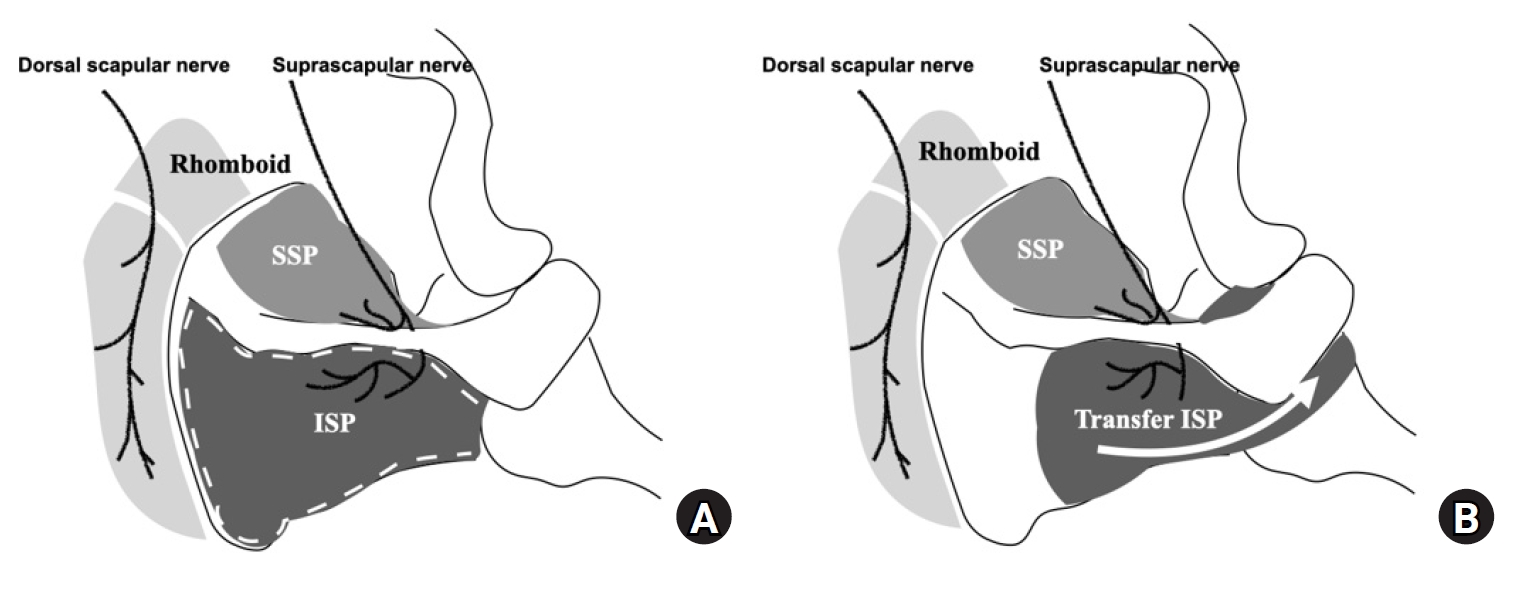
Table 1.
Patient demographics
Table 2.
Clinical outcomes
Values are presented as mean±standard deviation.
UCLA: University of California at Los Angeles, JOA: Japanese Orthopaedic Association, ASES: American Shoulder and Elbow Surgeons, WORC: Western Ontario Rotator Cuff Index, Shoulder 36: JOA shoulder 36 score, ROM: range of motion, ADL: activities of daily living, ER: external rotation, IR: internal rotation.
REFERENCES
1. Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med 2012;31:589–604.


2. Rees JL. The pathogenesis and surgical treatment of tears of the rotator cuff. J Bone Joint Surg Br 2008;90:827–32.


3. Jain NB, Ayers GD, Fan R, Kuhn JE, Warner JJ, Baumgarten KM, et al. Comparative effectiveness of operative versus nonoperative treatment for rotator cuff tears: a propensity score analysis from the ROW cohort. Am J Sports Med 2019;47:3065–72.



4. Song A, DeClercq J, Ayers GD, et al. Comparative time to improvement in nonoperative and operative treatment of rotator cuff tears. J Bone Joint Surg Am 2020;102:1142–50.


5. Piper CC, Hughes AJ, Ma Y, Wang H, Neviaser AS. Operative versus nonoperative treatment for the management of full-thickness rotator cuff tears: a systematic review and meta-analysis. J Shoulder Elbow Surg 2018;27:572–6.


6. Malahias MA, Kostretzis L, Chronopoulos E, Brilakis E, Avramidis G, Antonogiannakis E. Arthroscopic partial repair for massive rotator cuff tears: does it work? A systematic review. Sports Med Open 2019;5:13.



7. Namdari S, Voleti P, Baldwin K, Glaser D, Huffman GR. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a systematic review. J Bone Joint Surg Am 2012;94:891–8.

8. Shin JJ, Saccomanno MF, Cole BJ, Romeo AA, Nicholson GP, Verma NN. Pectoralis major transfer for treatment of irreparable subscapularis tear: a systematic review. Knee Surg Sports Traumatol Arthrosc 2016;24:1951–60.


9. Clouette J, Leroux T, Shanmugaraj A, et al. The lower trapezius transfer: a systematic review of biomechanical data, techniques, and clinical outcomes. J Shoulder Elbow Surg 2020;29:1505–12.


10. Mihata T, Lee TQ, Watanabe C, et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy 2013;29:459–70.


11. Stewart RK, Kaplin L, Parada SA, Graves BR, Verma NN, Waterman BR. Outcomes of subacromial balloon spacer implantation for massive and irreparable rotator cuff tears: a systematic review. Orthop J Sports Med 2019;7:2325967119875717.



12. Kovacevic D, Suriani RJ Jr, Grawe BM, et al. Management of irreparable massive rotator cuff tears: a systematic review and meta-analysis of patient-reported outcomes, reoperation rates, and treatment response. J Shoulder Elbow Surg 2020;29:2459–75.



13. Warner JJ. Management of massive irreparable rotator cuff tears: the role of tendon transfer. Instr Course Lect 2001;50:63–71.

14. Morihara T, Kida Y, Furukawa R, et al. Therapeutic outcomes of muscular advancement by an arthroscopic-assisted modified Debeyre-Patte procedure for irreparable large and massive rotator cuff tears. J Orthop Sci 2018;23:495–503.


15. Asato H, Teruya H, Kanaya F. Clinical results of infraspinatus muscle transfer for massive irreparable rotator cuff repair. Katakansetsu 2010;34:445–9.
16. Davidson J, Burkhart SS. The geometric classification of rotator cuff tears: a system linking tear pattern to treatment and prognosis. Arthroscopy 2010;26:417–24.


17. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures: pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994;(304):78–83.

18. Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. a prospective outcome study. J Bone Joint Surg Am 2007;89:953–60.

19. Mochizuki T, Sugaya H, Uomizu M, et al. Humeral insertion of the supraspinatus and infraspinatus. New anatomical findings regarding the footprint of the rotator cuff. J Bone Joint Surg Am 2008;90:962–9.


20. Lobao MH, Melvani RT, Abbasi P, Parks BG, Murthi AM. Dermal allograft superior capsule reconstruction biomechanics and kinematics. J Shoulder Elbow Surg 2021;30:2156–65.


21. Lobao MH, Canham RB, Melvani RT, Abboud JA, Parks BG, Murthi AM. Biomechanics of biodegradable subacromial balloon spacer for irreparable superior rotator cuff tears: study of a cadaveric model. J Bone Joint Surg Am 2019;101:e49.

22. Elhassan BT, Sanchez-Sotelo J, Wagner ER. Outcome of arthroscopically assisted lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tears. J Shoulder Elbow Surg 2020;29:2135–42.


23. Kany J, Grimberg J, Amaravathi RS, Sekaran P, Scorpie D, Werthel JD. Arthroscopically-assisted latissimus dorsi transfer for irreparable rotator cuff insufficiency: modes of failure and clinical correlation. Arthroscopy 2018;34:1139–50.


24. Kany J, Sekakaran P, Amavarathi RS, et al. Posterior latissimus dorsi transfer for massive irreparable posterosuperior rotator cuff tears: does it work in the elderly population? A comparative study between 2 age groups (≤55 vs. ≥75 years old). J Shoulder Elbow Surg 2021;30:641–51.


25. Smith TJ, Gowd AK, Kunkel J, et al. Clinical outcomes of superior capsular reconstruction for massive, irreparable rotator cuff tears: a systematic review comparing acellular dermal allograft and autograft fascia lata. Arthrosc Sports Med Rehabil 2020;3:e257–68.



26. de Campos Azevedo CI, Andrade R, Leiria Pires Gago Ângelo AC, Espregueira-Mendes J, Ferreira N, Sevivas N. Fascia lata autograft versus human dermal allograft in arthroscopic superior capsular reconstruction for irreparable rotator cuff tears: a systematic review of clinical outcomes. Arthroscopy 2020;36:579–91.e2.


27. Yokoya S, Nakamura Y, Harada Y, Ochi M, Adachi N. Outcomes of arthroscopic rotator cuff repair with muscle advancement for massive rotator cuff tears. J Shoulder Elbow Surg 2019;28:445–52.


28. Shirachi I, Gotoh M, Mitsui Y, et al. Collagen production at the edge of ruptured rotator cuff tendon is correlated with postoperative cuff integrity. Arthroscopy 2011;27:1173–9.










