Short-term outcomes of two-stage reverse total shoulder arthroplasty with antibiotic-loaded cement spacer for shoulder infection
Article information
Abstract
Background
The purpose of our study was to investigate short-term outcomes of two-stage reverse total shoulder arthroplasty (RTSA) with an antibiotic-loaded cement spacer for shoulder infection.
Methods
Eleven patients with shoulder infection were treated by two-stage RTSA following temporary antibiotic-loaded cement spacer. Of the 11 shoulders, nine had pyogenic arthritis combined with complex conditions such as recurrent infection, extensive osteomyelitis, osteoarthritis, or massive rotator cuff tear and two had periprosthetic joint infection (PJI). The mean follow-up period was 29.9 months (range, 12–48 months) after RTSA. Clinical and radiographic outcomes were evaluated using the visual analog scale (VAS) score for pain, American Shoulder and Elbow Surgeons (ASES) score, subjective shoulder value (SSV), and serial plain radiographs.
Results
The mean time from antibiotic-loaded cement spacer to RTSA was 9.2 months (range, 1–35 months). All patients had no clinical and radiographic signs of recurrent infection at final follow-up. The mean final VAS score, ASES score, and SSV were significantly improved from 4.5, 38.6, and 29.1% before RTSA to 1.7, 75.1, and 75.9% at final follow-up, respectively. The mean forward flexion, abduction, external rotation, and internal rotation were improved from 50.0°, 50.9°, 17.7°, and sacrum level before RTSA to 127.3°, 110.0°, 51.8°, and L2 level at final follow-up, respectively.
Conclusions
Two-stage RTSA with antibiotic-loaded cement spacer yields satisfactory short-term clinical and radiographic outcomes. In patients with pyogenic arthritis combined with complex conditions or PJI, two-stage RTSA with an antibiotic-loaded cement spacer would be a successful approach to eradicate infection and to improve function with pain relief.
INTRODUCTION
The shoulder joint is the third most common location for pyogenic arthritis following knee and hip joints [1]. It can be devastating and difficult to treat because the joint can be rapidly destroyed [2]. Standard management options have included open or arthroscopic irrigation, and debridement in conjunction with antibiotic treatment [2]. However, these classic approaches result in a higher failure rate of infection control with unsatisfactory outcomes when dealing with a combined complex condition such as osteomyelitis with joint destruction, massive rotator cuff tear, or advanced degenerative osteoarthritis. Upon systematic review, Memon et al. [1] reported a 28% revision rate and 21% complication rate after primary debridement in pyogenic arthritis of the shoulder.
Successful management of shoulder infection is more difficult to achieve in certain circumstances, including recurrent infection, massive rotator cuff tear, destruction of the joint, or the presence of internal fixation device or prosthesis. Particularly, periprosthetic joint infection (PJI) of the shoulder is one of the most devastating complications for orthopedic surgeons despite rare incidence of 1% to 4% [3-5]. An ideal treatment should secure successful eradication of infection and provide functional restoration with pain relief. Therefore, more aggressive treatment is crucial in these conditions. However, optimal treatment of pyogenic arthritis combined with complex conditions and PJI of the shoulder is not as well established as that in hip and knee joints [6]. For these reasons, treatment options for shoulder infection have been modeled on the management of hip and knee infections, and include antibiotic therapy, open or arthroscopic debridement, resection arthroplasty, and one-stage or two-stage implantation. Among these variety of options, the two-stage approach with temporary antibiotic-loaded cement spacer is well known as one of the standard options in hip and knee infections, and has become a procedure of interest for the treatment of shoulder infection [7,8]. Recently, several studies reported promising results using a two-stage reverse total shoulder arthroplasty (RTSA) with antibiotic-loaded cement spacers in the treatment of primary pyogenic arthritis, as well as PJI of the shoulder [9-12]. However, reports about the treatment of primary pyogenic arthritis using this modality are limited with a small number of patients [9].
The purpose of our study was to investigate short-term outcomes of two-stage RTSA with antibiotic-loaded cement spacer for shoulder infection. We hypothesized that two-stage RTSA with an antibiotic-loaded cement spacer would be a useful option to eradicate infection and to improve function with pain relief in patients with pyogenic arthritis combined complex conditions or PJI.
METHODS
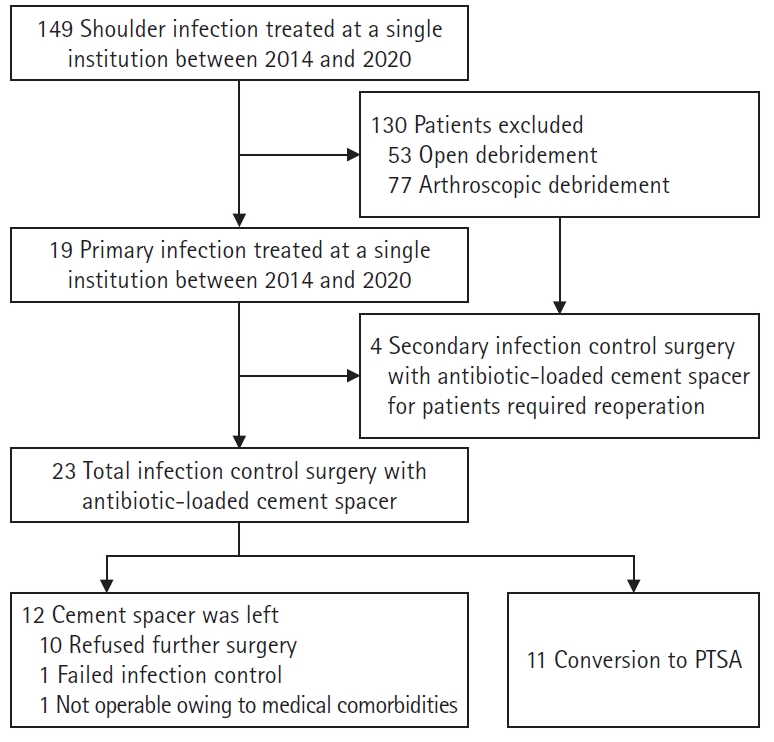
The present study was approved by the Institutional Review Board of Keimyung University Dongsan Hospital with exemption of informed consent (IRB No. 2021-05-082). Informed consent was obtained from the patients for the use of the photographs. We retrospectively reviewed 23 patients who underwent infection control surgery with antibiotic-loaded cement spacer for shoulder infection at a single institution between 2014 and 2020. Indications for infection control surgery with antibiotic-loaded cement spacer included PJI and pyogenic arthritis combined with complex conditions such as recurrent infection, extensive osteomyelitis, advanced degenerative osteoarthritis, or massive rotator cuff tear. Inclusion criteria in this study were as follows: (1) RTSA for the second stage procedure, (2) available medical records and radiographic findings, (3) and a follow-up period more than 12 months after RTSA. Twelve patients with retained cement spacer were excluded, including nine patients that had no infection sign, but refused further surgery, one patient had uncontrolled infection, and one patient was not operable owing to medical reasons. Finally, 11 patients were included in this study (Fig. 1).
Infection was diagnosed based on clinical presentation (erythema, warmth, swelling, tenderness, fever), laboratory markers (white blood cell counts, C-reactive protein, and erythrocyte sedimentation rate), joint fluid analysis, radiographic evaluations (plain radiographs, enhanced magnetic resonance imaging), and tissue culture or biopsy [11].
Surgical Technique
For the first stage, extensive debridement and bone curettage or removal of infected prosthesis was performed by a single surgeon (CHC). After thorough debridement, the humeral head was cut along anatomical neck and the medullary canal was reamed. A hand-made cement spacer loaded with 4 g of vancomycin and a 2.4 mm Steinmann pin was implanted. The mean duration of intravenous antibiotic therapy after infection control surgery was 3.7 weeks (range, 2–7 weeks). The following oral antibiotic therapy was used according to numerical values of serum inflammatory markers. For the second stage, conversion criteria to RTSA included: (1) no clinical symptoms and signs including resting pain, swelling, warmth, and erythema, (2) no radiographic signs of infection by plain radiographs and follow-up enhanced magnetic resonance imaging before conversion to RTSA (3) normalization of inflammatory markers at least three times, (4) intraoperative frozen biopsy or surgeon’s assessment. The criterion suggested by Mirra et al. [13] was used, in which <5 neutrophils per high-power field of frozen biopsy sample was considered negative. The Equinoxe Reverse Shoulder System (Exactech, Gainesville, FL, USA) was used in ten shoulders and the Delta Xtend Reverse Shoulder System (Dephy, Warsaw, IN, USA) in one shoulder. The mean time from antibiotic-loaded cement spacer to RTSA was 9.2 months (range, 1–35 months).
Outcome Assessment
The mean follow-up period after conversion to RTSA was 29.9 months (range, 12–48 months). No recurrence of infection was defined as the absence of any clinical signs of infection, normal values of inflammatory markers, and the absence of progressive radiolucency on serial plain radiographs. Clinical outcomes were evaluated using the visual analog scale (VAS) score for pain, American Shoulder and Elbow Surgeons (ASES) score, subjective shoulder value (SSV), and active range of motion (ROM) of the shoulder joint. Radiographic outcomes were evaluated using serial plain radiographs. Radiolucency around prosthesis was classified using the systems described by Gilot et al. [14].
Statistical Analysis
Statistical analysis was performed using SPSS ver. 20.0 (IBM Corp., Armonk, NY). The difference between clinical outcomes before RTSA and after RTSA were assessed using the Mann-Whitney test. A p-value <0.05 was considered statistically significant.
RESULTS
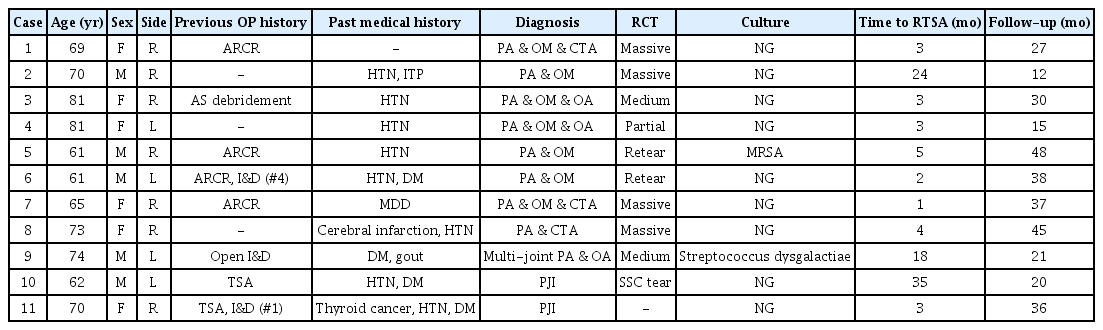
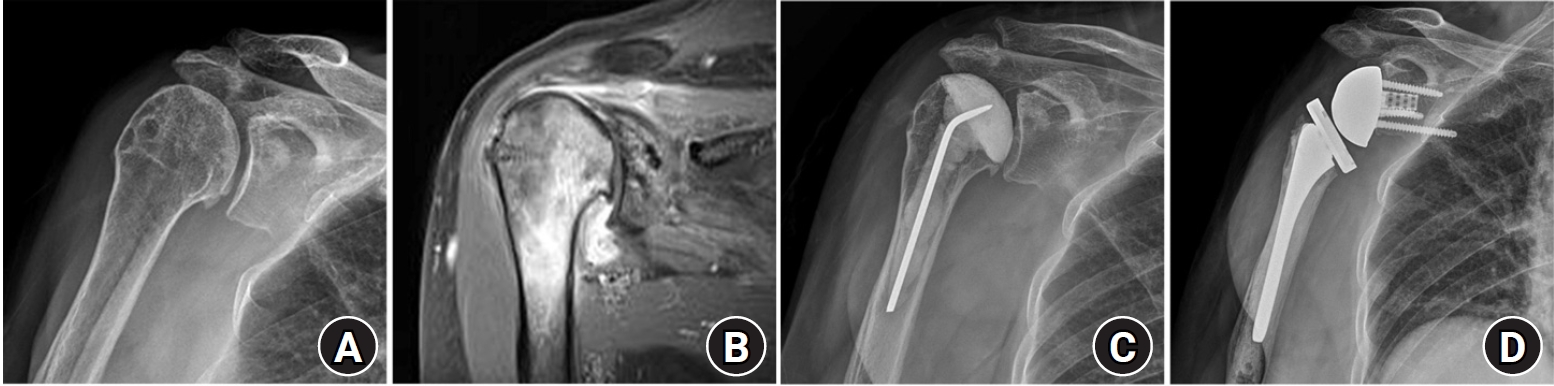
The mean age of patients was 69.7±7.2 (range, 61–81 years). There were six women and five men. Before infection control surgery with antibiotic-loaded cement spacer, three patients had recurrent infection and two patients had PJI. Among the remaining six patients with primary pyogenic arthritis combined complex conditions, three patients had cuff tear arthropathy, two patients had extensive osteomyelitis with joint destruction, and one patient had osteomyelitis with advanced degenerative osteoarthritis. Eight patients had a history of previous surgery, including four arthroscopic rotation cuff repair, two total shoulder arthroplasty, one arthroscopic debridement, and one open debridement for pyogenic arthritis (Table 1). According to enhanced magnetic resonance imaging, all patients had rotator cuff tear with or without degenerative arthritis. Intraoperative histopathology revealed acute or chronic inflammation consistent with infection in all shoulders, but positive culture was found in two shoulders at the time of infection control surgery with antibiotic-loaded cement spacer, including methicillin-resistant staphylococcus aureus (MRSA) and Streptococcus dysgalactiae. In nine shoulders, no organism was found in any culture from joint aspiration and intraoperative specimen.
At final follow-up evaluation after RTSA, no clinical and radiographic signs of recurrent infection were observed in all patients. The mean VAS pain score was significantly improved from 4.5±2.3 before RTSA to 1.7±1.6 at final follow-up (p<0.001). Three patients had no pain, six had mild pain, and two had moderate pain. The mean ASES score was significantly improved from 38.6±16.3 before RTSA to 75.1±16.2 at final follow-up (p<0.001). The mean SSV was significantly improved from 29.1%±17.6% before RTSA to 75.9%±16.9% at final follow-up (p<0.001). The mean forward flexion, abduction, external rotation, and internal rotation values were improved from 50.0°±31.9°, 50.9°±30.8°, 17.7°±16.9°, and sacrum level before RTSA to 127.3°±34.1°, 110.0°±38.2°, 51.8°±14.7°, and L2 level at final follow-up, respectively (p<0.05) (Table 2).
Based on the serial plain radiographs, proximal bone resorption by stress shielding was found in two patients (18.1%) and scapular notching was found in two patients (18.1%). No progressive osteolysis was observed around the prosthesis. Two complications (18.1%) among 11 patients were observed, including two periprosthetic humeral fractures. Case 5 with spiral fracture around the stem tip underwent open reduction and internal fixation at 32 months after RTSA. Case 10 had a transverse fracture around the stem tip at 21 months after RTSA and underwent conservative management because of medical comorbidities. At the final follow-up evaluation, both patients had poor clinical outcomes in spite of fracture healing.
DISCUSSION
The present study revealed that two-stage RTSA with an antibiotic-loaded cement spacer yields satisfactory short-term clinical and radiographic outcomes. In all patients, infection was successfully eradicated by infection control surgery using an antibiotic-loaded cement spacer. No clinical or radiographic signs of recurrent infection after two-stage RTSA were observed at final follow-up evaluation. The results presented here indicate that two-stage RTSA with an antibiotic-loaded cement spacer is an effective treatment option for pyogenic arthritis combined with complex conditions such as recurrent infection, extensive osteomyelitis, osteoarthritis, or massive rotator cuff tear, as well as PJI.
Although numerous treatment modalities for PJI of the shoulder have been reported, including long-term use of antibiotics, open or arthroscopic debridement, resection arthroplasty, one-stage implantation, and two-stage implantation, the optimal strategy is still controversial. Use of antibiotics with or without debridement has shown high rates (up to 65%) of recurrent infection that leads surgeons to look for alternative treatment options [3,15]. Resection arthroplasty leads to poor function with residual pain in up to 50% of patients, because the surrounding soft tissues can be irritated by the residual stump during movements [3,16]. Furthermore, it may compromise the potential for revision arthroplasty due to arm shortening, soft tissue adhesion around the joint, weak bone stock, and rotator cuff insufficiency [17]. The rates of recurrent infection after resection arthroplasty have also been reported up to 30% [3,15]. The one-stage procedure consists of extensive debridement of infected tissue with re-implantation of prosthesis after removal of all implants in the simultaneous step. Beekman et al. [18] reported on 11 shoulders with an infected RTSA treated using one-stage revision RTSA method. They concluded that this approach provides satisfactory results with reliable infection control rate and low cost and duration of treatment. Although this approach included several advantages such as a single anesthesia, low cost, and short hospital stay, surgeons may be afraid of recurrent infection after one-stage revision arthroplasty and may prefer a two-stage procedure that can yield more reproducible rates of infection control.
A two-stage approach with use of a temporary antibiotic-loaded cement spacer has been also used in infected shoulders as a common procedure proven by numerous studies for treatment of hip and knee infections [7-12]. The first stage in this approach consists of thorough irrigation and extensive debridement with implant removal if present, followed by subsequent insertion of a temporary antibiotic-loaded cement spacer with intravenous antibiotic therapy. The second stage is a delayed revision arthroplasty after eradication of infection. Despite the fact that it is difficult to directly translate strategy from hip or knee infection to shoulder infection, the shoulder joint has limited weight-bearing demands compared with the lower extremity [12]. In addition, the patients may tolerate a reduced ROM, because of the ability to compensate with use of the contralateral upper extremity [12,15]. Therefore, this strategy has been shown successfully in the shoulder as well, although published prior studies are not abundant [3,19]. Sperling et al. [3] found recurrent infection in 50% of patients who underwent a one-stage revision for PJI compared to 0% with two-stage revision group at a mean follow-up period of 6.5 years.
In addition, recurrent shoulder infection or primary pyogenic arthritis with combined complex conditions such as extensive osteomyelitis, advanced degenerative osteoarthritis, or massive rotator cuff tear are challenging to treat. Arthroscopic or open debridement for these conditions may result in a high failure rate of infection control. Although RTSA was usually performed in patients with rotator cuff insufficiency, its indications have been consistently expanded with successful outcomes [20,21]. Recently, promising results using a two-stage RTSA with an antibiotic-loaded cement spacer have been reported for the treatment of primary pyogenic arthritis, as well as PJI of the shoulder [9-12].
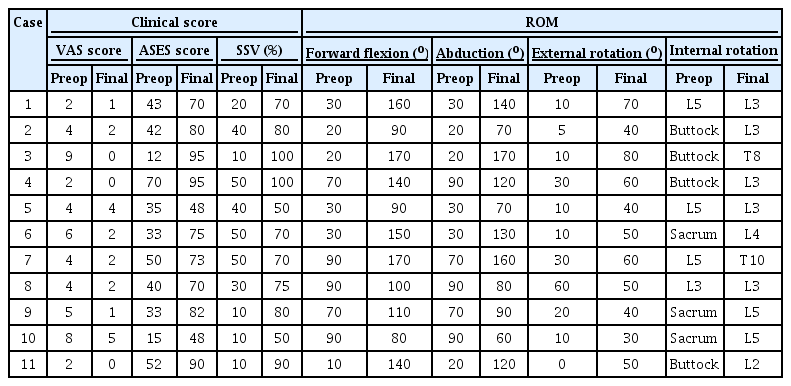
In the present study, two-stage RTSA with an antibiotic-loaded cement spacer was performed in nine pyogenic arthritis patients with combined complex conditions (Figs. 2 and 3) and two PJI (Figs. 4 and 5). All patients had rotator cuff tear with or without degenerative arthritis. As the first stage, we performed massive irrigation and extensive debridement of the soft tissue and bone. A cement spacer loaded with 4 g of vancomycin and a 2.4-mm Steinmann pin was made and inserted as similar as possible with the cutting head. We believe that this procedure can make further revision RTSA easier by reserving joint space and preventing contracture of surrounding soft tissues. For the second stage, we strictly keep the criteria for RTSA conversion, including no clinical and radiographic signs of infection, normalization of inflammatory markers, and intraoperative frozen biopsy. At final follow-up evaluation, all patients had no clinical and radiographic signs of recurrent infection after RTSA. The present study demonstrated two-stage RTSA with an antibiotic-loaded cement spacer yields satisfactory short-term clinical and radiographic outcomes.
Case 1. A 69-year-old woman with previous history of rotator cuff repair. Plain radiograph and magnetic resonance imaging show pyogenic arthritis with osteomyelitis and cuff tear arthropathy (A, B). (C) Plain radiograph shows an antibiotic-loaded cement spacer for infection control. (D) Plain radiograph shows reverse total shoulder arthroplasty performed at 3 months after infection control surgery.

Case 1. Plain radiograph at 27 months after reverse total shoulder arthroplasty shows proximal humeral bone resorption without any sign of implant loosening (A). Clinical photos at final follow-up show function restoration with pain relief (B-D).
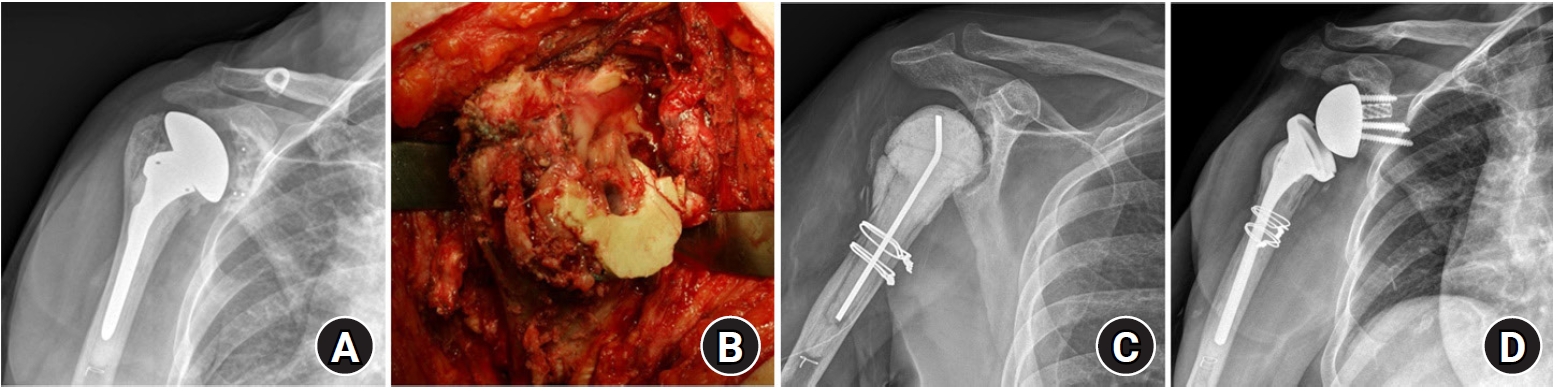
Case 10. A 70-year-old woman with infected total shoulder arthroplasty. Plain radiograph before infection control surgery shows glenoid component loosening with radiolucency (A). Intraoperative photo revealed dirty granulation tissue with pus-like joint fluid (B). Plain radiograph shows antibiotic-loaded cement spacer with implant removal for infection control (C). Plain radiograph shows reverse total shoulder arthroplasty performed at three months after infection control surgery (D).
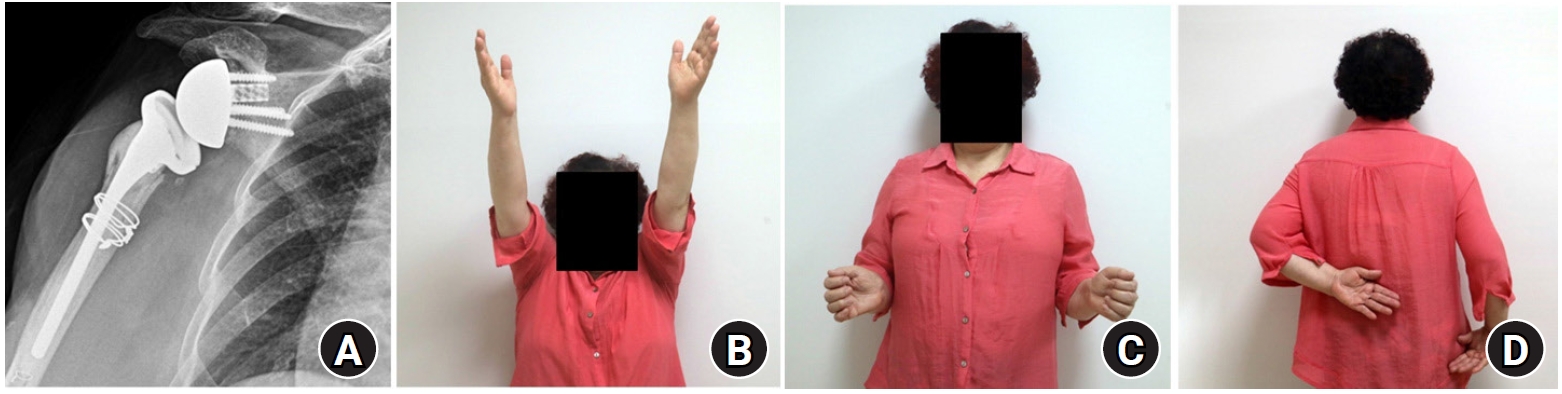
Case 10. Plain radiograph at 36 months after RTSA shows no evidence of radiolucency or implant loosening (A). Clinical photos at final follow-up show function restoration with pain relief (B-D).
Several studies reported MRSA and staphylococcus epidermidis were the most frequently cultured organisms in patients with shoulder infection [5,22]. However, other studies reported a high incidence of positive culture for Cutibacterium acnes in patients with PJI of the shoulder. Buchalter et al. [12] reported on 19 cases with PJI treated by two-stage revision arthroplasty. Eight (61.5%) among 13 positive cultures were C. acnes and the patients with C. acnes had higher rate of recurrent infection than those without C. acnes [12]. Recently, C. acnes is becoming recognized as a common pathogen in infected shoulder arthroplasty and requires prolonged incubation of cultures for recognition [11]. In the present study, MRSA and S. dysgalactiae were cultured in two shoulders and nine shoulders had negative cultures. A high rate of negative cultures might result from previous use of antibiotics because most patients were referred from local clinics. Also, we did not have positive culture for C. acnes in our cases. This result might be attributed to ethnicity and incubation period for the detection of C. acnes. East or southeast Asians had the lowest detection rate of C. acnes compared with all other ethnicities [23]. The incubation period for organisms was routinely three days only in our institute, although a 13–14 day incubation period is essential for the detection of C. acnes [24].
This study has several limitations. First, it was a retrospective study. Second, there was no control group of patients managed with other treatment modalities. Third, the number of patients was small with heterogeneous traits. As a result, subgroup analysis between primary and recurrent infection was not possible. Further prospective, large-scale, comparative studies are needed to clarify the efficacy of two-stage RTSA with antibiotic-loaded cement spacer for shoulder infection.
The present study revealed that two-stage RTSA with an antibiotic-loaded cement spacer yields satisfactory short-term clinical and radiographic outcomes. In patients with pyogenic arthritis combined with complex conditions or PJI, two-stage RTSA with an antibiotic-loaded cement spacer would be a successful approach to eradicate infection and to improve function with pain relief.
Notes
Financial support
None.
Conflict of interest
None.