Horizontal instability after acromioclavicular joint reduction using the two-hole technique is preferred over the loop technique: a single-blind randomized clinical trial
Article information
Abstract
Background
Most acromioclavicular joint (ACJ) injuries are caused by direct trauma to the shoulders, and various methods and techniques are used to treat them; however, none of the options can be considered the gold standard. This study examines the horizontal stability of the ACJ after a complete dislocation was repaired using one of two Ethibond suture techniques, the loop technique and the two holes in the clavicle technique.
Methods
In this single-blind, randomized clinical trial, 104 patients diagnosed with complete ACJ dislocation type V were treated using Ethibond sutures with either the loop technique or the two holes in the clavicle technique. Horizontal changes in the ACJ were radiographically assessed in the lateral axial view, and shoulder function was evaluated by the Constant (CS) and Taft (TS) scores at intervals of 3, 6, and 12 months after surgery.
Results
The horizontal stability of the ACJ was better with the two-hole technique than the loop technique at all measurement times. CS and TS changes showed a significant upward trend over time with both techniques. The mean CS and TS at the final visit were 95.2 and 11.6 with the loop technique and 94.0 and 11.9 with the two-hole technique, respectively. The incidence of superficial infections caused by the subcutaneous pins was the same in the two groups.
Conclusions
Due to the improved ACJ stability with the two-hole technique, it appears to be a more suitable option than the loop technique for AC joint reduction.
INTRODUCTION
The acromioclavicular joint (ACJ) is a diarthrodial joint located between the acromion and the clavicle and is supported by the AC and coracoclavicular (CC) ligaments. The AC ligament connects the acromion to the distal clavicle and provides the ACJ with horizontal (anterior–posterior) stability [1-3]. ACJ injury accounts for 9%–12% of shoulder injuries, is most common in people aged 20 to 30 years, and occurs five times more often in men than in women [1,2,4-6]. These injuries are often caused by direct trauma to the shoulder during contact sports (such as cycling, skiing, ice hockey, rugby, and soccer) when the arm is in an inclined position or when falling on an inclined arm [1,2,7,8]. ACJ injuries are usually classified by the Rockwood system into six types based on the damage to the AC and CC ligaments. Recommendations for managing these injuries are usually non-surgical for types I and II, surgical for types IV to VI, and controversial for type III [1,2,9].
More than 60 methods for treating ACJ injuries have been proposed in the literature, indicating disagreement about the best surgical procedure for treating them. Many of the methods focus on vertical instability (disruption of the CC ligaments). Horizontal instability (AC ligament disruption) has received less attention [1,9,10]. There is currently no gold standard surgical treatment for any type of AC injury, especially for horizontal ACJ instability [4,8,10,11]. This study examined the effects of two Ethibond suture techniques, the loop technique and the two holes in the clavicle technique, on the horizontal stability of the ACJ following its complete dislocation. These techniques were used because they are cheaper for patients than other techniques in our country.
METHODS
This study was approved by the University Ethics Committee (IR.GUMS.REC.1395.307) and is registered at the Iranian Registry of Clinical Trials (IRCT201704087274N12). All patients signed the consent form, and their personal information was kept confidential.
Study Design
This study was a single-blind, randomized, clinical trial with a parallel design conducted at a referral university hospital. A total of 104 patients aged 18–65 years were included in the study by convenience sampling from 2017 to 2019 after providing informed consent and receiving a thorough examination. The clinical part of the examination looked for symptoms such as hematoma or abrasion on the superolateral border of the shoulder or obvious asymmetry between the two distal clavicle ends, along with tenderness to the touch or positive piano-key sign. A radiographic evaluation was performed in the lateral axial view. Patients diagnosed with acute ACJ dislocation (for less than 3 weeks) of grade V in the Rockwood classification and treated with surgery by the first author were included in the study. Those with chronic dislocation, a history of shoulder joint trauma or associated lesions in the affected arm, psychological disorders, or alcohol or drug abuse were excluded.
Based on the results of previous studies [12] and considering a 95% confidence level and 90% test power, the required sample size was calculated to be 52 per group. Using a 1:1 ratio for the randomized block design, the eligible individuals were randomly allocated into the two Ethibond suture groups, the loop technique or the two holes in the clavicle technique. The website https://www.sealedenvelope.com was used to generate a randomization list for allocating the 104 patients to the study groups in randomized blocks of four. After generating the list, each person was assigned a unique code and identified with that code during the study. All participants were blinded to the randomization list; to ensure blinding, consecutively numbered sealed envelopes were used during the randomization process, and the envelope pertaining to each person was opened only after confirming the candidate’s eligibility and receiving their signed consent form. The study was single-blind; the subjects were blinded to the type of intervention they received.
Study Groups
The two-hole group
In this group, two holes, 1 cm apart, were made from the superior to the inferior part of the clavicle. An Ethibond 5 suture was divided into two layers, passed through the one hole, and looped around the coracoid to exit through the second hole. After an open ACJ reduction, the sutures were tied together, and the ACJ was stabilized with an additional flat pin from the acromion to the clavicle. The ACJ capsule was then repaired.
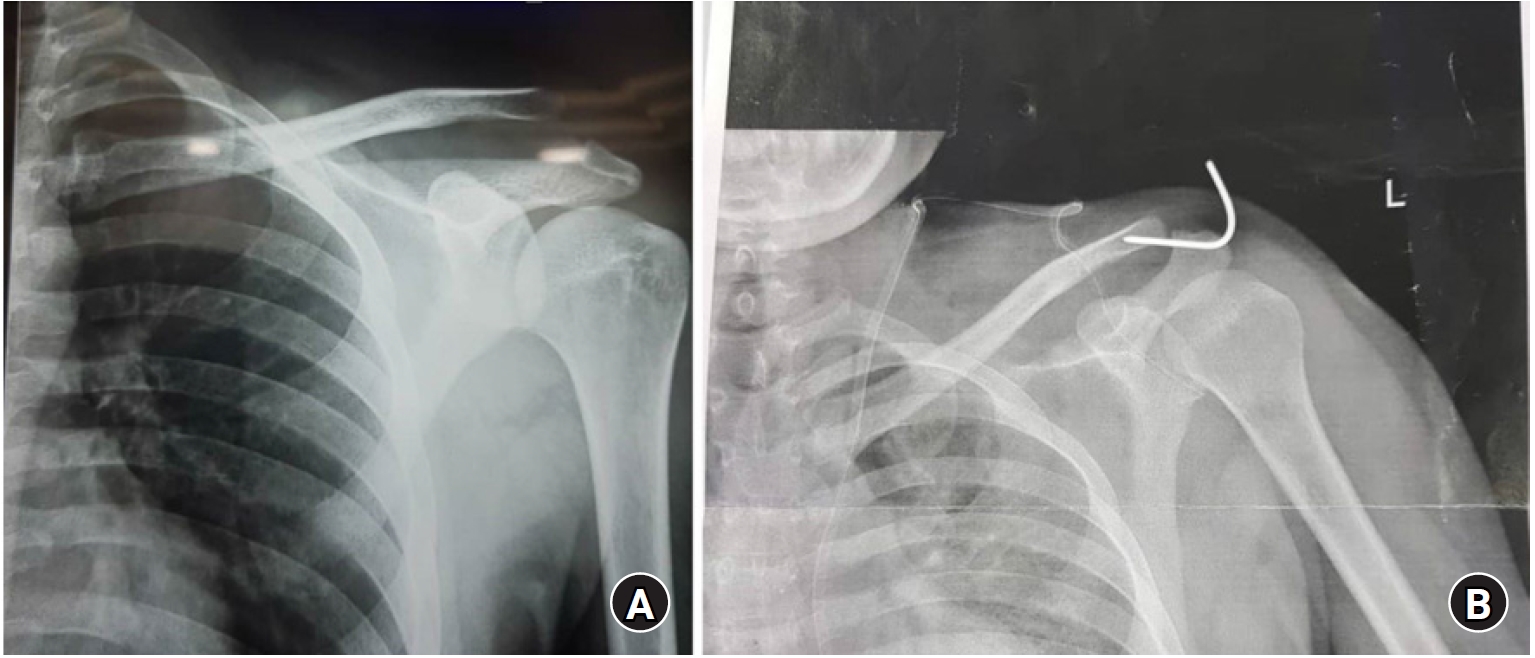
The loop group
In this group, the anchor suture was looped around the clavicle and coracoid bone instead of passing through a drilled tunnel, and the two ends of the suture were tied together while open ACJ reduction was being performed. As in the other group, the ACJ was stabilized with an additional flat pin from the acromion to the clavicle, and then the ACJ capsule was repaired (Figs. 1 and 2).
Rehabilitation Protocol
After the operation, the limbs were slinged for 2 weeks in both groups, and the patients were allowed to resume normal daily activities until the 6th week. In both groups, after 6 weeks, the subcutaneous pin was removed under local anesthesia, and patients were sent to physiotherapy and allowed further activities. After 3 months, patients were allowed to perform heavy activities, such as lifting, pushing, and pulling.
Data Collection
Data on the patients’ demographic characteristics (age and sex) and operation-site infections (serous or pus secretion) were recorded in a checklist. Horizontal stability of the ACJ was recorded by an X-ray device, and shoulder function was recorded by the Constant (CS) and Taft (TS) at 3, 6, and 12 months post-surgery.
Radiographic Evaluation
For the horizontal ACJ evaluation, axillary radiographs were produced. By measuring the distance between the anterior edge of the acromion and the anterior edge of the lateral clavicle, the dislocation was categorized as stable (≤2 mm) or unstable (>2 mm) (Fig. 3) [13-15].
Statistical Analysis
The collected data were analyzed in IBM SPSS ver. 21 (IBM Corp., Armonk, NY, USA) software. The chi-square test was used to compare changes between the two groups in shoulder position as shown on horizontal radiography. Repeated-measures analysis of variance (ANOVA) was used to evaluate the changes in CS and TS before and after surgery, following a normal distribution assessment with Shapiro-Wilk’s test. The independent T-test was used for comparisons between the two groups and to compare the age variable. The chi-square test was applied to compare the qualitative variables (sex and infection) between the two groups. A p<0.05 represented statistical significance for all tests.
RESULTS
A total of 104 patients entered the study, but two patients were excluded from the two-hole group due to unavailability. Therefore, 50 patients in the two-hole group and 52 patients in the loop group were evaluated. Among the patients undergoing surgery, 79.4% were male. The mean age of the patients was 29.2±5.5 years. The sex distribution (p=0.526) and mean age (p=0.116) of patients did not differ significantly between the two techniques. The percentage of superficial infections in the form of mild discharge from the wound was 25% (n=13) in the loop group and 30% (n=15) in the two-hole group, which was a not significant difference (p=0.06). Each group had one case of loss of reduction, and the loop group had one case of painful ACJ (Fig. 4).
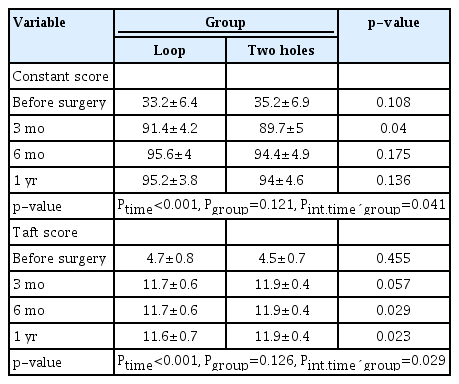
As shown in Table 1, changes in the horizontal stability of the shoulder differed significantly with the two methods (p<0.05) at all the measurement times (3, 6, and 12 months post-surgery), and the incidence of unstable cases with the loop technique was higher than that with the two-hole technique. Repeated-measure ANOVA results are shown in Table 2, along with the effect of time on the scores in the two groups. The CS and TS changes show a significant upward trend over time with both techniques (ptime<0.001). The group effect on the CS (pgroup=0.121) and TS (pgroup=0.126) was not statistically significant, indicating that the two techniques did not differ. The interaction between time and group for the CS and TS was significant, and those changes were statistically different at some intervals. However, the mean difference was not clinically significant.

Comparison of horizontal changes in shoulder position between the loop and two-hole methods at three measurement times
DISCUSSION
The results show a higher degree of horizontal instability with the loop technique than the two-hole technique. Twelve months after surgery, instability was found in 26.9% of the loop group and 8% of the two-hole group (17.6% overall). The changes in shoulder function reported in the CS and TS were similar with the two techniques. Also, the incidence of superficial infections caused by the subcutaneous pins was the same in the two groups. In this study, horizontal dislocations and joint instability were lower in the two-hole group; at 1-year postoperation, instability was more than three times more common in the loop group than the two-hole group (26.9% vs. 8%). However, with the loop technique, additional instability did not occur after 6 months. In other words, joints treated with the loop technique maintained the stability they had achieved at 6 months after surgery. Although the rates of instability and dislocation differed between the two techniques, the resulting shoulder function did not differ between the groups. Kraus et al. [12] showed that instability existed after shoulder joint reduction for grade V injuries with the double-tightrope technique based on either the V-shaped or parallel drill hole method. Shoulder function did not differ with those two methods either, consistent with the findings of this study. In general, it can be argued that horizontal instability does not affect short- or medium-term shoulder function.
In a review of biomechanical and clinical studies, Jordan et al. [16] showed that simultaneous reconstruction of the ACJ and CC joint produces less horizontal instability than isolated CC reconstruction, although the clinical outcomes did not differ. In other words, horizontal instability appears not to affect the functional outcomes of the shoulder.
In the two-hole group in this study, two holes were made in the clavicle, and an Ethibond suture was passed through the holes and looped around the coracoid so that the two ends of the suture could be tied together. In contrast, in the loop technique, the Ethibond suture was looped around the clavicle and the coracoid. In general, passage of the suture through the holes in the clavicle appears to restrict it. In other words, if the clavicle is fixed by passing a suture through holes in its structure, movement restriction is increased, which reduces the horizontal instability of the clavicle. Beitzel et al. [17] also showed that horizontal instability is limited in CC ligament reconstruction using single or double tunneling, which confirms the results of this study, though their surgical procedural details differed from those used here.
Previous studies have shown that several methods can be used for ACJ reconstruction, and no consensus has been reached on the best methods for diagnosing, evaluating, and treating acute or chronic ACJ horizontal instability. Horizontal instability injuries are often overlooked or not well understood, complicating diagnosis and potentially leading to extensive complications and failure after surgical stabilization [1].
Regarding complications, because subcutaneous pins were used for both techniques in this study, mild infections with small secretions were observed in both groups and were controlled with antibiotics. In a study by Liu et al. [13], a patient developed a superficial wound infection 3 weeks after surgery, which healed after routine care. Theopold et al. [18] reported no intraoperative complications and generally no fractures in the clavicle or coracoid area based on radiological examinations. No postoperative infections or wound healing disorders occurred in their study. In a study by Bostrom Windhamre et al. [19], five superficial infections were reported and treated with oral antibiotics, which is comparable to the results in this study, in which 28 people developed superficial infections. In our study, each group had one case of loss of reduction, and the loop group had one case of painful ACJ. In the study of Tauber et al. [20], a vertical re-dislocation with complete loss of reduction and clinically relevant ACJ deformity was observed in four patients. In general, ACJ reconstruction with various surgical techniques appears to have limited and acceptable complications.
Although horizontal stability differed between the two groups over the course of 1 year, functional outcomes did not differ between the groups. A 1-year follow-up might be too short to evaluate shoulder function, and functional outcomes might vary with longer follow-up periods. Also, clavicle instability could cause ACJ arthritis in the long term. None of the participants in this study were professional athletes or relied heavily on shoulder use. Functional outcomes might also differ in those individuals depending on which of the two techniques is used, and that constitutes one of the limitations of this study.
Although functional outcomes did not differ significantly between the two-hole and loop techniques in the short- and medium-term, the improved horizontal stability of the ACJ with the two-hole method suggests that technique as a more suitable option for ACJ reduction.
Notes
Financial support
None.
Conflict of interest
None.