A modified method of augmented distal clavicle fracture osteosynthesis with a Fibertape coracoclavicular cerclage
Article information
Abstract
Background
Unstable distal clavicles experience high non-union rates, prompting surgeons to recommend surgery for more predictable outcomes. There is a lack of consensus on the optimal method of surgical fixation, with an array of techniques described in the literature. We describe an alternative method of fixation involving the use of a distal clavicular anatomical locking plate with Fibertape cerclage augmentation in our series of patients.
Methods
Nine patients (8 males and 1 female), with a mean age of 36 years, who sustained unstable fracture of the distal clavicle in our institution were treated with our described technique. Postoperative range of motion, functional and pain scores, and time to radiographic union were measured over a mean follow-up period of 10 months. Incidences of postoperative complications were also recorded.
Results
At the last patient consult, the mean visual analog scale score was 0.88±0.35, with a mean Disabilities of the Arm, Shoulder, and Hand (DASH) score of 1.46±0.87 and American Shoulder and Elbow Surgeons (ASES) score of 94.1±3.57. The mean range of motion achieved was forward flexion at 173°±10.6°, abduction at 173°±10.6°, and external rotation at 74.4°±10.5°. All patients achieved internal rotation at a vertebral height of at least L2 with radiographical union at a mean of 10 weeks. No removal of implants was required.
Conclusions
Our described technique of augmented fixation of the distal clavicle is effective, produces good clinical outcomes, and has minimal complications.
INTRODUCTION
Clavicle fractures are common, and while most such fractures occur at the mid shaft, approximately 15% involve the distal one-third [1]. The most common classification for distal one-third clavicle fractures is the Modified Neer system based on the fracture site’s relationship with the coracoclavicular (CC) ligament [2]. Unstable fractures, such as type 2 and type 5, often experience significant displacement due to deforming forces from the trapezius acting upon the proximal fragment along with the weight of the arm pulling the distal fragment inferiorly. As a result, these fractures experience high non-union rates [3,4], prompting surgeons to recommend surgery [5].
With a lack of consensus on the best surgical option, various techniques have been described, such as anatomical locking plates or hook plate fixation, CC stabilization (with a suture anchor, button device, or screw), Kirschner wire fixation, or arthroscopic assisted procedures. Each of these methods has advantages and shortcomings such as the need for implant removal or risk of intraoperative fractures [6]. The purpose of our study is to illustrate an alternative method of fixation involving the use of a distal clavicular anatomical locking plate with Fibertape cerclage augmentation in a series of patients. We hypothesize that our method of augmented fixation will be reliable and produce good outcomes with minimal complications.
METHODS
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Ethics Committee of National Health Group (No. NHG 2020/00202). Patient records and radiographs were retrospectively accessed through the patient's electronic medical records upon Institutional Review Board approval.
Nine patients who sustained unstable fracture of the distal clavicle treated by distal clavicle locking plates along with Fibertape (Arthrex, Naples, FL, USA) augmentation from the period of January 2018 to January 2020 in Khoo Teck Puat Hospital, Singapore were included in our study retrospectively. The inclusion criteria of this study were adult patients who suffered an unstable (modified Neer type 2 or type 5) distal clavicle fracture (Figs. 1 and 2). Patients excluded from the study were polytraumatic patients, those who had pathological fractures, patients with a concomitant injury to the ipsilateral upper limb, and those undergoing revision fixation.
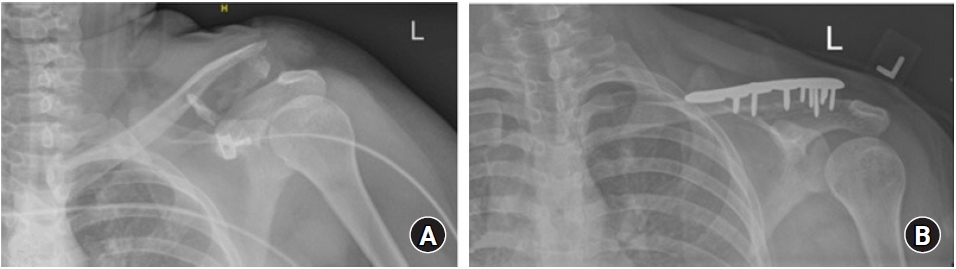
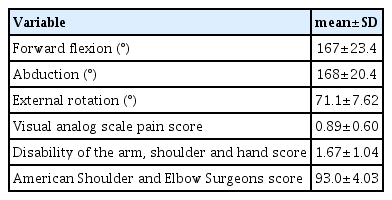
(A) Plain radiographs of a patient with modified Neer type 2 distal clavicle fracture. (B) Final postoperative radiographs demonstrating healed fracture.
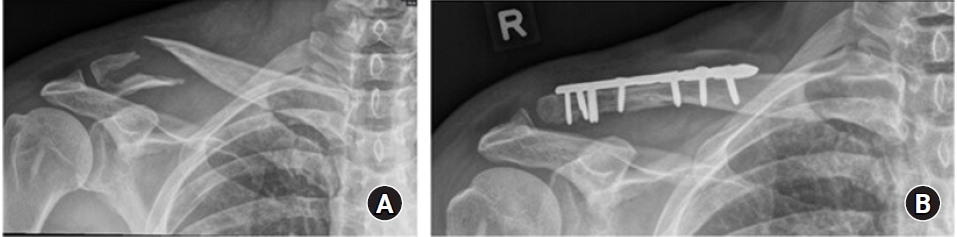
(A) Plain radiographs of a patient with modified Neer type 5 distal clavicle fracture. (B) Final postoperative radiographs demonstrating healed fracture.
Under general anesthesia, the procedures were performed with the patients in a beach-chair position. A longitudinal or saber incision along the distal clavicle was created to allow direct access to the fracture site and coracoid process. The deltotrapezial fascia was split, and the fracture was provisionally reduced under direct visualization and confirmed under fluoroscopy (Fig. 3). A Synthes 3.5 mm LCP Superior Clavicle plate with lateral extension was then applied with as much distal bony purchase as possible using lateral 2.7 mm locking screws (up to six screws). Blunt dissection to the base of the coracoid was performed, and a right-angle curved hemostat was used to guide the Fibertape (Arthrex, USA) around the base of the coracoid process and over the clavicle before being secured using a standard surgeon’s knot and square knots over the plate (Figs. 4 and 5). The wound was closed in layers with reconstruction of the deltoid fascia.
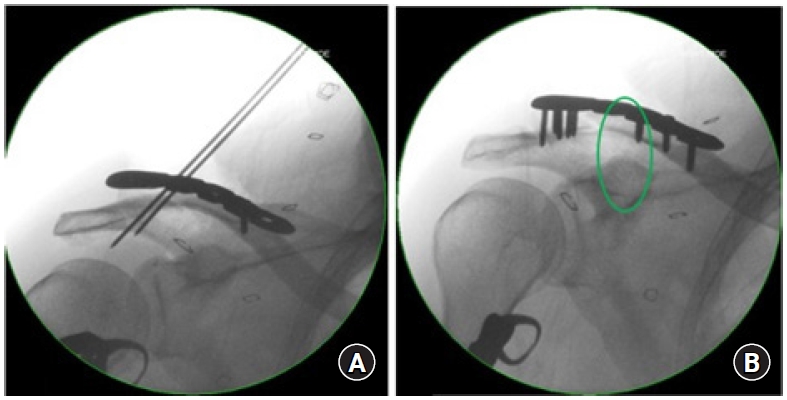
(A) Intraoperative imaging demonstrating reduction of the fracture and initial positioning of the clavicle plate with Kirschner wires. (B) The location of the Fibertape cerclage (green circle).
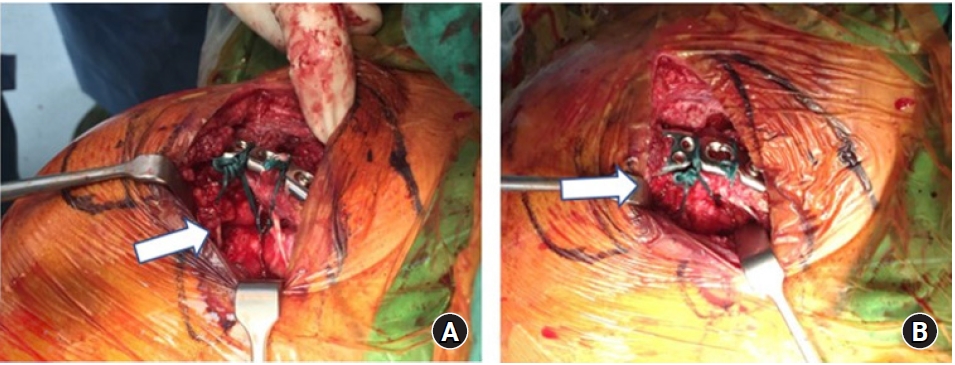
(A) Arrow depicting where the Fibertape cerclage is employed in an under coracoid and around the clavicle manner. (B) Arrow depicting where the Fibertape knot is secured on the clavicle plate.
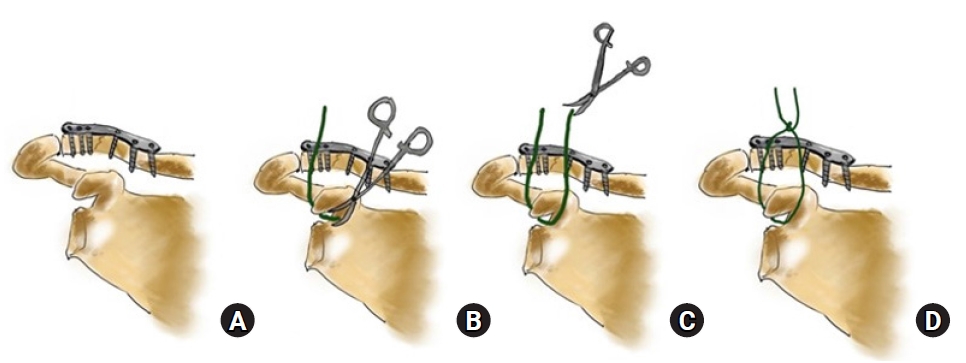
(A) Illustration showing distal clavicle fracture with plate in situ. (B, C) Blunt dissection of base of coracoid performed and the use of a curved haemostat to guide the Fibertape around the coracoid process and over the clavicle. (D) The Fibertape is then secured over the plate with standard surgeon's knot and square knots.
The patients were allowed early passive mobilization of the shoulder on postoperative day 1 with the assistance of a physiotherapist. Graduated progression in range of motion and weight bearing status was advised during subsequent visits, and radiographs were obtained in outpatient clinics.
Clinical and radiographical evaluations of the patients were performed at 6 weeks, 3 months, 6 months, and 1 year after surgery. Functional scoring was performed using the Disabilities of the Arm, Shoulder, and Hand (DASH) and American Shoulder and Elbow Surgeons (ASES) questionnaires. The patient’s objective range of motion was measured along with injury-residual pain using the visual analog scale (VAS) score, with 0 representing no pain and 10 representing the worst possible pain. Postoperative radiographs (anterior-posterior and axial views of the affected clavicle) were obtained at each follow-up visit. Radiographical union was defined as the presence of bridging callus across the fracture site or healing of the fracture line (Fig. 2). Incidences of postoperative complications such as surgical site infection, non-union, and implant failure were recorded.
RESULTS
The study group involved nine patients, of whom eight were males and one was female, with a mean age of 36 years (range, 21–66 years) at the time of surgery. The dominant arm was involved in six of the nine patients. In addition, six of the nine patients were smokers, and all had suffered the injury in a road traffic accident. Of the nine cases, one involved bone grafting for a non-united conservatively treated distal clavicle. The mean time to surgical fixation for acute fracture was 14.75 days (range, 7–25 days). One patient was subsequently lost to follow-up, while the remaining eight patients were followed up for a mean of 10 months (range, 8–13 months).
At their last follow-up assessments, the mean VAS score was 0.88±0.35 (range, 0–1) with a mean DASH score of 1.46±0.87 and ASES score of 94.1±3.57. The mean range of motion achieved was forward flexion at 173±10.6, abduction at 173±10.6, and external rotation at 74.4±10.5 (Table 1). All patients achieved internal rotation at a vertebral height of at least L2.
All patients achieved radiographical union on subsequent follow-ups at a mean of 10±0.82 weeks (range, 9–12 weeks) as determined by a consulting orthopedic surgeon. There were no significant postoperative complications noted, although one patient required a second procedure for exchange of a distal locking screw that was backing out at 1 month postoperative. None of the patients complained of plate and/or knot prominence that required implant removal.
DISCUSSION
The study results suggest that our method of augmented fixation for unstable distal clavicle fractures is reliable with good clinical outcomes, achieved radiographical union, and exhibited no significant postoperative complications. Unstable distal clavicle fractures experience high non-union rates, prompting most surgeons to recommend surgical fixation for more predictable outcomes [5,7-11]. Clavicle hook plates remain a popular option [12,13] as there are concerns of insufficient distal bone purchase with distal clavicle locking plates. However, hook plates have the disadvantage of requiring a subsequent surgery for removal of the implant in order to avoid complications such as subacromial osteolysis, subacromial impingement, and implant fracture [14,15]. Several authors have suggested a combined procedure (clavicle locking plate fixation augmented with CC stabilization) [7,16-20] for added stability [19].
A combined procedure involving a locking plate and CC augmentation has been proposed by various authors to provide greater stability [7,16,17,19]. Xu et al.’s retrospective cohort study [17] comparing distal clavicular locking plates alone with combined use of plates and CC suture anchors exhibited better functional outcomes and a shorter union time with no increase in complications in the combined group. Fan et al.’s study [16] of 28 patients with unstable distal clavicle fracture revealed that anatomical locking plates combined with additional suture anchor fixation resulted in better radiographical and functional outcomes. These results are also supported by biomechanical studies, such as Madsen et al.’s cadaveric study [19] where CC augmentation added additional stability to the fixation construction when loaded to failure. Similar results were reported in another biomechanical study by Alaee et al. [7], which revealed clear improvements in overall construct stability between various methods of CC augmentation coupled with plate fixation.
Various complications of commonly used supplemental stabilization techniques have been described in the literature. Methods such as suture anchors or tight rope fixation require drilling through the coracoid process, risking potential fracture [20,21]. Technical challenges also can complicate a procedure. For example, drilling a hole in the distal clavicle for Endobutton fixation can be complex in more comminuted fracture patterns. A poorly positioned drill hole in the coracoid process can lead to an increased risk of implant failure or cut out [22].
Our proposed method of using a Fibertape cerclage under the coracoid and around the clavicle does not require drilling and avoids the complications described above. It is also a less expensive alternative to the more costly suture anchors. In addition, as a non-metal implant, it does not introduce hardware that might require a subsequent procedure for removal. We believe that this technique will produce consistently good clinical and radiographical outcomes with low rates of complications. These findings are supported by the good outcomes of Martetschläger et al. [20] with a low rate of complications using a distal radius locking plate and a 1.5-mm braided polydioxanone suture (PDS) cord as a cerclage. We believe that the use of a Fibertape cerclage is a more robust option due to its greater width (2 mm) and higher biomechanical failure load compared to the use of a PDS suture [23,24].
There are disadvantages to the use of a CC cerclage alone that have been highlighted in the literature. Some authors [25] argue that CC cerclage stabilization produces greater anterior-posterior translation compared to other techniques. This is supported by Alaee’s biomechanical study [7] showing an increase in anterior-posterior translation with the use of a suture cerclage around the coracoid compared to an intact native CC ligament. However, there was no difference in load to failure or stiffness between the constructs. In the absence of clinical studies comparing the various techniques, this apparent difference might not affect the final functional outcome. Another drawback to this technique is that it relies on the integrity of the coracoid and cannot be performed if the patient has a concomitant fracture of the coracoid.
There are a few limitations to our study. It is a case series with a small group of patients with relatively short follow-up periods. This prohibited us from observing longer term complications of the cerclage technique such as osteolysis and erosion of the distal clavicle [26] or development of AC joint arthritis. However, the development of osteolysis is likely to be averted with our technique as the Fibertape is anchored around the locking plate and not directly on the clavicle. In addition, the follow-up period is sufficient to evaluate bony healing as all cases exhibited union at a mean of 10 weeks. Longer term studies with a larger sample size will be useful to better reflect the long-term outcomes and efficacy of this technique. Studies elucidating circumstances when augmented osteosynthesis is best indicated will also be helpful in guiding treatment.
In conclusion, our modified technique of an augmented distal clavicle fixation is reliable, produces good clinical results, has no significant complications, and did not require subsequent surgery for removal of implants within our period of follow-up.
Notes
Financial support
None.
Conflict of interest
None.