Radiofrequency in arthroscopic shoulder surgery: a systematic review
Article information
Abstract
Background
Radiofrequency has seen an increase in use in orthopedics including cartilage lesion debridement in the hip and knee as well as many applications in arthroscopic shoulder surgery. The purpose of this systematic review is to evaluate the safety and usage of radiofrequency in the shoulder.
Methods
This systematic review was registered with PROSPERO (international registry) and followed the preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) guidelines. Embase and PubMed were searched using: “shoulder,” “rotator cuff,” “biceps,” “acromion” AND “monopolar,” “bipolar,” “ablation,” “coblation,” and “radiofrequency ablation.” The title and abstract review were performed independently. Any discrepancies were addressed through open discussion.
Results
A total of 63 studies were included. Radiofrequency is currently utilized in impingement syndrome, fracture fixation, instability, nerve injury, adhesive capsulitis, postoperative stiffness, and rotator cuff disease. Adverse events, namely superficial burns, are limited to case reports and case series, with higher-level evidence demonstrating safe use when used below the temperature threshold. Bipolar radiofrequency may decrease operative time and decrease the cost per case.
Conclusions
Shoulder radiofrequency has a wide scope of application in various shoulder pathologies. Shoulder radiofrequency is safe; however, requires practitioners to be cognizant of the potential for thermal burn injuries. Bipolar radiofrequency may represent a more efficacious and economic treatment modality. Safety precautions have been executed by institutions to cut down patient complications from shoulder radiofrequency. Future research is required to determine what measures can be taken to further minimize the risk of thermal burns.
Level of evidence
IV.
INTRODUCTION
Radiofrequency (RF) refers to application of thermal energy to reorganize tissue on a molecular level and restore normal structure and function [1]. Traditional RF or electrocauterization refers to the use of thermal energy to treat surgical pathology by passing electrical current directly through tissue [1]. RF can be delivered through a monopolar or bipolar device [1-3]. Bipolar RF represents a safer alternative at lower temperatures, voltages, contact pressures, and contact times [1]. These devices create high-energy free radicals that can break molecular bonds and excise soft tissue at relatively low temperatures (40°C–70°C) [2]. RF systems are widely used in arthroscopic orthopedic procedures for ablation, resection, and coagulation of soft tissues [3]. RF energy is not without its risks and does exhibit time-dependent effects that need to be considered by surgeons [4]. Next-generation RF devices utilize plasma energy fields to deliver thermal energy to minimize damage to the surrounding soft tissues [1,5].
The safety profile of RF has been studied in the knee in the context of low-grade cartilage lesions [2]. The safety of RF has also been well-studied in the hip for ablating soft tissues [6]. In the glenohumeral joint, RF was first studied in the context of instability but resulted in overtreatment [7], permanent tissue damage [7], and high failure rates necessitating capsular plication [8,9]. However, there are limited reports on the temperature profile and complications in shoulder joint RF.
In recent years, there have been many studies published regarding the use of RF energy in the surgical treatment of many shoulder pathologies. In the existing publications regarding RF use in the shoulder, the purpose of the equipment is to split and partially remove soft tissues [10-20]. However, the safety and complications of RF use to debride soft tissue have not been established. The purpose of this investigation is to conduct a systematic review of the currently available literature to evaluate the safety and complication profile of RF devices for use in the shoulder.
METHODS
General
This systematic review was registered in an international prospective register of systematic reviews (PROSPERO No. CRD42021288444.) The Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) guidelines were followed.
Literature Search
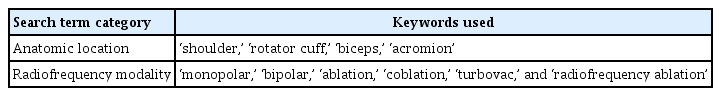
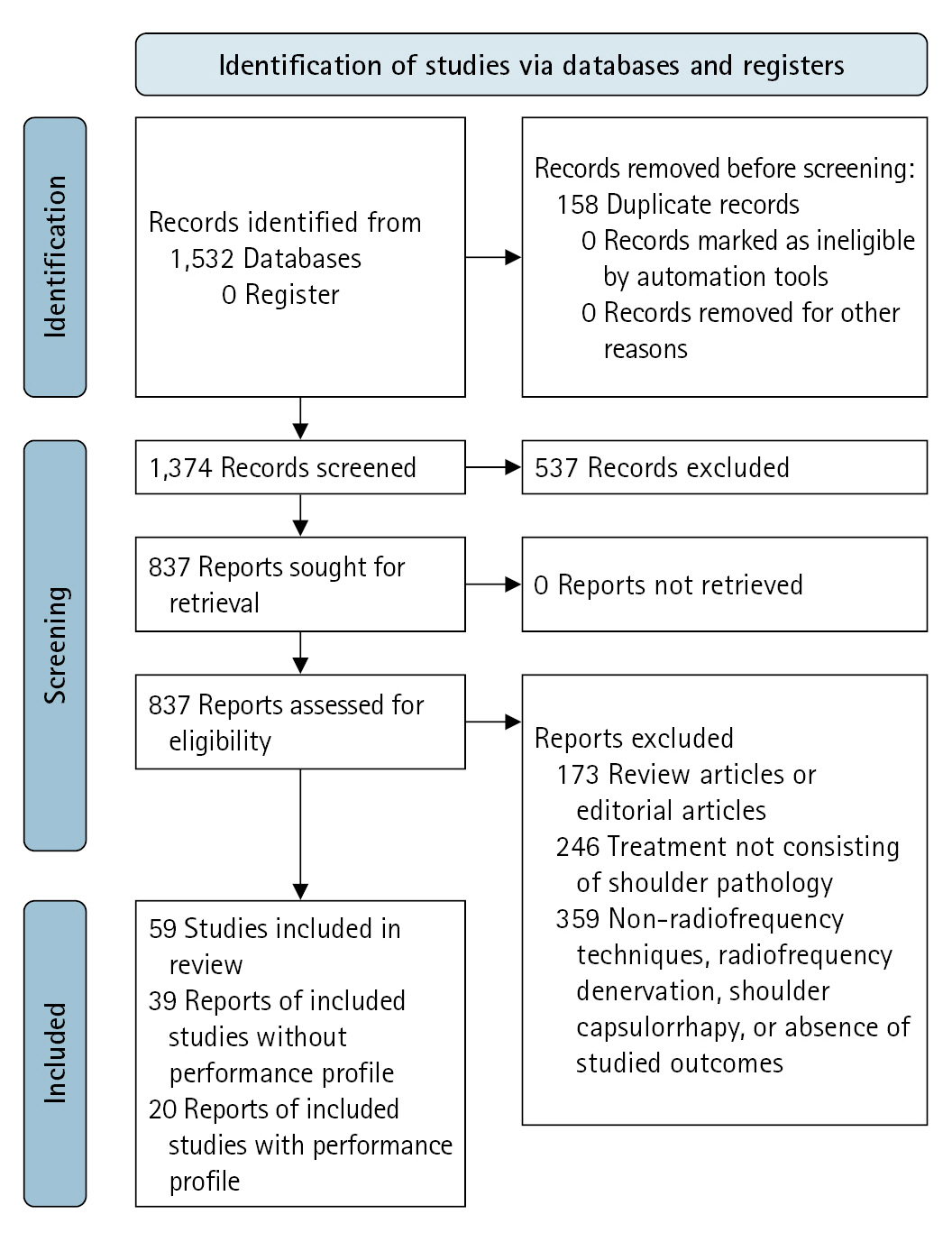
The literature search was performed using Embase and PubMed with the keywords displayed in Table 1. The initial literature search revealed 1,531 studies. After removal of duplicate articles, title and abstract screening was performed on 1,374 studies. Of these, 537 studies did not pertain to the use of RF in arthroscopic shoulder surgery. Finally, the full-text of 837 studies was screened (Fig. 1).
Study Selection
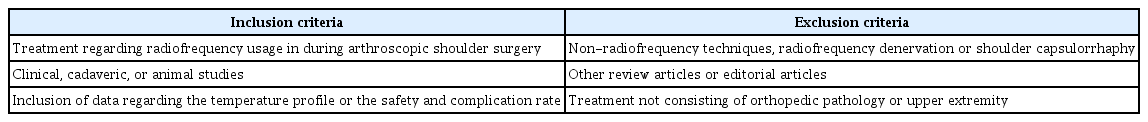
Studies were selected according to the inclusion and exclusion criteria presented in Table 2. Of note, studies related to shoulder capsulorrhaphy usage were excluded, given the high complication rates of axillary nerve dysfunction, articular cartilage damage, and capsular necrosis [21]. Application of our inclusion and exclusion criteria resulted in a total of 63 studies.
Qualitative Synthesis
Due to a limited number of high-level clinical studies on the topic and heterogeneous reporting of data, the included studies were qualitatively synthesized. The included studies were grouped into those that contained data regarding the performance profile of RF and those that did not. The performance profile was defined as any mention of the temperature profile, safety profile and complication rate, or clinical outcomes. These studies were grouped accordingly and descriptively summarized in the tables.
RESULTS
General
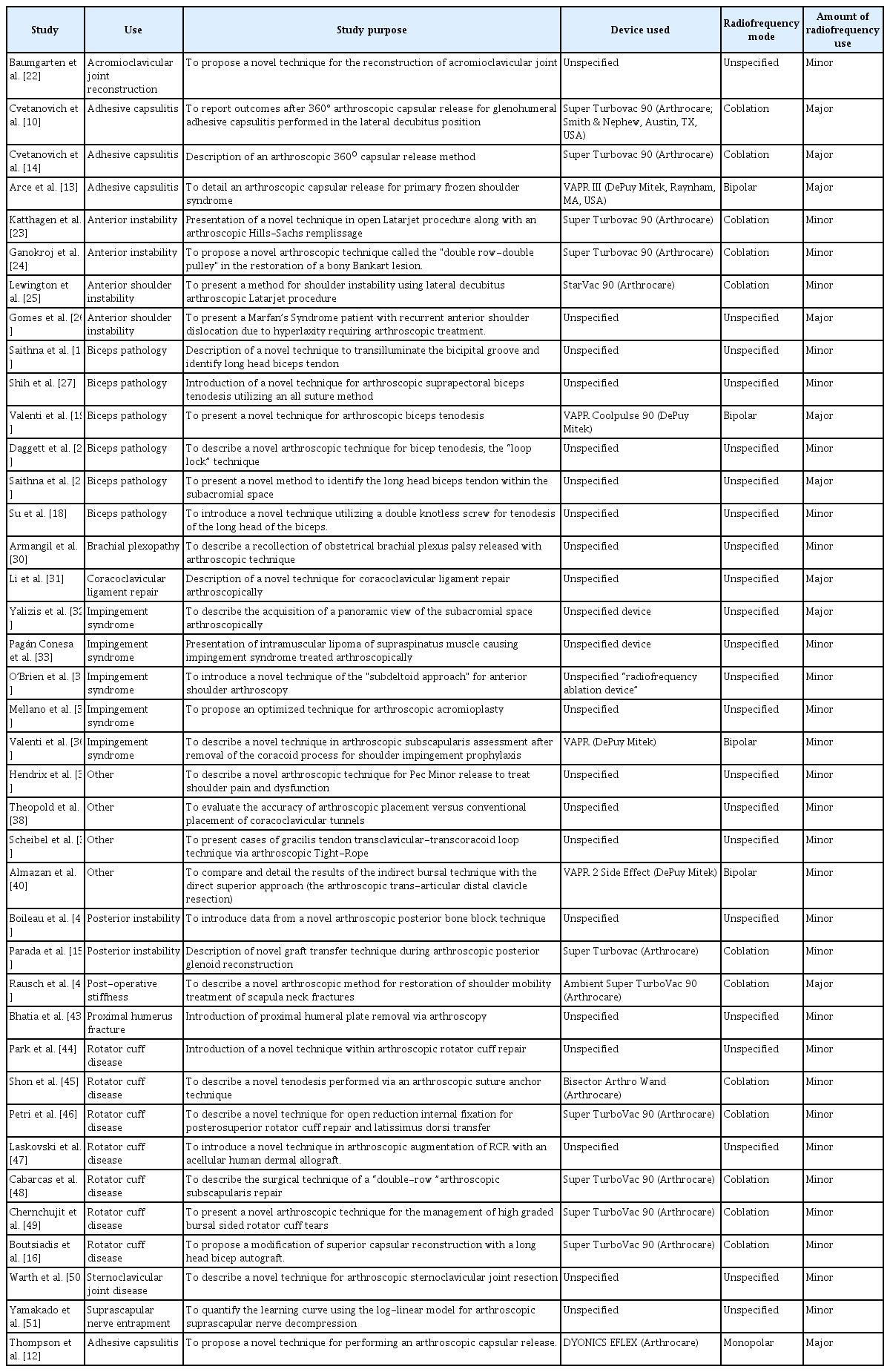
Of our 59 included articles, 39 did not include RF performance in terms of temperature profile or complications. The remaining 20 studies did include at least one of these measures. The studies in this review that discuss RF for shoulder arthroscopic orthopedic procedures without data on performance profile do provide insight regarding the breadth of shoulder RF use and are summarized in Table 3 [10,12-19,22-51]. Table 3 revealed bipolar RF as the most commonly used modality. Of the 39 studies depicted in Table 3, only 17 (43.6%) specified the RF modality, all of which were bipolar. The remaining 22 studies (56.4%) were unspecified.
Performance Profile
Studies that disclosed the performance profile of RF usage in the shoulder were further analyzed. These studies were grouped by temperature profile (Table 4) [3,20,52-62] and complications (Table 5) [21,63-68].
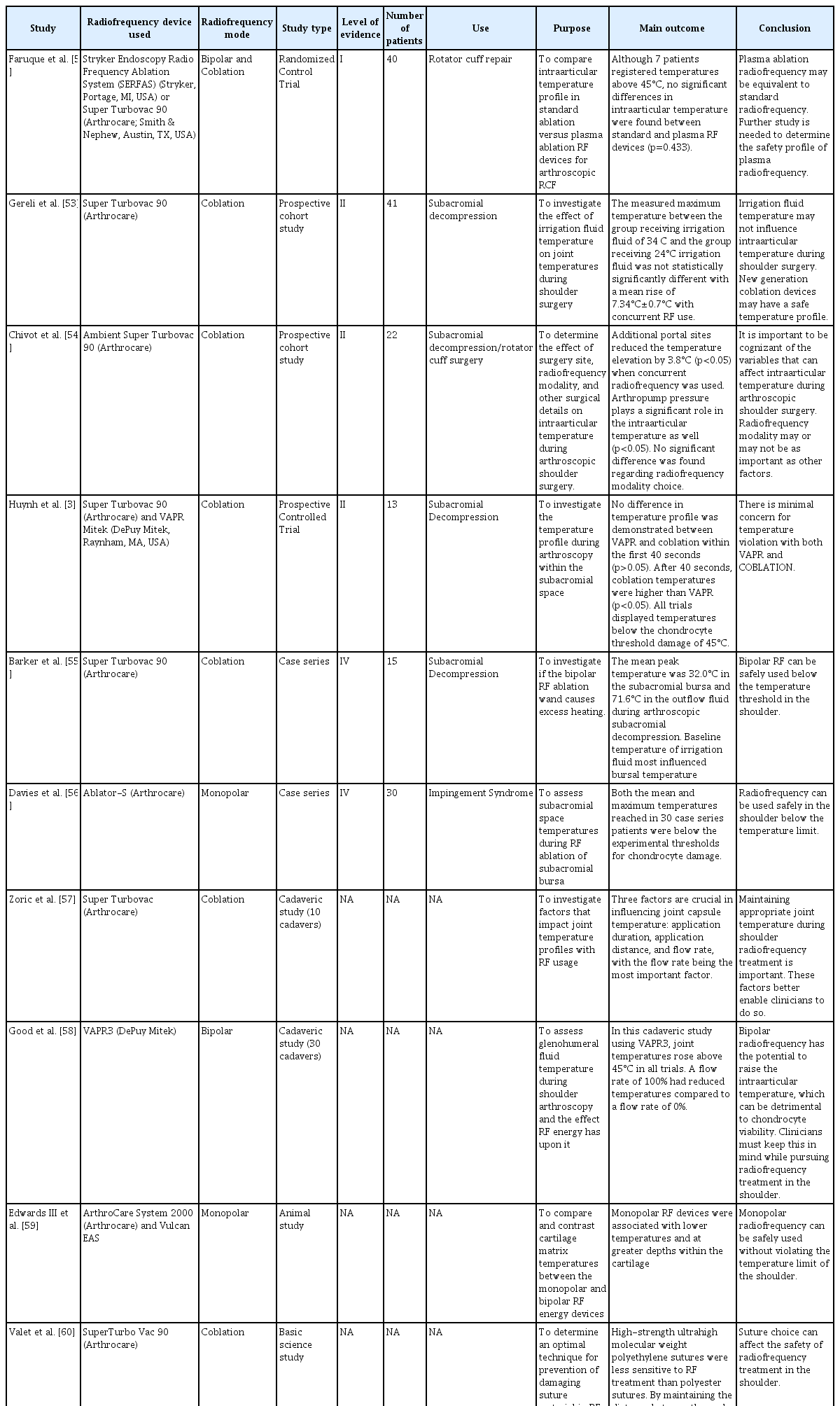
Included studies for which the temperature profile was the primary outcome with regards to radiofrequency usage in the shoulder
Temperature Profile
Our literature review identified two randomized controlled trials, two prospective cohort studies, two case series, three cadaveric studies, two animal studies, and two basic science studies exploring the temperature profile of RF ablation devices in the shoulder (Table 4).
While comparing RF instruments, Huynh et al. [3] found few differences in temperature characteristics. The peak temperature during RF usage in subacromial decompression was 32.0°C (range, 29.3 °C–43.1°C) [55]. The mean peak temperature of outflow fluid was 71.6°C, assumed to mimic wand tip temperature, which should be between 40 and 70°C [55]. During the study, Barker et al. [55] found the most crucial factor in subacromial temperature to be fluid irrigation temperature. For this reason, they recommended against the use of warmed irrigation fluid in RF. Davies et al. [56] also suggested that irrigation fluid be cooled before RF usage. In their case series of 30 patients, subacromial bursa temperature during RF with a monopolar device was assessed. Mean (27.8°C) and maximum (41.8°C) temperatures were observed well below the chondrocyte damage threshold temperature. The authors explained the isolated reading of 41.8°C to be due to blockage of the RF suction probe [56].
Good et al. [58] performed a cadaveric study regarding intraarticular temperatures during shoulder RF use. Intraarticular temperatures increased above 45°C in each trial. The highest peak temperatures were observed when the fluid flow rate was 0%, while the lowest peak temperatures were observed when the fluid flow rate was 100% [58]. No statistical differences in mean temperature were observed whether the device was immersed in fluid or in direct contact with tissue [58]. Zoric et al. [57] demonstrated three factors that were critical for maintaining safe intra-articular temperature: rate of flow, distance of device application, and duration of usage. This study also suggested that maximization of irrigation flow, shorter duration of device use, and adequate suction techniques further prevent temperature-related patient complications and injuries.
Safety and Complications
Overall, reports of postoperative complications following RF methods were lacking (Table 5). Our literature search revealed one prospective controlled trial, one case series, and five case reports that provided significant complication rates or commented on the safety profile. The small number of reported complications from RF usage within the literature was related to increased irrigation fluid temperature and was limited to case reports [55] and case series [65]. Four cases of second-degree burns were reported by Troxell et al. [65] due to a bipolar RF device being used in an unreported number of patients over 4 years. The authors [65] attributed these four cases to lack of outflow tubing. Since changing their practice, further burn cases have not occurred.
The most common adverse events of RF use are thermal injuries due to high temperature of the fluid and surrounding tissue [3]. Many studies involve novel arthroscopic techniques with RF devices, yet parameters of its use such as safety, complications, and outcome profiles are poorly detailed within the majority of studies [16,44-49,69]. All four studies reporting these adverse events specify second-degree burns as related to direct contact of the irrigation fluid from outflow tubing rather than from contiguous, elevated intraarticular temperatures [65-68]. Dermal burns have been reported during subacromial decompression [66]. Surgeons, however, plugged fluid outflow to increase the joint tamponade effect for better visibility, resulting in overheated irrigation fluid that burned the patient [66]. To decrease the burn risk, it is recommended that suction surveillance and high fluid outflow be maintained by surgeons [68].
DISCUSSION
In this systematic review of the literature, 63 studies demonstrated the safety and efficacy of RF devices within the shoulder. Of these, 25 studies explicitly studied the temperature profile, safety profile, or clinical outcomes. Though the temperature and safety profile were reasonably well described, functional or patient-reported outcomes after RF treatment were sparse [10,11,13-19, 22,23,25-27,29-33,35,39-45,49-51].
Our study demonstrated that the landscape of shoulder RF has changed significantly since it was originally studied in the context of shoulder instability [1,7,9]. Given the unanimous findings of poor outcomes in this setting, RF is largely used for debriding soft tissue (Table 3). Yasura et al. [70] demonstrated that bipolar RF resulted in significantly less chondrocyte death than unipolar RF in the knee. The results of our systematic review seem to be in concordance with this and demonstrate a general trend toward the use of bipolar RF in recent years. Though a few studies in our literature review demonstrate adverse thermal effect profiles, these are limited to case reports [65-67], case series, and cadaveric studies [58]. Shoulder joint temperature increases with the use of RF technologies [3,55,58]. The flow of irrigation fluid [55,57,58], length of application [55,57], device used [3], and proximity of the thermometer to the RF wand [57,58] all impact the temperature profile.
The incidence of RF complications was appropriately reported [21,63-68,71] and generally comprised superficial burns related to fluid irrigation temperature [65-68]. All of the Level III or higher studies reporting temperature profile demonstrate a favorable profile (Table 5). This is in concordance with the literature on RF use in the knee [1,5] and hip [6]. Maintenance of inflow and outflow circulation, avoidance of plugged arthroscopic fluid outflow, avoidance of excess use of coagulation mode [54], and monitoring overheating of the tubing can be performed to reduce burn complications with RF in the shoulder. It is well known that cartilage is more heat-sensitive than other tissues in the human body, and this must be considered when treating cartilage lesions [1].
It is important to consider economic efficiency when determining the RF modality of choice. Efficiency and cost between monopolar RF and bipolar RF in 40 arthroscopic subacromial decompression patients were investigated by Diab et al. [72]. The mean operative time in the bipolar group was 13 minutes (5–25 minutes), while it was 21 minutes (10–35 minutes) for the monopolar RF device group. Bipolar RF decreased the average procedure time by 8 minutes (p<0.0001), while simultaneously decreasing cost by 83 British Pounds (111 European Euros) per case (p<0.003) in comparison to monopolar RF [72]. Based on these results, the authors recommended bipolar RF when clinical judgment deems it appropriate.
This systematic review is not without its limitations. As a systematic review of level I–level IV evidence, the findings are limited to level IV. Due to heterogeneous data reporting, this is a comprehensive summary of all studies delineating the use of RF in the shoulder as defined by the inclusion and exclusion criteria. However, many of the studies included were limited by unspecified use of RF. Further, our study is unable to comment on the clinical outcomes of RF based on the inclusion criteria regarding temperature profile and safety/complications of shoulder RF. The results pertaining to safety and complication are based on a limited subset of select articles. Thus, the findings of this study may be limited by selection bias.
CONCLUSIONS
Shoulder RF has a wide scope of application in various shoulder pathologies. Although shoulder RF is safe, it requires practitioners to be cognizant of the potential for thermal burn injuries. Protocols regarding irrigation fluid temperature and outflow rates should be set by individual institutions to further reduce minor patient complications of shoulder RF. Future research is required to determine measures to minimize further the risk of thermal burn injuries.
Notes
Author contributions
Conceptualization: NV, JNL, NA. Data curation: NV, JNL, NA. Formal Analysis: NV, JNL, NA. Investigation: NV, JNL, NA. Methodology: NV, JNL, NA. Project administration: JNL, NA. Resources: NV, JNL, NA. Software: NV, JNL, NA. Supervision: JNL, NA. Validation: NV, JNL, NA. Visualization: NV, JNL, NA. Writing – original draft: NV, JNL, NA. Writing – review & editing: NV, JNL, NA.
Conflict of interest
None.
Funding
None.
Data availability
None.
Acknowledgments
None.