1. Khatib O, Onyekwelu I, Yu S, Zuckerman JD. Shoulder arthroplasty in New York State, 1991 to 2010: changing patterns of utilization. J Shoulder Elbow Surg 2015;24:e286–91.


2. Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am 2011;93:2249–54.


4. Trofa D, Rajaee SS, Smith EL. Nationwide trends in total shoulder arthroplasty and hemiarthroplasty for osteoarthritis. Am J Orthop (Belle Mead NJ) 2014;43:166–72.

5. Bryant D, Litchfield R, Sandow M, Gartsman GM, Guyatt G, Kirkley A. A comparison of pain, strength, range of motion, and functional outcomes after hemiarthroplasty and total shoulder arthroplasty in patients with osteoarthritis of the shoulder: a systematic review and meta-analysis. J Bone Joint Surg Am 2005;87:1947–56.

6. Gartsman GM, Roddey TS, Hammerman SM. Shoulder arthroplasty with or without resurfacing of the glenoid in patients who have osteoarthritis. J Bone Joint Surg Am 2000;82:26–34.


7. Hasan SS, Fleckenstein CM. Glenohumeral chondrolysis: part I: clinical presentation and predictors of disease progression. Arthroscopy 2013;29:1135–41.


8. Matsen FA, Papadonikolakis A. Published evidence demonstrating the causation of glenohumeral chondrolysis by postoperative infusion of local anesthetic via a pain pump. J Bone Joint Surg Am 2013;95:1126–34.


9. Johnson MH, Paxton ES, Green A. Shoulder arthroplasty options in young (<50 years old) patients: review of current concepts. J Shoulder Elbow Surg 2015;24:317–25.


11. McCarty LP, Cole BJ. Nonarthroplasty treatment of glenohumeral cartilage lesions. Arthroscopy 2005;21:1131–42.


12. Saltzman BM, Leroux TS, Verma NN, Romeo AA. Glenohumeral osteoarthritis in the young patient. J Am Acad Orthop Surg 2018;26:e361–70.


13. Cameron BD, Galatz LM, Ramsey ML, Williams GR, Iannotti JP. Non-prosthetic management of grade IV osteochondral lesions of the glenohumeral joint. J Shoulder Elbow Surg 2002;11:25–32.


14. Millett PJ, Gaskill TR. Arthroscopic management of glenohumeral arthrosis: humeral osteoplasty, capsular release, and arthroscopic axillary nerve release as a joint-preserving approach. Arthroscopy 2011;27:1296–303.


15. Millett PJ, Horan MP, Pennock AT, Rios D. Comprehensive arthroscopic management (CAM) procedure: clinical results of a joint-preserving arthroscopic treatment for young, active patients with advanced shoulder osteoarthritis. Arthroscopy 2013;29:440–8.


16. Van Thiel GS, Sheehan S, Frank RM, et al. Retrospective analysis of arthroscopic management of glenohumeral degenerative disease. Arthroscopy 2010;26:1451–5.


17. Weinstein DM, Bucchieri JS, Pollock RG, Flatow EL, Bigliani LU. Arthroscopic debridement of the shoulder for osteoarthritis. Arthroscopy 2000;16:471–6.


18. Sayegh ET, Mascarenhas R, Chalmers PN, Cole BJ, Romeo AA, Verma NN. Surgical treatment options for glenohumeral arthritis in young patients: a systematic review and meta-analysis. Arthroscopy 2015;31:1156–66.e8.


19. Hasan SS, Fleckenstein CM. Glenohumeral chondrolysis: part II: results of treatment. Arthroscopy 2013;29:1142–8.


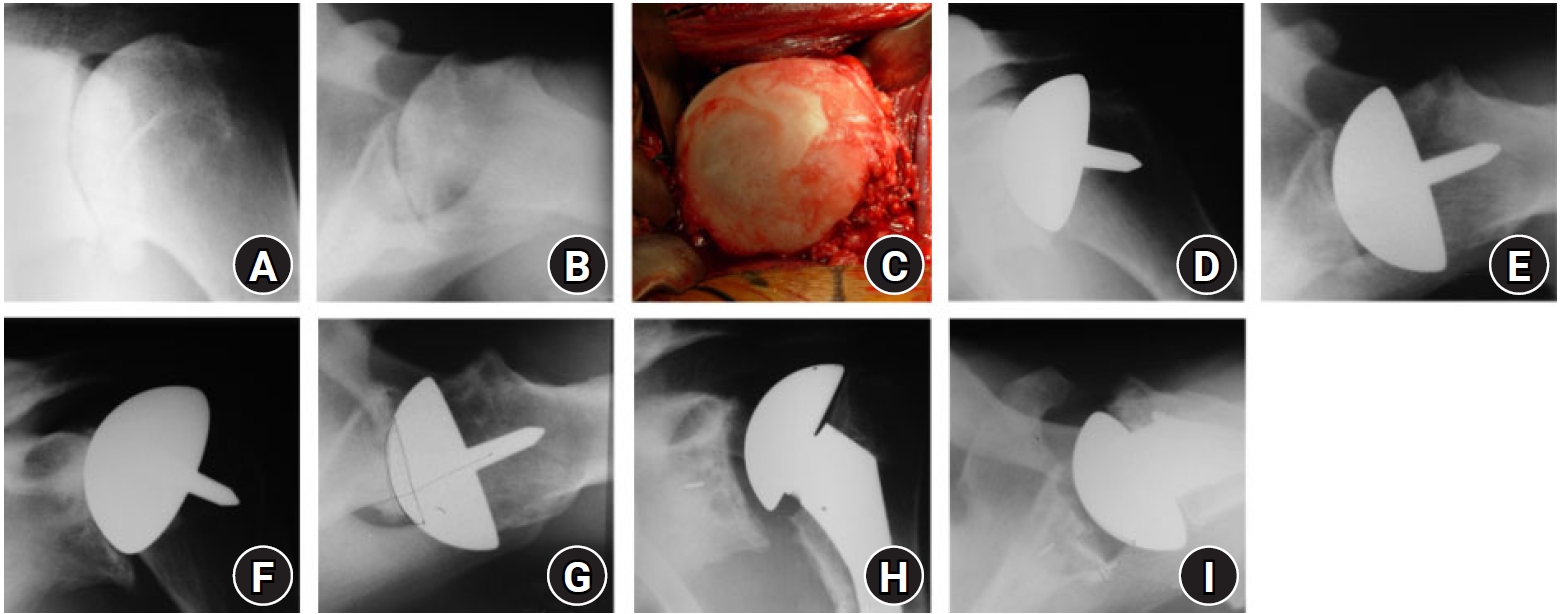
20. Schoch B, Werthel JD, Cofield R, Sanchez-Sotelo J, Sperling JW. Shoulder arthroplasty for chondrolysis. J Shoulder Elbow Surg 2016;25:1470–6.


21. Bailie DS, Llinas PJ, Ellenbecker TS. Cementless humeral resurfacing arthroplasty in active patients less than fifty-five years of age. J Bone Joint Surg Am 2008;90:110–7.


22. Bartelt R, Sperling JW, Schleck CD, Cofield RH. Shoulder arthroplasty in patients aged fifty-five years or younger with osteoarthritis. J Shoulder Elbow Surg 2011;20:123–30.


23. Eichinger JK, Miller LR, Hartshorn T, Li X, Warner JJ, Higgins LD. Evaluation of satisfaction and durability after hemiarthroplasty and total shoulder arthroplasty in a cohort of patients aged 50 years or younger: an analysis of discordance of patient satisfaction and implant survival. J Shoulder Elbow Surg 2016;25:772–80.


24. Schoch B, Schleck C, Cofield RH, Sperling JW. Shoulder arthroplasty in patients younger than 50 years: minimum 20-year follow-up. J Shoulder Elbow Surg 2015;24:705–10.


25. Sperling JW, Cofield RH, Rowland CM. Neer hemiarthroplasty and Neer total shoulder arthroplasty in patients fifty years old or less: long-term results. J Bone Joint Surg Am 1998;80:464–73.


26. Sperling JW, Cofield RH, Rowland CM. Minimum fifteen-year follow-up of Neer hemiarthroplasty and total shoulder arthroplasty in patients aged fifty years or younger. J Shoulder Elbow Surg 2004;13:604–13.


27. Levy JC, Virani NA, Frankle MA, Cuff D, Pupello DR, Hamelin JA. Young patients with shoulder chondrolysis following arthroscopic shoulder surgery treated with total shoulder arthroplasty. J Shoulder Elbow Surg 2008;17:380–8.


28. Rill BK, Fleckenstein CM, Levy MS, Nagesh V, Hasan SS. Predictors of outcome after nonoperative and operative treatment of adhesive capsulitis. Am J Sports Med 2011;39:567–74.


29. Saltzman MD, Mercer DM, Warme WJ, Bertelsen AL, Matsen FA. Comparison of patients undergoing primary shoulder arthroplasty before and after the age of fifty. J Bone Joint Surg Am 2010;92:42–7.


30. Wagner ER, Houdek MT, Schleck CD, et al. The role age plays in the outcomes and complications of shoulder arthroplasty. J Shoulder Elbow Surg 2017;26:1573–80.


32. Jensen KL. Humeral resurfacing arthroplasty: rationale, indications, technique, and results. Am J Orthop (Belle Mead NJ) 2007;36(12 Suppl 1):4–8.
33. Levy O, Tsvieli O, Merchant J, et al. Surface replacement arthroplasty for glenohumeral arthropathy in patients aged younger than fifty years: results after a minimum ten-year follow-up. J Shoulder Elbow Surg 2015;24:1049–60.


35. Merolla G, Bianchi P, Lollino N, Rossi R, Paladini P, Porcellini G. Clinical and radiographic mid-term outcomes after shoulder resurfacing in patients aged 50 years old or younger. Musculoskelet Surg 2013;97 Suppl 1:23–9.


36. Raiss P, Pape G, Becker S, Rickert M, Loew M. Cementless humeral surface replacement arthroplasty in patients less than 55 years of age. Orthopade 2010;39:201–8.


37. Rispoli DM, Sperling JW, Athwal GS, Schleck CD, Cofield RH. Humeral head replacement for the treatment of osteoarthritis. J Bone Joint Surg Am 2006;88:2637–44.


38. Brolin TJ, Thakar OV, Abboud JA. Outcomes after shoulder replacement surgery in the young patient: how do they do and how long can we expect them to last. Clin Sports Med 2018;37:593–607.


39. Elhassan B, Ozbaydar M, Diller D, Higgins LD, Warner JJ. Soft-tissue resurfacing of the glenoid in the treatment of glenohumeral arthritis in active patients less than fifty years old. J Bone Joint Surg Am 2009;91:419–24.


40. Hammond LC, Lin EC, Harwood DP, et al. Clinical outcomes of hemiarthroplasty and biological resurfacing in patients aged younger than 50 years. J Shoulder Elbow Surg 2013;22:1345–51.


41. Lee KT, Bell S, Salmon J. Cementless surface replacement arthroplasty of the shoulder with biologic resurfacing of the glenoid. J Shoulder Elbow Surg 2009;18:915–9.


42. Lollino N, Pellegrini A, Paladini P, Campi F, Porcellini G. Gleno-Humeral arthritis in young patients: clinical and radiographic analysis of humerus resurfacing prosthesis and meniscus interposition. Musculoskelet Surg 2011;95 Suppl 1:S59–63.


43. Puskas GJ, Meyer DC, Lebschi JA, Gerber C. Unacceptable failure of hemiarthroplasty combined with biological glenoid resurfacing in the treatment of glenohumeral arthritis in the young. J Shoulder Elbow Surg 2015;24:1900–7.


44. Muh SJ, Streit JJ, Shishani Y, Dubrow S, Nowinski RJ, Gobezie R. Biologic resurfacing of the glenoid with humeral head resurfacing for glenohumeral arthritis in the young patient. J Shoulder Elbow Surg 2014;23:e185–90.


46. Clinton J, Franta AK, Lenters TR, Mounce D, Matsen FA. Nonprosthetic glenoid arthroplasty with humeral hemiarthroplasty and total shoulder arthroplasty yield similar self-assessed outcomes in the management of comparable patients with glenohumeral arthritis. J Shoulder Elbow Surg 2007;16:534–8.


47. Gilmer BB, Comstock BA, Jette JL, Warme WJ, Jackins SE, Matsen FA. The prognosis for improvement in comfort and function after the ream-and-run arthroplasty for glenohumeral arthritis: an analysis of 176 consecutive cases. J Bone Joint Surg Am 2012;94:e102.


48. Gowd AK, Garcia GH, Liu JN, Malaret MR, Cabarcas BC, Romeo AA. Comparative analysis of work-related outcomes in hemiarthroplasty with concentric glenoid reaming and total shoulder arthroplasty. J Shoulder Elbow Surg 2019;28:244–51.


49. Hasan SS. Revisiting the socket: commentary on an article by Jeremy S. Somerson, MD, et al.: “Clinical and radiographic outcomes of the ream-and-run procedure for primary glenohumeral arthritis”. J Bone Joint Surg Am 2017;99:e85.


50. Matsen FA. The ream and run: not for every patient, every surgeon or every problem. Int Orthop 2015;39:255–61.


51. Somerson JS, Neradilek MB, Service BC, Hsu JE, Russ SM, Matsen FA. Clinical and radiographic outcomes of the ream-and-run procedure for primary glenohumeral arthritis. J Bone Joint Surg Am 2017;99:1291–304.


52. Virk MS, Thorsness RJ, Griffin JW, et al. Short-term clinical outcomes of hemiarthroplasty with concentric glenoid reaming: the ream and run procedure. Orthopedics 2018;41:e854–60.


53. Matsen FA, Carofino BC, Green A, et al. Shoulder hemiarthroplasty with nonprosthetic glenoid arthroplasty: the ream-and-run procedure. JBJS Rev 2021;9:e20.00243.

54. Dillon MT, Inacio MC, Burke MF, Navarro RA, Yian EH. Shoulder arthroplasty in patients 59 years of age and younger. J Shoulder Elbow Surg 2013;22:1338–44.


55. Kany J, Benkalfate T, Favard L, et al. Osteoarthritis of the shoulder in under-50 year-olds: a multicenter retrospective study of 273 shoulders by the French Society for Shoulder and Elbow (SOFEC). Orthop Traumatol Surg Res 2021;107:102756.


56. Schiffman CJ, Hannay WM, Whitson AJ, Neradilek MB, Matsen FA, Hsu JE. Impact of previous non-arthroplasty surgery on clinical outcomes after primary anatomic shoulder arthroplasty. J Shoulder Elbow Surg 2020;29:2056–64.