Mid- to long-term success rate and functional outcomes of acromioclavicular injections in patients with acromioclavicular osteoarthritis
Article information
Abstract
Background
Acromioclavicular (AC) osteoarthritis (OA) is a frequent pathology of the shoulder in elderly patients. Drug injection plays an important role in treatment of AC OA. Literature has demonstrated excellent short-term results regarding shoulder function and pain. However, mid- to long-term results are lacking. The aim of this study was to assess the efficacy of a single intra-articular AC injection in patients with AC OA and to identify predictive factors for success.
Methods
A retrospective study was performed to analyze success rate, shoulder function, and pain perception after a single intra-articular injection in patients with AC OA. Success was defined as the absence of reinterventions such as additional injection or surgery. Outcome measures were 1-year success rate and clinical outcome scores of Numeric Rating Scale (NRS) for pain, Oxford Shoulder Score, and Subjective Shoulder Value.
Results
Ninety-eight patients participated in this study. At a median final follow-up of 0.8 years (interquartile range, 0–6), 57 of these patients (58%) had undergone a reintervention. The 1-year success rate was 47% (95% confidence interval, 37%–57%), with NRS at rest as the sole factor significantly associated with success. Thirty patients not requiring reintervention reported significant improvement from baseline for all reported outcome measures at final follow-up.
Conclusions
AC injections offer a 1-year success rate of 47%. The AC injection produces good mid- to long-term clinical outcomes regarding shoulder function, quality of life, and pain perception in one-third of patients. Further research is essential to analyze mid- to long-term outcomes of AC injections.
Level of evidence
Level IV.
INTRODUCTION
Osteoarthritis (OA) of the acromioclavicular (AC) joint occurs in 48% to 82% of the population older than 50 years, often without symptoms [1]. AC OA mainly presents in combination with concomitant pathologies such as subacromial pain syndrome, biceps tendinopathy, or rotator cuff pathology [2]. According to Farrell et al. [2], only 7% of all AC OA cases are isolated, emphasizing the selectivity of this condition and the importance of proper diagnosis and correct treatment algorithm. Clinical presentation of AC OA is characterized by specific pain in the anterosuperior region of the shoulder, increasing with overhead or cross-body motions. Pain increases when pressure is exercised on the AC joint; for instance, when patients are wearing a backpack or bra. Diagnosis is based on patient history, physical examination, and additional imaging such as X-ray or ultrasound [3].
Conservative treatment is preferred, initially consisting of a combination of oral analgesics, physical therapy, activity modifications, and intra-articular injections. When conservative treatment fails, surgical treatment is indicated. Arthroscopic or mini-open distal clavicle resection known as the Mumford procedure is the gold standard, with an overall success rate greater than 90% [4,5].
Regarding conservative treatment, an optimal treatment algorithm is lacking [6]. Intra-articular AC injections produce good short-term outcomes and may have added value for AC OA diagnosis. The literature reports good short-term results of pain relief and shoulder function, with a maximum follow-up of 3 weeks [7,8]. There is no consensus, however, on significant benefits of AC injections in comparison to placebo treatments or regarding difference in pain relief [9,10]. Studies regarding mid- to long-term results (defined as longer than 6 months) in intra-articular AC injections in patients with AC OA are scarce. Hossain et al. [11] reported significant pain relief for at least 12 months after treatment with a single AC injection. van Riet et al. [12] stated that only 28% of patients treated with AC injection experienced significant benefits in shoulder function and pain relief at 1 month after administration.
The primary aim of this study was to determine the 1-year success rate of a single intra-articular AC injection in patients with symptomatic isolated AC OA. Second, this study aimed to identify predictive factors associated with successful injection and to investigate outcomes of shoulder function and pain perception at a minimum of 1-year of follow-up.
METHODS
This single-center retrospective study was approved by the Institutional Review Board of Spaarne Gasthuis Hospital (ACLU Spaarne Gasthuis: 2020.0100). This was a retrospective study to assess healthcare over mid- to long-term follow-up. Informed consent was acquired for each patient.
Population
All patients with isolated AC OA conservatively treated with ultrasound- or roentgen-guided intra-articular AC injection between January 2016 and December 2019 were included. Therefore, all included patients were treated with an initial AC injection at least 1 year before inclusion in this study. Diagnosis of AC OA was based on physical examination according to a standard protocol and was confirmed by radiographic imaging defined by the Claes Petersson grading system [13]. Regarding the physical examination, a positive diagnosis was confirmed in cases of local tenderness over the AC joint and at least one positive AC compression test among crossover adduction, O’Brien, or Bell-van Riet test [14-16]. To exclude any concomitant shoulder pathologies, all patients underwent ultrasound of the shoulder. Cases of previous AC injection or surgery on the AC joint were excluded. Cases of post-traumatic AC instability, glenohumeral OA, instability of the shoulder, active infection of the AC joint, and additional shoulder pathologies (e.g., m. biceps tear or tendinitis, partial or complete rotator cuff tear, rotator cuff calcification, or tendinosis) were also excluded.
Procedure
Identification of patients was performed using CTcue to filter the Electronic Patient Database. Eligibility was assessed by a researcher (NM) based on inclusion and exclusion criteria. After confirmed eligibility, patients were required to provide informed consent. After receiving consent, demographic and clinical data were extracted as well as data regarding shoulder function, pain relief, and baseline patient-reported outcome measures (PROMs). Demographic and clinical data consisted of age, sex, lateralization of AC OA, nonsteroidal anti-inflammatory drug (NSAID) use, reinterventions, and time to reintervention. Baseline PROMs were registered at the initial visit at a specialized outpatient shoulder clinic. In cases of no documentation of reintervention, patients were contacted to verify. In the absence of any reintervention at final follow-up, a questionnaire was sent.
Administration of Ultrasound-Guided or Radiograph-Guided AC Injection
All AC injections were performed by a senior shoulder orthopedic surgeon. Patients were treated with an intra-articular AC injection consisting of 1 mL Lidocaine (10 mg/mL) and 1 mL corticosteroid (Kenacort 40 mg/mL). All injections were performed under guidance of ultrasound or radiographic imaging. To identify the AC joint, the ultrasound probe was placed transversely over the acromion and clavicle. Subsequently, the probe was rotated in a longitudinal direction over the AC joint. From a posterior angle, a needle was inserted to identify the joint on ultrasound.
For radiographic imaging of the AC joint, patients were placed in the supine position on an examination table. Subsequently, the AC joint was palpated and marked. Using a needle, the AC joint was identified on a single-plane X-ray. Guided by the image, the AC joint was punctated, and the injection was performed. A standard follow-up procedure was applied in which patients were contacted 6 weeks after administration of the injection.
Outcome Measures
Primarily, the success rate of a single AC injection was assessed. Success was defined as the absence of any type of reintervention such as subsequent AC injections or surgery. Reintervention was considered the endpoint. In patients lost to follow-up, the date of the last visit to the outpatient clinic was considered the censoring date.
Secondary outcome measures were the Oxford Shoulder Score (OSS), the Subjective Shoulder Value (SSV), and the Numeric Rating Scale (NRS) score for pain at rest and during activity. The OSS is a widely used PROM to subjectively rate a combination of pain perception, shoulder function, and quality of life [16]. The SSV is a PROM used to rate subjective shoulder function in comparison to a normal functioning shoulder and is comprised of a single question: “If a normal functioning shoulder is 100%, how well does your shoulder function?” [17]. The NRS consists of an 11-point rating system for subjective pain perception. Scores range from zero to 10, with zero representing no pain and 10 representing extreme pain [18].
Statistical Analysis
Statistical analysis was mainly descriptive. Patients’ demographic and clinical characteristics are described as means with standard deviations (SDs) according to distribution. Categorical data are presented as numbers with accompanying proportions. Kaplan-Meier survival analysis was performed to calculate the 1-year success rate of a single corticoid injection with a 95% confidence interval (CI). Due to lack of power, univariate Cox regression analyses were performed to identify factors associated with injection failure and to calculate hazard ratios (HRs) with 95% CIs. Changes from baseline in PROMs were analyzed using paired t-tests. A P-value <0.05 was considered statistically significant. Due to the explorative nature of this study, adjustment for multiple testing was not performed.
RESULTS
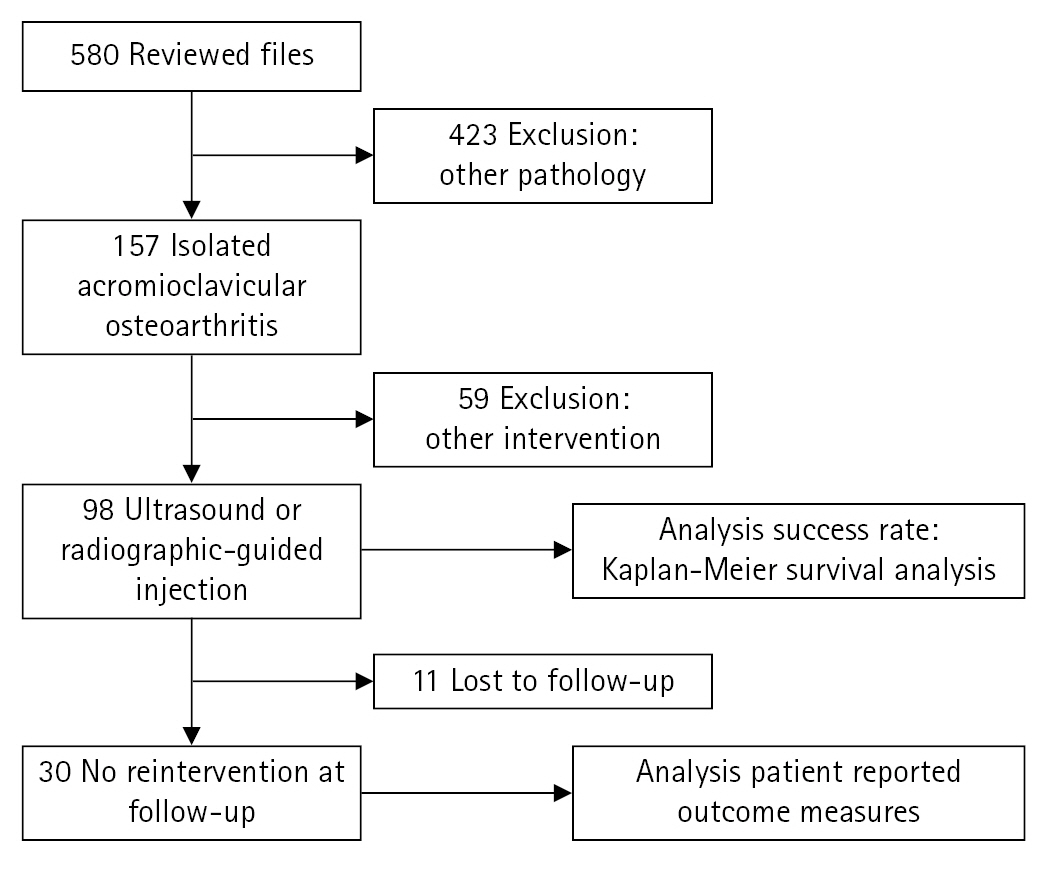
Five hundred eighty intra-articular AC injections were performed between January 2016 and December 2019. Of these, 482 patients were excluded due to coexisting pathology or interventions other than intra-articular AC injection. After applying inclusion and exclusion criteria, 98 patients remained. Finally, 30 patients (31%) were confirmed not to have undergone reintervention. Of these, 11 patients were lost to follow-up (Fig. 1).
Patient Population
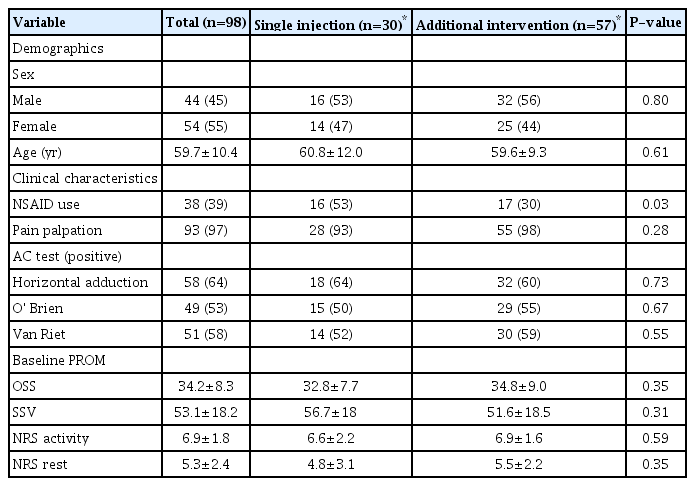
The study population had a mean age of 59.7±10.4 years and consisted of 44 males (45%) and 54 females (55%). Thirty-eight patients (39%) concomitantly used a form of NSAID daily at baseline (Table 1).
Success Rate
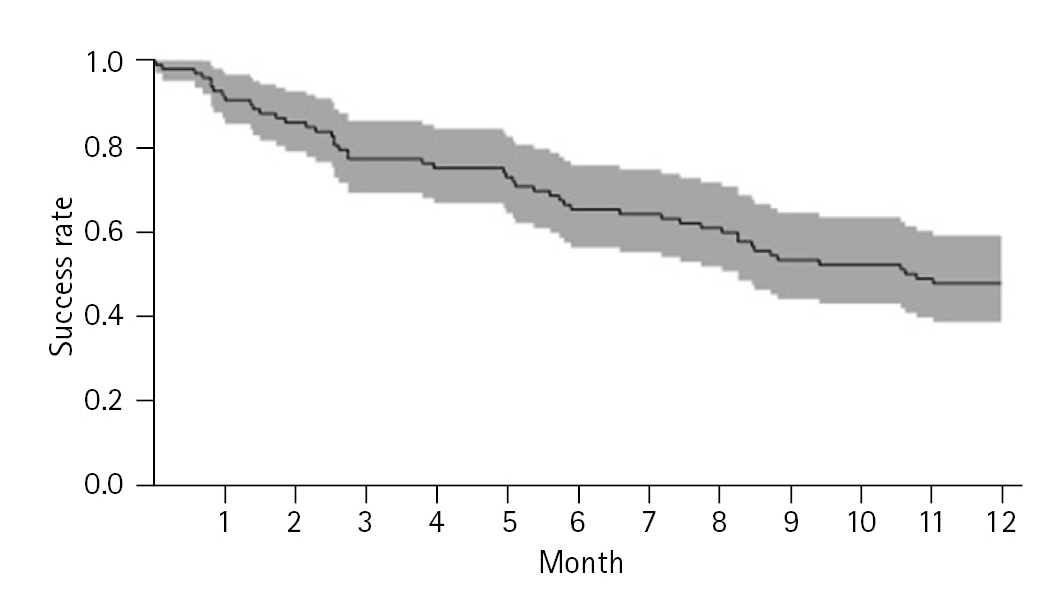
Median time to follow-up of all patients was 0.8 years (interquartile range [IQR], 0–6). In 57 of the total 98 patients (58%), the initial AC injection failed to resolve shoulder pain, requiring additional reintervention. Of these patients, 42 (74%) were treated with arthroscopic distal clavicle resection, five (12%) of whom were pre-administered a second AC injection, to no prevail. The other 15 patients (26%) requiring reintervention received a second AC injection and showed sufficient results. The median duration until reintervention was 0.5 years (IQR, 0–2.7). Forty-nine of 57 reinterventions (86%) occurred within the first year following the injection. Kaplan-Meier survival analysis yielded a 1-year success rate of 47% (95% CI, 37%–57%) (Fig. 2).
Predictive Factors Associated with Injection Success
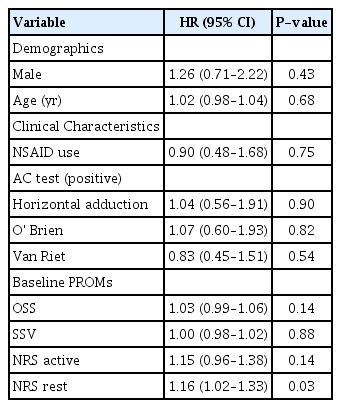
No patient demographics or clinical characteristics were significantly associated with success of injection. Regarding baseline PROMs, only the NRS score for pain at rest was significantly associated (P=0.03) with success of AC injection, with an HR of 1.16 (95% CI, 1.02–1.33) (Table 2).
PROMs at Final Follow-up
Among the 30 patients that had not undergone reintervention at final follow-up, 22 completed the questionnaire, a response rate of 73%. For these patients, mean time of final follow-up was 3.3±1.6 years. Significant improvement was seen between all baseline PROMs and final follow-up PROMs (P≤0.01 for all comparisons). Among all patients, OSS improved from 32.5±7.5 at baseline to 25.5±6.0 at final follow-up, while SSV improved significantly from 54.4%±18.4% to 76.3%±12.9%. Finally, significant improvement in NRS scores for pain at rest and during activity was observed, with changes from 5.1±2.8 to 2.4±3.1 at rest and 6.9±2.2 to 2.7±2.7 during activity (Table 3).
DISCUSSION
This study found a 1-year success rate of 47% of a single intra-articular AC injection in patients with isolated AC OA. Fifty-eight percent of all patients required reintervention by final follow-up, 86% of whom had required reintervention in the first year following administration of AC injection. The sole predictive factor associated with the likelihood for reintervention was the pain NRS score at rest at baseline. In patients that did not require reintervention at final follow-up, PROMs improved significantly in comparison to baseline.
In comparison to previous findings, the success rate of AC injections in our study was higher. van Riet et al. [12] showed only 28% of 58 patients with positive results from a single intra-articular AC injection. A study by Jacob and Sallay [10] concluded a 20-day mean duration of improvement due to AC injections, even though they failed to offer long-term effect for 81% of those patients.
These differences in success rates in comparison to our study may be explained by our specific selection of patients. First, we included only patients who were treated with ultrasound-guided or radiographic imaging-guided AC injections. van Riet et al. [12] and Jacob and Sallay [10] included patients in whom injection was administered without extra guidance. Research has shown that administration of AC injections under guidance of additional imaging is significantly more accurate, resulting in a significantly larger amount of patients with relief from pain. Without use of additional imaging, injections might not be administered in the AC joint. As a result, patients will have no, or less, pain relief [19-21]. Second, we included only patients who were diagnosed with isolated AC OA. In our sample of patients, diagnoses were based on an additional ultrasound of the shoulder to exclude other shoulder pathologies. While the works of van Riet et al. [12] and Jacob and Sallay [10] state that only patients with isolated AC OA are included, they do not explain the ruling out of other shoulder pathologies. Therefore, these previous results might have been influenced by concomitant pathologies to the shoulder.
Literature has proven that glucocorticosteroid injections are an excellent short-term treatment option for OA. In particular, triamcinolone acetonide (Kenacort) is effective in treating OA, insofar as it is the least soluble, injectable corticosteroid. While patients may still experience pain relief or improved functionality, research cannot conclude that these results are effects of the corticosteroid [19,22-24]. Furthermore, it remains to be discussed whether intra-articular injections are superior to other types of injections. Existing literature is not clear on this. Our study does not find demographic or clinical factors associated with likelihood of subsequent injection or surgery. However, patients who reported high pain levels at baseline were shown to have increased risk for reintervention. This may imply that pain at rest indicates the severity of the condition, with a higher risk of poor effects of injections in patients with higher levels of pain at rest.
On the part of physicians, it is beneficial for patients to be told that long-term improvement in a shoulder is a product of a return to a balanced state in the joint. In these cases, due to a combination of decreased inflammation, retraining of the joint, and a constant alteration of sensation, a new balanced state is achieved. But the true essence of pain relief is unclear and needs further research.
One strength of this study is homogeneity in its population. Patients were specifically selected for their isolated AC OA and for only receiving a single ultrasound-guided or radiograph-guided AC injection. Furthermore, our study had a follow-up of 0.8 years for all patients, which is long in comparison to most existing research [8,21]. Indeed, studies with mid- to long-term follow-up are scarce [11,12].
This study also has a few limitations. First, success of AC injection was defined as no reintervention (e.g., surgery or second injection). This allows for the possibility that patients may have retained a certain degree of pain, even in cases defined as a success, yielding potential overestimation in our success rate. However, due to the retrospective design of our study, it was beneficial to define a hard outcome to prevent recall bias. Second, also due to the retrospective design of our study, no á priori power analysis could be performed, creating the possibility of an underpowered association. While our study sample is the largest among other research in mid- to long-term success rates of AC injections, the study sample is small. Additionally, due to its retrospective design, the possibility for selection bias exists. Finally, 11 of 98 patients were lost to follow-up. Future research would benefit from analysis of differences in efficacy of injections between a control group with AC OA and an intervention group in a prospective design.
CONCLUSIONS
This study shows that single intra-articular AC injections in patients with AC OA produce a 1-year success rate of 47%. Single AC injections were shown to produce good mid- to long-term clinical outcomes regarding shoulder function and pain perception in one-third of patients. Further research is essential to analyze mid- to long-term outcomes of AC injections.
Notes
Author contributions
Conceptualization: NM, RJMV, TDWA, IS, AVN. Data curation: NM, IS. Formal Analysis: IS, AVN. Investigation: NM. Methodology: NM, TDWA, IS, AVN. Project administration: NM. Resources: RJMV. Supervision: TDWA, IS, AVN. Validation: TDWA, IS, AVN. Visualization: AVN. Writing – original draft: NM, RJMV. Writing – review & editing: RJMV, TDWA, AVN.
Conflict of interest
None.
Funding
None.
Data availability
Contact the corresponding author for data availability.
Acknowledgments
None.