Prevalence of incidental distal biceps signal changes on magnetic resonance imaging
Article information
Abstract
Background
Knowledge of the base rate of signal changes consistent with distal biceps tendinopathy on magnetic resonance imaging (MRI) has the potential to influence strategies for diagnosis and treatment of people that present with elbow pain. The aim of this study is to measure the prevalence of distal biceps tendon signal changes on MRIs of the elbow by indication for imaging.
Methods
MRI data for 1,306 elbows were retrospectively reviewed for mention of signal change in distal biceps tendon. The reports were sorted by indication.
Results
Signal changes consistent with distal biceps tendinopathy were noted in 197 of 1,306 (15%) patients, including 34% of patients with biceps pain, 14% of patients with unspecified pain, and 8% of patients with a specific non-biceps indication. Distal biceps tendon changes noted on radiology reports were associated with older age, male sex, and radiologists with musculoskeletal fellowship training.
Conclusions
The finding that distal biceps MRI signal changes consistent with tendinopathy are common even in asymptomatic elbows reduces the probability that symptoms correlate with pathology on imaging. The accumulation of signal changes with age, also independent of symptoms, suggests that tendon pathology persists after symptoms resolve, that some degree of distal biceps tendinopathy is common in a human lifetime, and that tendinopathy may often be accommodated without seeking care.
Level of evidence
IV.
INTRODUCTION
Distal biceps tendinopathy is sometimes misleadingly referred to as a “partial tear” [1-3]. Acute traumatic ruptures of the distal biceps tendon are complete avulsions from the radial tuberosity. The misnomer “partial tear” might arise from the fact that new pains from tendinopathy are often misperceived as an injury, but a convincing link to trauma is not established [4,5]. The term “partial tear” has the potential to reinforce these types of unhelpful thoughts.
Distal biceps tendinopathy is associated with increased signal on magnetic resonance imaging (MRI) from changes in the tendon near the radial tuberosity with or without thinning or thickening of the tendon [3]. Incidental signal changes in tendons and entheses are common on MRI of the elbow and wrist [6-8]. In addition, symptoms from tendinopathies and enthesopathies are generally temporary while MRI signal changes are likely permanent and may not correspond with symptoms [6-8]. This creates a circumstance of notable potential for signal changes that are unrelated (incidental) to symptoms. Ascribing symptoms to incidental findings is a form of overdiagnosis that can lead to overtreatment.
Most enthesopathies of middle age are self-limiting, but symptomatic distal biceps tendinopathy is less common in musculoskeletal specialty care as compared for instance to enthesopathy of the extensor carpi radialis brevis (ECRB) origin, so-called lateral epicondylitis. While the natural history of enthesopathies such as lateral epicondylitis and plantar fasciitis is resolution of symptoms over time, the natural history of untreated distal biceps tendinopathy is debated [1,9]. Given that enthesopathies and tendinopathies can cause prolonged symptoms of more than a year of duration, it might seem like they will not resolve without intervention [9]. If the natural history of distal biceps tendinopathy is a temporary period of symptoms which nevertheless in many patients lasts more than a year, then people can choose to avoid surgery. Given that full recovery from injury or surgery takes about a year, surgery could conceivably prolong recovery in some patients [1,3,10,11]. A notable prevalence of incidental signal changes consistent with distal biceps tendinopathy in people with either no symptoms or uncharacteristic symptoms, particularly if the prevalence increases with age, might indicate that distal biceps tendinopathy is common even though presentation for care of symptoms related to distal biceps tendinopathy is not. This would indicate that distal biceps tendinopathy is typically accommodated without formal medical care and also that it is likely self-limited, as are many other enthesopathies and tendinopathies.
This study estimates the base rate of distal biceps tendinopathy by measuring differences in the prevalence of signal changes consistent with distal biceps tendinopathy in radiology reports of elbow MRIs ordered for biceps symptoms, for nonspecific elbow pain, and for specific non-biceps indications. These three groups would be expected to present with different tendinopathy rates, with the latter group most closely approximating a population base since the tendinopathy-related signal changes in the biceps are likely asymptomatic and incidental. We also studied the association of age, sex, and musculoskeletal fellowship training of the evaluating radiologist with the prevalence of recorded distal biceps signal changes on elbow MRI.
METHODS
This study received approval from the Institutional Review Board of the University of Texas at Austin (No. 2019010148). After review by the Institutional Review Board of the University of Texas at Austin, informed consent was waived. This study has been performed in accordance with the ethical standards in the 1964 Declaration of Helsinki. This study has been carried out in accordance with relevant regulations of the US Health Insurance Portability and Accountability Act (HIPAA).
Study Design and Setting
After institutional review board approval of this retrospective study, we obtained radiology reports for elbow MRI that were read by 14 radiologists from one regional radiology service. We included patients aged 18 to 89 years old who had an elbow MRI with proton density and T2 sequences from January 2016 through December 2018. We excluded patients with an antecubital fossa tumor, surgery, trauma, or infection that could distort the distal biceps. We searched diagnosis codes and full text of the radiology reports. In total, 1,306 radiology reports were evaluated for analysis. There were no standard protocols for making images or documenting the interpretation.
Outcome Measures
Our primary measure was a record of signal changes consistent with distal biceps tendinopathy in the MRI report. We searched the reports using the key words “distal,” “biceps,” “tendinosis,” “tendinopathy,” “partial,” and “tear” in order to identify potential signal changes. One of us reviewed all of the reports to verify the 197 elbow MRIs in which the radiologist felt that changes consistent with distal biceps tendinopathy were present (Fig. 1).
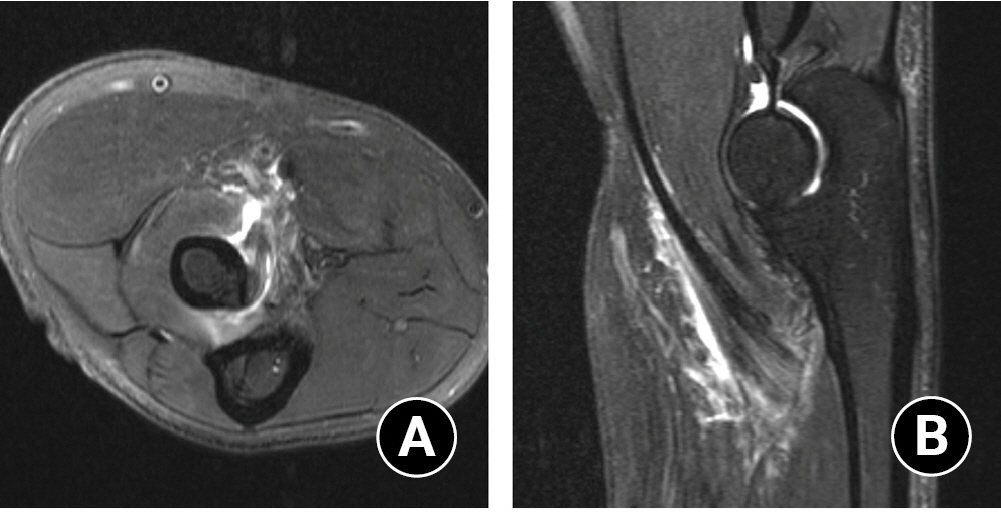
Axial (A) and sagittal (B) T2-weighted fat suppressed magnetic resonance images with prominent thickening and edema-like signal involving the distal biceps tendon as it approaches at its insertion on the radius.
The indication for MRI was categorized into three groups: biceps pain (n=257, 20%), unspecified pain (n=388, 30%), and specific non-biceps indications (n=661, 50%). Implication of the biceps was inclusive: it was defined by either explicit inclusion of the word “biceps” in the patient history recorded in the radiology report or a less specific history (e.g., elbow pain after lifting a heavy weight) that seemed consistent with potential biceps pathophysiology. Less specific descriptions of potential distal biceps pain were present for 36 (14%) out of the 259 classifications of biceps pain. Specific non-pain indications included evaluation of bumps (81 patients), numbness (75 patients), and infection/wound (8 patients). Specific non-biceps pain included evaluation of other elbow pains (e.g., lateral, 171 patients; medial, 99 patients; or posterior, 64 patients), stiffness/arthrosis/synovitis (82 patients), and sprain/strain/contusion/fracture/fall (99 patients) that would not involve the biceps. All other indications, including vague histories such as “right elbow pain,” were included in evaluation of unspecified pain (367 patients). Factors evaluated for association with radiologist description of tendinopathy in the distal biceps included age at the time of imaging, sex, and whether the radiologist assessing the MRI had completed a musculoskeletal imaging fellowship.
Statistical Analysis
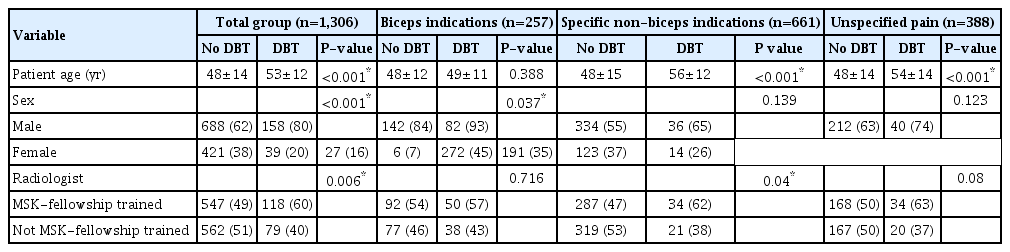
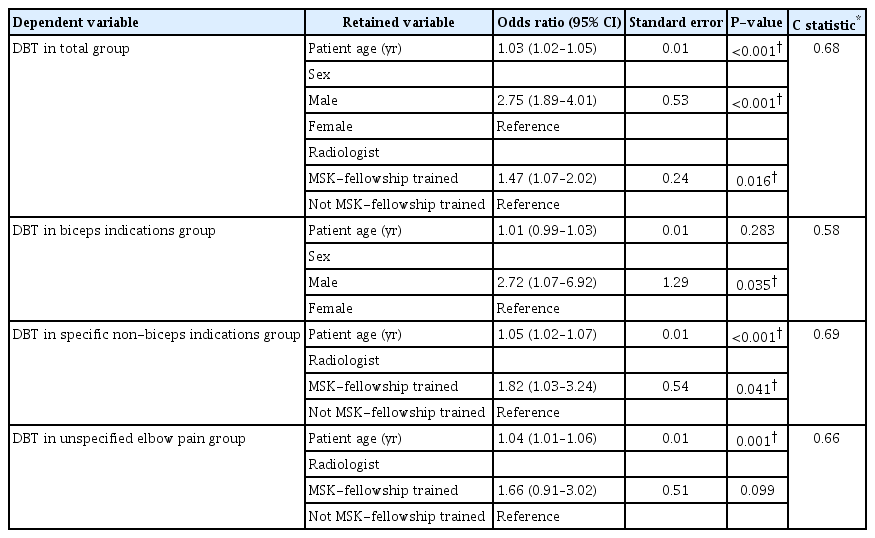
Continuous variables are presented as mean±standard deviation and discrete data as proportions. We used the Student t-test to assess differences between continuous variables and dichotomous variables and the Fisher exact tests for discrete variables. Our primary dependent variable (presence of signal changes consistent with distal biceps tendinopathy) was binary and was used for bivariate and multivariable analysis. We created four multivariable logistic regression models to assess factors independently associated with the presence of signal changes consistent with distal biceps tendinopathy in the total group and the no suspected biceps symptoms group. We included all variables with a P<0.10 on bivariate analysis for the entire cohort in the final model for a parsimonious multivariable model (Table 1). We considered P<0.05 significant for multivariable logistic regression models.
RESULTS
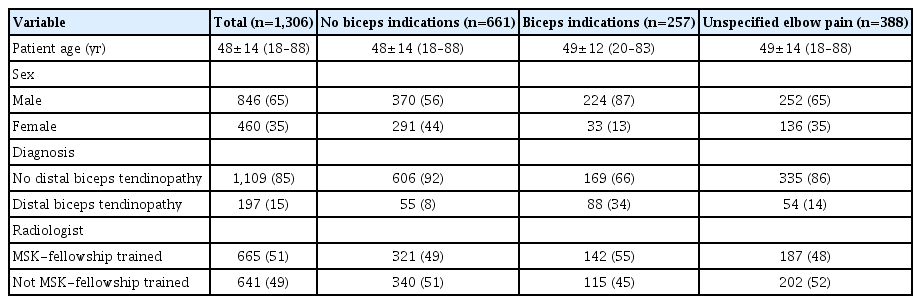
Signal changes consistent with distal biceps tendinopathy were noted in 197 of 1,306 (15%) reports including: 88 of the 257 (34%) reports classified as biceps indications, 54 of 388 (14%) reports associated with unspecified pain, and 55 of 661 (8%) reports classified as specific non-biceps indications for MRI (P <0.001) (Table 2). In the latter group–the one that best represents the population-based prevalence of MRI signal changes consistent with distal biceps tendinopathy–the prevalence of that condition was about 5% in the 30 to 50 year age group, 9% in the 50 to 60 year age group, and 19% (nearly 1 in 5 people) after age 60. Assuming that everyone with a biceps indication had symptoms from distal biceps tendinopathy, the Bayes-adjusted positive and negative predictive values of MRI for this condition are 37% and 90%, respectively.
In bivariate analysis of the entire cohort, signal changes consistent with distal biceps tendinopathy were more common with older age, male sex, and when the images were interpreted by a radiologist who did a musculoskeletal imaging fellowship (Table 1). All three variables were retained in multivariable analysis (Table 3). Among people imaged for biceps indications, signal changes consistent with distal biceps tendinopathy were associated with male sex in bivariate and multivariable analyses (Tables 1 and 3).
In the group imaged for unspecified elbow pain, there was an association between the presence of distal biceps tendinopathy and patient age in both bivariate and multivariable analyses (Tables 1 and 3). Among people imaged for specific non-biceps indications, signal changes consistent with distal biceps tendinopathy were associated with older age and radiologists with musculoskeletal fellowship training on bivariate and multivariable analyses (Tables 1 and 3).
DISCUSSION
Contrary to the current tendency to refer to distal biceps tendinopathy as a “partial tear,” and thus imply an unfavorable natural history meaning that the disease must be treated, it is possible that distal biceps tendinopathy is one of the common incidental tendinopathies and enthesopathies of middle age with a pathophysiology of mucoid degeneration rather than injury, overuse, or inflammation, and a benign, self-limited natural history [9,12]. Estimates based on incidental changes in the origin of the ECRB suggest that at least 1 in 7 adults will have an enthesopathy of ECRB origin in their lifetime. If the same is true for distal biceps tendinopathy, then it seems likely that many patients with these common conditions have few symptoms, adapt well to symptoms, or find them problematic but do not seek medical attention [6-8]. Furthermore, if evidence emerges that distal biceps tendinopathy is relatively common over a human lifetime, and signal changes consistent with tendinopathy are prevalent and permanent, we may need to be cautious about a potential base rate fallacy. According to Bayes’ theorem, interpretation of diagnostic tests is affected by prevalence of symptomatic and asymptomatic disease. A high prevalence of incidental tendinopathy unrelated to presenting symptoms increases the risk of misdiagnosis of distal biceps tendinopathy as the source of symptoms and overtreatment of the imaging finding.
Among patients undergoing MRI of the elbow for any cause, we found that signal changes consistent with tendinopathy of the distal biceps are present in up to 15% of the population and are likely incidental, more so with older age. By establishing a notable mean base rate of at least 9% among people having an elbow MRI for problems unrelated to the biceps, and at higher rates in older age groups, one can infer that distal biceps tendinopathy is seemingly much more common than the rate a specialist encounters among people seeking care for distal biceps tendinopathy [1]. That would indicate that far more people experience the condition than seek treatment for it. Based on this, one could then infer that the natural history of distal biceps tendinopathy might be symptoms that are often accommodated, as well as typically temporary (self-limited)—a hypothesis that would need a longitudinal study to confirm or refute. This inference has face validity given that many of the most common enthesopathies (e.g., enthesopathy of the extensor carpi radialis brevis origin) are very common and therefore likely to be accommodated and generally self-limiting.
This study has some limitations. The categorization of the reports by indication depended upon the history provided in the radiology report rather than clinical notes. Nearly a third of these were nonspecific. Some of the patients in the unspecified pain cohort may have had symptoms from distal biceps tendinopathy. Therefore, we intentionally kept this group separate. Given that the data was drawn from MRIs that were ordered by both specialists and non-specialists, the unspecified pain group might include people referred by a non-specialist; had those people seen a specialist, the clinical diagnosis of distal biceps tendinopathy may have been made. The relatively comparable prevalence of signal changes consistent with distal biceps tendinopathy in the unspecified group compared to the specific non-biceps indication group suggests that this was relatively uncommon. We were only interested in tendon changes sufficient to be noticed and recorded by a musculoskeletal radiologist in a formal report. Lesser changes might have been detected on direct review of the MRI, which would increase the base rate of tendinopathy. Several other limitations would likely also err towards an increased prevalence including the variation between radiologists, the absence of standard protocols for taking images or documenting the interpretation, heterogeneity in scanning protocols that are not specific to distal biceps evaluation, and heterogeneity in the strength of the MRI used in the evaluation of the elbow (a 3.0 Tesla magnet is likely more sensitive). Since all of these factors would likely increase the prevalence of incidental MRI signal changes consistent with distal biceps tendinopathy, we can be confident that if we were able to control these factors it could further support our findings. We did not study the interobserver reliability or accuracy of the readings. In our opinion, a study of MRIs by trained specialist musculoskeletal radiologists using specific MRI sequences and scanning planes to detect distal biceps pathophysiology with reliable interpretation strategies would be more likely to increase rather than decrease the prevalence of distal biceps tendinopathy.
The observation that MRI signal changes consistent with distal biceps tendinopathy are more common among people with biceps/anterior elbow pain indications is expected, and the prevalence of tendinopathy signal changes in a notable percentage of the other categories points to a likely notable base rate of asymptomatic or accommodated tendinopathy in the general population. It is a little surprising that among people with a biceps-specific indication, only 34% overall had MRI findings of tendinopathy. This may in part reflect inaccuracy and unreliability of diagnosis of distal biceps tendinopathy-based symptoms and signs, in part our inclusiveness in this category which included relying on a brief history recounted in the radiologist reports, and in part that some pathophysiology causing symptoms are not detected on MRI. Future research is needed to determine which of these factors is more important, but it seems safe to assume for the time being that diagnosis based on symptoms and signs should be made with caution. The observation that one in five patients over 60 have incidental tendinopathy signal changes in the distal biceps suggests that distal biceps tendinopathy is a common aspect of human existence and that the symptoms are typically accommodated. A study of people not seeking care could determine the rate of biceps related symptoms and signs that are being accommodated in the general population. These types of population-based studies done for knee osteoarthritis and rotator cuff tendinopathy have identified a high prevalence of accommodated symptoms and there is no reason to believe that the situation would be different for distal biceps tendinopathy or enthesopathy of the extensor carpi radialis brevis origin [13-15].
The observation that radiologist reports of MRI signal changes consistent with distal biceps tendinopathy are associated with older age and men is consistent with prior evidence. Studies note an increased prevalence of people seeking care for distal biceps tendinopathy in the fifth and sixth decades of life. The finding that signal changes in the distal biceps tendon were increasingly common as age increased suggests that signal changes may be permanent even if the symptoms resolve. This observation is also consistent with studies of other enthesopathies of the upper extremity that note an increasing prevalence with age [6-8]. This circumstance allows the study of MRI obtained for non-biceps indications to function as a population-based study of the accumulating, lifetime prevalence of distal biceps tendinopathy.
The variation in mention of distal biceps tendinopathy by the training of the reading radiologist is consistent with other studies that report inter-rater reliability in the diagnosis of other studies involving distal biceps tendinopathy using MRI. According to Festa et al., the sensitivity and specificity of MRI for detecting tendinopathy in 22 people was 59% and 100% respectively, which was worse than those of MRI for detecting 24 avulsions of the distal biceps insertion [16]. Lynch et al. found that the accuracy of MRI for complete avulsion of the distal biceps tendon insertion (86%) was greater than that for distal biceps tendinopathy (67%) [17].
CONCLUSIONS
MRI findings of distal biceps tendinopathy are relatively common, even among people undergoing MRI for reasons unrelated to the biceps. Knowledge of this base rate leads to several inferences that may alter patient and surgeon perceptions of this condition, which might in turn alter diagnostic and treatment strategies. Distal biceps tendinopathy appears spontaneous, benign, and self-limiting, as well as unrelated to trauma, arm use, or inflammation. The term “partial tear” is misleading: “distal biceps tendinopathy” is the preferred, descriptive term. Correcting common misinterpretations of symptoms–viewing new pain as a repairable injury, believing prolonged symptoms require treatment, and associating painful activity as worsening the problem–is essential to patient's choices align with their values. Another reason this is important is the lack of evidence that surgery, extracorporeal shock wave therapy, or corticosteroid or platelet-rich plasma injections alter the natural history of symptoms or alleviate symptoms better than simulated (placebo) treatments. These interventions may increase false hope, discomfort, and inconvenience, and may cause potential financial, psychological, and iatrogenic harm [1,10,11,18,19]. Ensuring that patients understand the self-limiting natural history of many enthesopathies and tendinopathies, the uncertain benefit of interventions, and the value of supportive treatments can empower them to make informed choices, avoid unnecessary tests, and accommodate symptoms.
Notes
Author contributions
Conceptualization: EK, DR. Data curation: EK. Formal analysis: EK, JTPK. Investigation: EK, JTPK, DR. Methodology: EK, DR. Supervision: DR. Validation: DR. Writing-original draft: EK. Writing-review & editing: JTPK, AIG, DR, LMR.
Conflict of interest
DR has or may receive payment or benefits from Skeletal Dynamics, Wright Medical for elbow implants, Deputy Editor for Clinical Orthopaedics and Related Research, Universities and Hospitals, Lawyers outside the submitted work. No other potential conflicts of interest relevant to this article were reported.
Funding
None.
Data availability
None.
Acknowledgments
None.