Glenohumeral versus subacromial steroid injections for impingement syndrome with mild stiffness: a randomized controlled trial
Article information
Abstract
Background
The subacromial (SA) space is a commonly used injection site for treatment of impingement syndrome. For shoulder stiffness, glenohumeral (GH) injections are commonly performed. However, in cases of impingement syndrome with mild shoulder stiffness, the optimal site of steroid injection has yet to be identified.
Methods
This prospective, randomized study compared the short-term outcomes of ultrasound-guided GH and SA steroid injections in patients who were diagnosed with impingement syndrome and mild stiffness. Each group comprised 24 patients who received either a GH or SA injection of 40 mg of triamcinolone. Range of motion and clinical scores were assessed before and 3, 7, and 13 weeks after the injection.
Results
GH and SA injections significantly improved the range of motion and clinical scores after 13 weeks of follow-up. Notably, targeting the GH joint resulted in an earlier gain of forward elevation, external rotation, and internal rotation in 3 weeks (P<0.001, P=0.012, and P=0.002, respectively) and of internal rotation and a Constant-Murley score in 7 weeks (P<0.001 and P=0.046). Subsequent measurements were similar between the groups and showed a steady improvement in all ranges of motion and clinical scores.
Conclusions
GH injections may be more favorable than SA injections for treatment of impingement syndrome with mild stiffness, especially in improving the range of motion in the early period. However, the procedures showed similar outcomes after 3 months.
Level of evidence
I.
INTRODUCTION
Impingement syndrome is a frequently occurring shoulder disorder caused by compression or friction of the rotator cuff tendons and subacromial (SA) bursa against the SA arch [1]. This condition results in pain when elevating the shoulder, which often leads to a limited range of motion (ROM), causing secondary shoulder stiffness [2].
Steroid injection is a recognized treatment option for both impingement syndrome and shoulder stiffness [3]. Its purpose is to reduce inflammation and pain, thereby improving function and ROM in the shoulder joint [4]. However, the effectiveness of steroid injections may depend on the site of injection, specifically in relation to the primary diagnosis. While SA injections are essential in treating bursal inflammation and impingement syndrome, glenohumeral (GH) injections are more effective in managing capsular inflammation, which is commonly observed in shoulder stiffness [5,6].
Despite the commonality of impingement syndrome with a resultant “mild” (defined in the Methods section) stiffness in the outpatient setting, there is a shortage of literature regarding the optimal injection site. It remains to be determined if addressing bursal pain through an SA injection will ultimately relieve stiffness, or if targeting the stiff capsule with a GH injection will provide a better outcome in terms of function. Several studies have compared injection sites in primary shoulder stiffness [5,7]; however, no study has yet to directly compare the two methods in treating impingement syndrome. Therefore, the current study aimed to compare the effectiveness of ultrasound-guided steroid injections in the SA and GH spaces for treating impingement syndrome with mild stiffness.
METHODS
This study was approved by Institutional Review Board of Hallym University Chuncheon Sacred Heart Hospital (No. 2012-96). Informed consent was obtained from all patients.
Patient Enrollment
Following approval from the Institutional Review Board, and in compliance with the Declaration of Helsinki, a prospective randomized controlled trial was conducted from January 2013 to June 2014, involving 56 patients diagnosed with shoulder impingement syndrome with mild stiffness (ClinicalTrials ID: NCT06051370). Impingement syndrome was diagnosed based on a positive Hawkin’s sign and radiographic findings (rotator cuff with intact continuity but tendinosis confirmed by magnetic resonance imaging (MRI) or ultrasound, with a possible SA enthesophyte) [8]. “Mild” stiffness was defined in this study as the degree of that permits daily activity but often causes endpoint range-of-motion pain [9]. It was specified as meeting two or more of the following criteria in both passive and active shoulder ROM: abduction between 110° and 150°, forward elevation (FE) between 120° and 140°, external rotation at the side (ER) between 30° and 50°, and internal rotation at 90° of abduction (IR) between 30° and 50°.
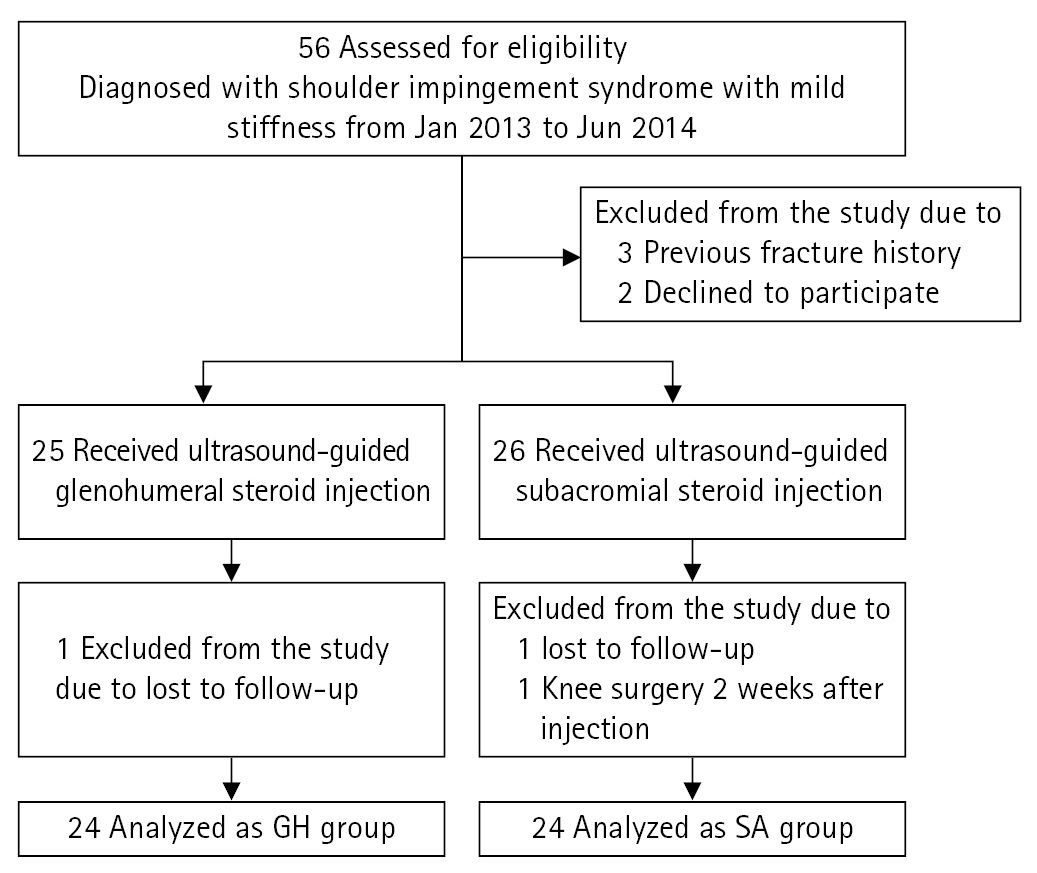
Patients were excluded from the study if they (1) refused to undergo ultrasound-guided injection, (2) were diagnosed with a rotator cuff tear, calcific tendinosis, or biceps pathology, (3) had a history of operation, fracture, or nerve injury of the shoulder, or (4) received treatment apart from the protocol conducted during this study. A final number of 51 patients was enrolled in the trial and randomly assigned to either the GH ultrasound-guided injection group (GH group) or the SA ultrasound-guided injection group (SA group). Double-blinded randomization was performed by an independent nurse using a computer-generated random sequence. A musculoskeletal radiologist (MSH) with more than 20 years of experience performed diagnostic ultrasound and MRI interpretations. A shoulder specialist (JTH) with more than 10 years of experience performing ultrasound-guided injections. A blinded orthopedic resident and nurse carried out the physical examination and clinical scoring. After the final follow-up, 48 patients (24 in each group) were eligible for analysis (Fig. 1).
Treatment and Follow-up Protocol
A diagnostic ultrasound was first performed using a 5- to 12-MHz linear probe (Philips Healthcare) to rule out shoulder pathology other than impingement syndrome. Using a 21-gauge spinal needle, a solution of 1 mL triamcinolone, 4 mL 1% lidocaine, and 7 mL 0.9% normal saline was injected under ultrasound guidance using 5- to 13-MHz linear probe (GE Healthcare) into either the GH space through the posterior approach or the SA space through the anterolateral approach (Fig. 2) [10]. The patients were then observed in 3, 7, and 13 weeks after the injection. Oral aceclofenac 100 mg twice daily and omeprazole 20 mg once daily were prescribed during the follow-up. Stretching exercises in all ranges of motion commenced in the 3rd week. Using a wand, patients were instructed to passively stretch their shoulders to an endpoint where pain is felt and maintain that position for at least 30 seconds, five sessions a day, 5 minutes per session. Rubber-band strengthening was added in the 7th week, with a concentration on ER. Using a rubber band (Thera-band, Hygienic Corp.) tied into a loop, the patients were instructed to maintain maximum painless external rotation for 30 seconds, five sessions a day, 5 minutes per session. The tension of the rubber band was based on the patients’ ability to maintain painless maximum rotation for 30 seconds.

Ultrasound-guided steroid injection. (A) Glenohumeral injection. The needle was introduced intra-articularly through a posterior approach. The injection solution as marked by the asterisk (*) is visualized between the cuff/capsule and the humeral head. (B) Subacromial injection. The needle is introduced through an anterolateral approach between the deltoid and the rotator cuff. Bulging of the subacromial bursa during injection as indicated by the triangle (▲) is demonstrated.
Clinical Assessment and Data Collection
Patient information, including age, sex, duration of symptoms, affected side, and hand dominance, was recorded. The following assessments were performed at baseline and at follow-up visits in weeks 3, 7, and 13: ROM in FE, ER, and IR, pain visual analog scale (pVAS), American Shoulder and Elbow Surgeons (ASES) score, and the Constant-Murley (Constant) score. The ASES score was chosen because it has been verified as best reflecting the activities of daily life [11], while strength was evaluated through the Constant score [12] Improvement in ROM was calculated by subtracting the pre-injection measurements from the measurements at each follow-up visit.
Statistical Analysis
A power analysis determined that a sample size of 42 patients (21 per group) would be sufficient to have an 80% statistical power to detect a significant difference in the improvement of the Constant score between pre-injection and 7-week post-injection, with a two-sided α level of 0.05. An effect size of 0.89 was assumed based on the mean difference and standard deviation of improvement in the Constant score between pre-injection and 7-week post-injection in a pilot study of 20 patients.
Normal distribution was checked using the Kolmogorov-Smirnov test. The independent-samples t-test or the Mann-Whitney U-test were used to analyze continuous data, while the paired-sample t-test was used for an intra-group comparison of serial measurements. Categorical data were analyzed using Pearson’s chi-square test. Continuous data were described as mean±standard deviation, and categorical data were described as a percentage. Analyses were performed using IBM SPSS ver. 25 (IBM Corp.), and a P-value below 0.05 was considered statistically significant.
RESULTS
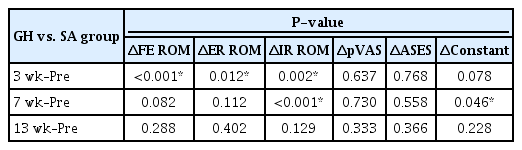
The demographic data and pre-injection baseline clinical evaluation results were comparable between the two groups (Table 1). Significant improvement in ROM and clinical scores were observed within both groups from pre-injection to the final 13-week follow-up (Table 2). Generally, an early improvement of ROM was observed in the GH group in 3 weeks (Table 3).
Both groups exhibited significant improvement in ROM, pain, and clinical scores from pre-injection to the final follow-up at 13 weeks (Table 2). However, the GH group demonstrated an earlier gain of FE, ER, and IR ROM in 3 weeks (P<0.001, P=0.012, and P=0.002) and of ER and the Constant score in 7 weeks (P<0.001 and P=0.046) compared to the SA group (Table 3, Fig. 3). Nevertheless, the improvements between the two groups were similar in subsequent follow-ups (Table 3, Fig. 3)
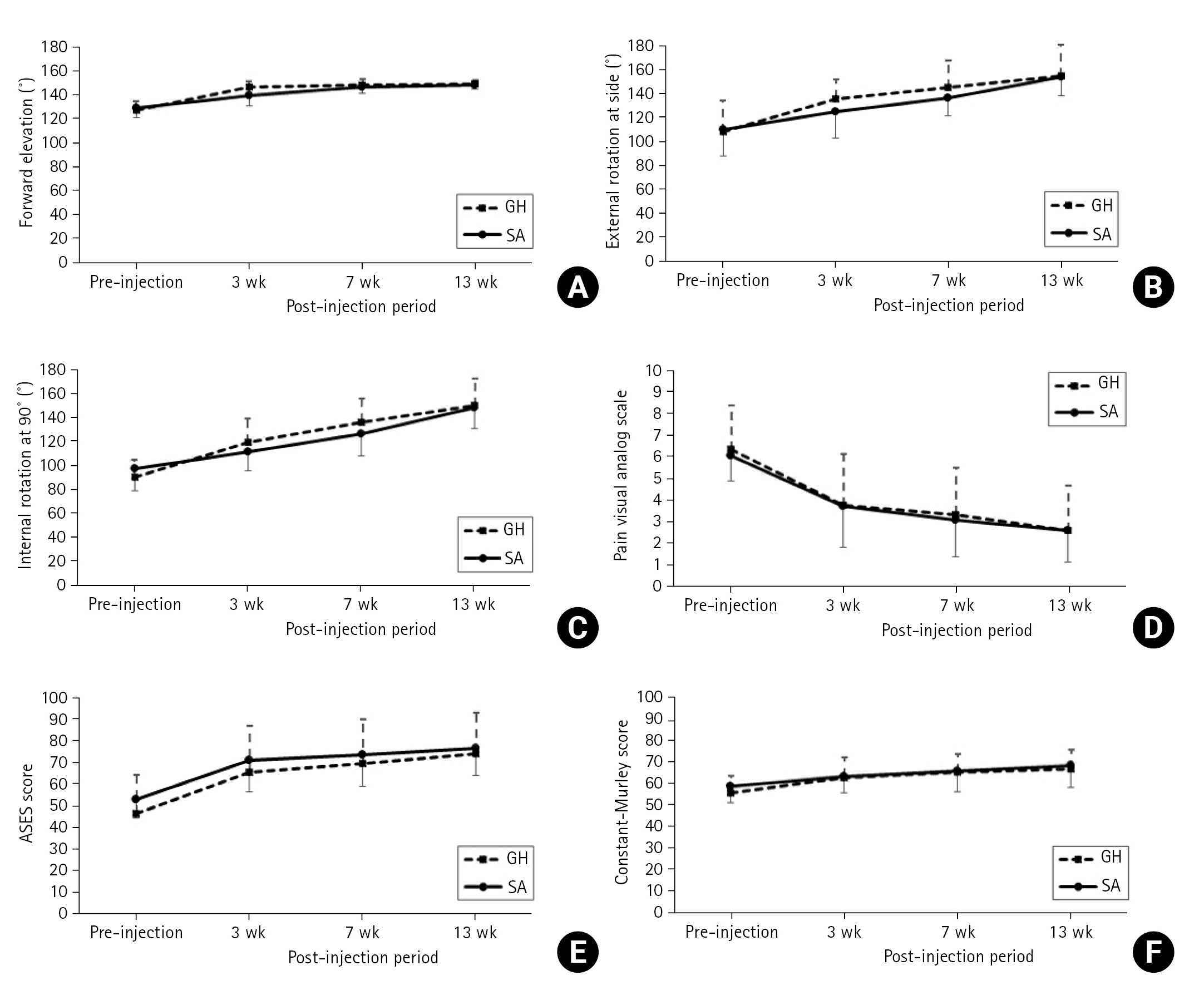
Serial measurements from pre-injection to last follow-up. (A) Forward elevation. (B) External rotation at side. (C) Internal rotation at 90˚ of shoulder abduction. (D) Pain visual analog scale. (E) American Shoulder and Elbow Surgeons (ASES) score. (F) Constant-Murley score. GH group: ultrasound-guided glenohumeral steroid injection, SA group: ultrasound-guided subacromial steroid injection.
DISCUSSION
The SA space has traditionally been the preferred injection site for treating impingement syndrome [8]. However, in cases of mild stiffness, the current study suggests that GH injections may lead to an earlier improvement than the SA approach, within 7 weeks post-injection. Overall, injection targeting the GH joint resulted in a general earlier gain of ROM. Contrary to common perception, there was no significant advantage of SA injections over GH injections in terms of reducing pain. Nonetheless, both injection groups demonstrated a significant improvement in symptoms, with no discernible difference between the two groups after 13 weeks.
Various studies have examined the accuracy of SA and GH injections. A direct comparison of the two techniques was conducted by Eustace et al. [6]. In their study, the injections were performed without ultrasound guidance. Nevertheless, the accuracy of the SA injections was 29%, whereas that of the GH injections was 42%. The results demonstrated that the GH injections had a higher success rate, which was associated with better clinical outcomes.
The accuracy of SA injections is often questioned and has been intensively investigated. Precise, isolated infiltration of the SA bursa is difficult as the bursa is normally collapsed into a thin layer [13]. Moreover, in pathologic scenarios, adhesion and thickening of the walls are common [14]. Several studies have reported success rates for SA injections ranging from 69% to 83%. However, within these successful cases, 46%–75% have also infiltrated other structures, including the subcutaneous layer, deltoid, rotator cuff, and GH joint [10,15–17].
The GH joint consists of an “actual” space between two directly articulating bones with a joint capsule surrounding the joint cavity. The interval between the round humeral head and the relatively flat upper glenoid is readily available for injection with a reliable “loss-of-resistance” to aid in precise needle placement [18]. Unlike SA injections, in which even a successful procedure may cause direct contact with the steroid to the posterosuperior rotator cuff, in GH injections, the superior capsule covers the underside of the rotator cuff, and its non-dependent position away from gravity dispersion may minimize direct steroid-to-tendon infiltration [19]. Not limited to an established treatment of primary shoulder stiffness, the safety and efficacy of postoperative GH steroid injections to treat pain and stiffness after rotator cuff repair have been repeatedly reported [20,21].
The preferred technique needs to be identified. An ideal injection site for steroids would be the first choice, where the success rate is higher in placing the intended injection. The second choice would be the technique whereby the deleterious effects of the steroids can be minimized. In this aspect, the current study showed there is no reason to insist on traditional SA injections for the treatment of impingement syndrome, especially when there is concomitant stiffness.
This study had some limitation. First, the follow-up rate was short, spanning approximately 3 months. Long-term follow-up may permit further comparison regarding the incidence of a subsequent injection or even a rotator cuff tear. However, as this was an outpatient investigation based on conservative treatment for a relatively mild disease state, 3 months of evaluation may have been sufficient to reveal meaningful results, as they were for other studies regarding injection treatments [5,22]. Second, as this was an outpatient-based study, patient compliance and the effect of oral anti-inflammatory medication may have been confounding factors. Nonetheless, the same amount of oral medication was prescribed, and patient instruction on adhering to the treatment protocol was conducted throughout the study. Therefore, the difference in outcomes could be predominantly attributed to the only independent variable—the injection method. Another study limitation was its relatively small sample size. Although some statistically significant findings were derived, a follow-up study with a greater number of participants, and perhaps with a third arm of sham injection, may be needed. Despite these limitations, this study was the first to elucidate an infrequently discussed but relatively common disease entity observed in everyday practice.
CONCLUSIONS
GH injections may be preferable to SA injections for the treatment of impingement syndrome with mild stiffness, notably in gaining ROM in the early period. However, the two procedures showed similar outcomes regarding pain, ROM, and clinical scores after 3 months.
Notes
Author contributions
Conceptualization: JTH. Data curation: TYK. Formal analysis: YTK, TYK. Supervision: JTH. Validation: YTK. Writing–original draft: YTK, TYK. Writing–review & editing: JBL.
Conflict of interest
Jung-Taek Hwang is an editorial board member of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Funding
None.
Data availability
Contact the corresponding author for data availability.
Acknowledgments
The authors would like to thank Myung Sun Hong, MD, a musculoskeletal radiologist with 20 years of experience working at Hallym University Chuncheon Sacred Heart Hospital, for performing the diagnostic ultrasound and magnetic resonance imaging interpretations.