Concomitant open distal clavicle excision is associated with greater improvement in range of motion without increased risk of acromial stress fracture after reverse total shoulder arthroplasty: a retrospective cohort study
Article information
Abstract
Background
The purpose of this study was to evaluate the effect of concomitant open distal clavicle excision (DCE) on postoperative clinical outcomes and incidence of acromial and scapular stress fractures (ASFs) in patients with symptomatic acromioclavicular joint osteoarthritis (ACJ OA) undergoing reverse total shoulder arthroplasty (RTSA).
Methods
A single-surgeon retrospective cohort study was conducted including patients who underwent primary elective RTSA with or without DCE from 2015 to 2019 with a minimum 6-month follow-up period. Shoulder active range of motion (AROM) and visual analog scale (VAS) pain were recorded preoperatively and postoperatively. ASFs and other adverse events were identified using postoperative notes and/or radiographs. Characteristics and outcomes were compared between the RTSA and RTSA-DCE groups.
Results
Forty-six RTSA patients (mean age, 67.9±8.7 years; 60.9% male; mean follow-up, 24.9±16.6 months) and 70 RTSA-DCE patients (mean age, 70.2±8.9 years; 20.0% male; mean follow-up, 22.7±12.9 months) were included. There were no significant intergroup differences in rates of ASF (RTSA, 0.0% vs. RTSA-DCE, 1.4%; P=1.00), stress reactions (RTSA, 8.7% vs. RTSA-DCE, 11.4%; P=0.76), reoperation, revision, or infection (all P>0.05), or in pre-to-postoperative reduction in VAS pain (P=0.17) at latest follow-up. However, the RTSA-DCE group had greater pre-to-postoperative improvement in flexion AROM (RTSA, 43.7°±38.5° vs. RTSA-DCE, 59.5°±33.4°; P=0.03) and internal rotation (IR) AROM (P=0.02) at latest follow-up.
Conclusions
Concomitant DCE in RTSA improves shoulder flexion and IR AROM, alleviates shoulder pain, and does not increase the risk of ASFs.
Level of evidence
III.
INTRODUCTION
Acromioclavicular joint (ACJ) osteoarthritis (OA) is common in patients with rotator cuff disorders, which accounts for a large proportion of patients undergoing reverse total shoulder arthroplasty (RTSA) [1,2]. Severe ACJ OA with ankylosis is a potential risk factor for acromial and scapular stress fractures (ASFs) after RTSA [3]. ACJ OA may increase the risk of ASFs after RTSA due to loss of motion through the ACJ and compensatory motion through the glenohumeral joint. This could, in turn, lead to increased compensatory deltoid muscle activity and increased stress at the acromion and scapular spine [3,4]. Even in the absence of ACJ OA, ASFs can occur after RTSA due to the increased demand placed on the deltoid as well as the presence of certain risk factors such as female sex, osteoporosis, and inflammatory arthritis [5-7].
Patients undergoing RTSA who have comorbid symptomatic ACJ OA may benefit from concomitant distal clavicle excision (DCE), which can relieve ACJ-related pain and improve shoulder function [8]. By reducing ACJ stiffness, concomitant DCE could restore scapulothoracic motion and reduce the risk of postoperative ASF. In the setting of RTSA, however, the coracoacromial (CA) ligament is frequently transected to assist in exposure, which may increase stress on the acromion and scapula and increase the risk of postoperative ASF [9, 10]. In CA ligament deficiency, DCE could further disrupt the scapular ring and theoretically predispose patients to greater scapular and acromial stresses and increased risk of ASF. There are few published data comparing outcomes between patients who underwent RTSA with DCE versus those who underwent RTSA alone, and the effect of concomitant DCE on clinical outcomes after RTSA is not well understood.
The purpose of this study was to evaluate the effect of concomitant open DCE on postoperative clinical outcomes and incidence of ASFs in patients with symptomatic ACJ OA undergoing RTSA. We hypothesized that there would be no differences in clinical outcomes or incidence of ASFs between patients undergoing RTSA with versus without DCE based on anecdotal evidence from the senior author (YWK)’s experience performing the concomitant DCE procedure without observing any increased incidence of ASFs or other adverse events.
METHODS
This study was conducted in compliance with the principles of the Declaration of Helsinki. The study’s protocol was reviewed and approved by the Institutional Review Board of New York University Langone Health (No. 21-01089). The requirement for informed consent was waived.
Study Design
A single-center, single-surgeon retrospective cohort study was conducted.
Eligibility Criteria and Cohort Selection
Patients who underwent primary RTSA with a shoulder and elbow fellowship-trained orthopedic surgeon (YWK) at a single urban academic medical center between February 1, 2015 and December 31, 2019 were identified using the senior author’s institutional database. Subjects were included in the cohort if they were ≥18 years of age at the time of surgery, underwent elective primary RTSA for the indication of cuff tear arthropathy, massive irreparable cuff tear, or primary glenohumeral OA (see “Diagnostic Criteria and Surgical Indications”), and had minimum follow-up of 6 months. This minimum follow-up time was based on prior studies of ASF incidence after RTSA with minimum 3-month follow-up but found that a significant number of ASFs took place between 3 and 6 months postoperatively [5,6,11]. Subjects were excluded from the cohort if they had a prior history of proximal humerus fracture and/or glenoid fracture, underwent revision RTSA, or underwent RTSA for the indication of proximal humerus fracture, glenoid fracture, rheumatoid arthritis, or avascular necrosis of the humeral head.
Diagnostic Criteria and Surgical Indications
The primary indications for RTSA among the study cohort were (1) symptomatic cuff tear arthropathy, (2) massive irreparable cuff tear associated with pain, pseudoparalysis, and/or range of motion (ROM) limitations, and (3) primary glenohumeral OA in patients ≥70 years old and/or with rotator cuff insufficiency identified intraoperatively. RTSA was preferred over other surgical interventions (e.g., anatomic TSA) in patients ≥70 years old with low functional demand, adequate glenoid bone stock, and intact deltoid muscle function. RTSA was contraindicated in patients with a non-functional deltoid.
Cuff tear arthropathy and massive cuff tears were diagnosed based on a combination of clinical and radiographic findings. Presenting symptoms included shoulder pain with motion, pain at night (particularly when sleeping on the affected shoulder), and/or reduced ROM. Physical exam findings included supraspinatus/infraspinatus atrophy and/or pseudoparalysis. Superior migration of the humeral head (defined as an acromiohumeral interval <7 mm) with or without acetabularization of the acromial undersurface on plain radiographs in the setting of a chronic rotator cuff tear was considered to be evidence of cuff tear arthropathy. Rotator cuff tears were identified on magnetic resonance imaging (MRI) and confirmed intraoperatively. Computed tomography (CT) imaging was not routinely obtained since all patients had MRI scans available, which were suitable for both prosthetic planning and identification of soft tissue pathology.
DCE was indicated in patients with symptomatic ACJ OA. The diagnosis of ACJ OA was made on the basis of findings on an anteroposterior radiograph of the shoulder (i.e., joint space narrowing, subchondral sclerosis and cysts, osteophyte formation) and on physical exam (i.e. focal tenderness to palpation over the ACJ, positive scarf test, positive resisted ACJ extension test, positive O’Brien’s test) and was confirmed intraoperatively. DCE was not performed in patients with radiographic evidence of ACJ OA without positive physical exam findings.
Operative Technique and Postoperative Rehabilitation
All RTSA procedures were performed using a deltopectoral approach without violating the CA ligament. The DJO Altivate Reverse Total Shoulder Prosthesis system (DJO Global) with a lateralized glenosphere and an inlay humeral stem was used for all cases. If the subscapularis was present, a subscapularis tenotomy was performed to achieve adequate exposure of the glenohumeral joint; the tendon was repaired at the end of the case.
All DCE procedures were performed after insertion of the prostheses. The CA ligament was resected, the distal clavicle and ACJ were identified in the superior portion of the wound, and approximately 10 mm of the distal clavicle was resected using a high-speed burr and small osteotomes. The CA ligament was preserved in all RTSA cases and was resected in all RTSA-DCE cases. Drains were used in all cases and removed on postoperative day 1.
Regardless of procedure (RTSA or RTSA-DCE), all patients followed the same postoperative protocol. Patients were immobilized in a sling for up to 4 weeks. Passive shoulder ROM exercises including forward flexion as tolerated in the plane of the scapula and external rotation (ER) to 20° past neutral and isometric deltoid strengthening exercises were started on postoperative day 1. Active-assisted and active ROM (AROM) exercises and isometric ER exercises were started at 4 to 6 weeks postoperatively.
Demographic and Preoperative Data
Demographic information was obtained via chart review and included age at time of surgery, sex, body mass index (BMI) at time of surgery, American Society of Anesthesiologists (ASA) physical status classification, and smoking history. Prior medical history was also obtained from chart review including primary indication for RTSA and history of diabetes mellitus, chronic kidney disease, rheumatological disease, and/or osteoporosis. Subjects reported their preoperative level of shoulder pain on a 10-point visual analog scale (VAS) with zero indicating no pain and 10 indicating the worst possible pain.
Radiographic Data
Severity of cuff tear arthropathy, glenohumeral OA, and ACJ OA were assessed on plain radiographs. Cuff tear arthropathy was graded using the Hamada classification system [12]. Glenohumeral OA and ACJ OA were graded using the Kellgren-Lawrence classification system [13].
Active ROM Measurement
Shoulder AROM for flexion, ER, and internal rotation (IR) were measured preoperatively and at latest follow-up. Flexion and ER AROM were measured in degrees (°). IR AROM was reported on an 8-point scale previously described by Flurin et al. [14] and Mollon et al. [15] based on the highest vertical distance that the subject could reach behind their back (e.g., hip, buttock, sacrum, vertebral level) during the physical exam (Table 1).
Outcomes Measured
The primary outcome measured was the incidence of ASFs. For the purposes of this study, ASFs were defined as ASFs visualized on plain radiographs in the presence or absence of associated symptoms (focal pain or tenderness to palpation over the acromion or scapular spine). Secondary outcomes included the incidence of other postoperative adverse events (acromial stress reactions, all-cause reoperations, all-cause revisions, non-infectious revisions, prosthetic joint infections), pre-to-postoperative change in VAS pain, and pre-to-postoperative change in flexion, ER, and IR AROM. Acromial stress reactions were defined as focal pain or tenderness to palpation over the acromion or scapular spine in the absence of radiographic changes [6]. Reoperations were defined as any subsequent surgery involving the index shoulder while revisions were defined as any subsequent procedure involving replacement of one or more components of the original prosthesis. All secondary outcomes were abstracted from postoperative notes, radiographs, and MRI scans.
Statistical Analysis
All statistical analyses were performed in SAS Studio ver. 9.4 (SAS Institute). All continuous variables were assessed for normality using the Shapiro-Wilk test. Normally distributed continuous variables were compared between groups using Student t-test. Non-normally distributed continuous variables were compared between groups using the Mann-Whitney U-test. Pre-to-postoperative change in VAS pain and AROM was evaluated using the paired t-test or Wilcoxon signed-rank test, as appropriate. Categorical variables were compared between groups using Fisher’s exact test. Multivariable linear and logistic regression were used to identify predictors of continuous and binary outcomes, respectively. Each regression model included the following predictors: DCE, procedure indication, age, sex, BMI, smoking history, comorbidities, glenohumeral OA grade, and ACJ OA grade. Subgroup analyses were performed for subjects with CTA (with Hamada classification included as a co-predictor) and for subjects with primary glenohumeral OA. Linear regression results were reported as beta (β) coefficients with 95% confidence intervals (CIs) and logistic regression results were reported as odds ratios (ORs) with 95% CIs. All P-values <0.05 were considered significant.
RESULTS
Demographic and Clinical Characteristics
Three hundred twenty-six patients were screened for inclusion in the study, of whom 116 met eligibility criteria (Fig. 1). Of the 116 included subjects, 46 underwent RTSA without DCE and 70 underwent RTSA with DCE. Demographic and clinical characteristics were compared between groups (Table 2). The RTSA cohort had a mean age of 67.9±8.7 years (range, 43–87 years) and the RTSA-DCE cohort had a mean age of 70.2±8.9 years (range, 51–95 years). Pluralities of patients in both groups underwent RTSA for treatment of cuff tear arthropathy (RTSA, 56.5%, RTSA-DCE, 47.1%), but a significantly higher proportion of RTSA-DCE patients underwent surgery for treatment of primary glenohumeral OA (RTSA, 21.7% vs. RTSA-DCE, 44.3%; P<0.001). The RTSA group had a significantly lower proportion of never smokers (P=0.02) and a significantly lower proportion of patients indicated for RTSA due to primary glenohumeral OA (P=0.02), but age, BMI, ASA classification, glenohumeral OA grade, ACJ OA grade, incidence of comorbidities, and follow-up time did not significantly differ between the two groups (all P>0.05).
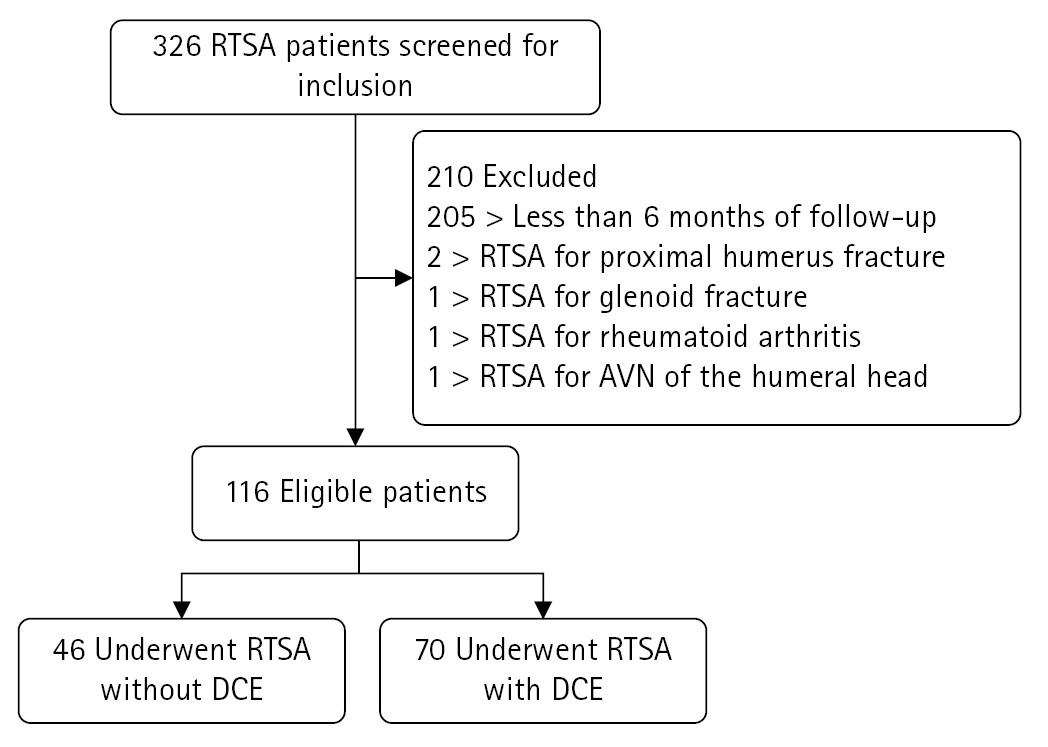
Patient flowchart. RTSA: reverse total shoulder arthroplasty, AVN: avascular necrosis, DCE: distal clavicle excision.
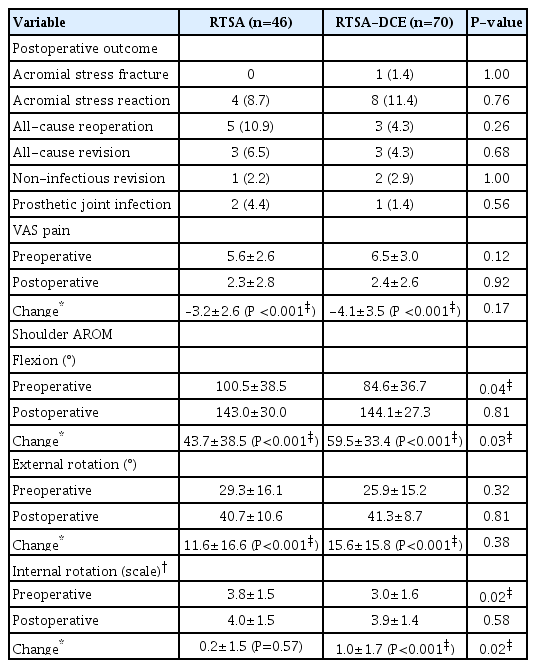
Postoperative Outcomes and AROM
Postoperative outcomes and shoulder AROM were compared between the RTSA and RTSA-DCE groups (Table 3). No ASFs occurred in the RTSA group by latest follow-up. Only one ASF occurred in the RTSA-DCE group by latest follow-up; this patient was a 65-year-old female with prior history of chronic kidney disease and osteoporosis who underwent RTSA for a primary indication of glenohumeral OA. The most common postoperative adverse events were acromial stress reactions (RTSA, 8.7%; RTSA-DCE, 11.4%) and all-cause reoperations (RTSA, 10.9%; RTSA-DCE, 4.3%). There were no significant inter-group differences in the incidence of acromial stress reactions, all-cause reoperations, all-cause revisions, non-infectious revisions, or prosthetic joint infections (all P>0.05). Both groups experienced significant pre-to-postoperative reduction in VAS pain (both P<0.001), but the magnitude of this reduction was not significantly different between the two groups (P=0.17).
Prior to surgery, the RTSA group had significantly higher flexion AROM (P=0.04) and IR AROM (P=0.04) but not ER AROM (P=0.32). Both groups experienced significant pre-to-postoperative improvement in flexion AROM and ER AROM (all P<0.001), but only the RTSA-DCE group experienced significant improvement in IR AROM (P<0.001). Improvement in flexion AROM and IR AROM was significantly higher in the RTSA-DCE group (all P<0.05), but there was no significant inter-group difference in ER AROM improvement (P=0.38).
Predictors of Postoperative Outcomes
Significant predictors of postoperative outcomes and shoulder AROM were identified (Table 4). Among all subjects, DCE was not significantly predictive of the odds of ASF, acromial stress reaction, or any other postoperative adverse event (all P>0.05). However, DCE was predictive of greater pre-to-postoperative improvement in flexion AROM (P=0.006) and IR AROM (P=0.04). Higher BMI was associated with increased odds of all-cause reoperation (P=0.03) and all-cause revision (P=0.04). Primary indication of glenohumeral OA was predictive with lower odds of acromial stress reaction (P=0.049) and greater improvement in ER AROM (P=0.01) and IR AROM (P=0.03) compared to primary indication of cuff tear arthropathy. Conversely, primary indication of massive irreparable rotator cuff tear was associated with reduced improvement in ER AROM (P=0.04) compared to primary indication of cuff tear arthropathy.
Subgroup Analysis by Procedure Indication
When subgrouping the cohort by procedure indication (Table 4), DCE was found to be predictive of greater improvement in IR AROM (P=0.04) among patients with cuff tear arthropathy and greater improvement in both flexion AROM (P=0.03) and IR AROM (P=0.03) among patients with primary glenohumeral OA. In addition, current smoker status (vs. never smoker status) was predictive of reduced improvement in ER AROM (P=0.03) among patients with cuff tear arthropathy and reduced improvement in both flexion AROM (P=0.03) and ER AROM (P=0.02) among patients with primary glenohumeral OA.
DISCUSSION
Main Findings
The most important finding of this study was that RTSA with concomitant DCE was not associated with higher odds of postoperative ASF compared to RTSA without DCE, thus supporting the hypothesis of the study. Moreover, DCE was not associated with the odds of any other postoperative adverse events including acromial stress reactions, all-cause reoperations, all-cause revisions, non-infectious revisions, or PJIs. In contrast, DCE was associated with greater pre-to-postoperative improvement in both flexion AROM and IR AROM. In addition, DCE was predictive of greater improvement in flexion AROM and IR AROM among RTSA patients with primary glenohumeral OA and greater improvement in IR AROM among RTSA patients with cuff tear arthropathy. DCE was not found to be predictive of pre-to-postoperative improvement in VAS shoulder pain.
Concomitant DCE and Acromial Stress Fracture Risk
Prior retrospective studies involving large cohorts of RTSA patients identified risk factors for postoperative ASF including older age, female sex, osteoporosis, and inflammatory arthritis, but none to date assessed whether concomitant DCE is a predictive factor for risk of ASF [6,7]. Likewise, while open DCE has been associated with common complications such as wound disruption, hematoma, and surgical site infection, neither isolated procedures nor concomitant procedures with RTSA were associated with increased rates of ASF in prior retrospective analyses [16,17]. In contrast, in a retrospective case-control study of 11 primary RTSA patients with postoperative ASFs matched to 44 controls, Townsend et al. [3] noted that 20% of the control group had radiographic evidence of a prior DCE or ACJ coplaning procedure, whereas no patients in the ASF group had undergone prior ACJ surgeries. Though Townsend et al. [3] did not find the difference in ACJ procedure rates to be statistically significant, they did hypothesize that DCE was a protective factor against ASF following RTSA. The lone patient in the present study who experienced a postoperative ASF had undergone RTSA with concomitant DCE, but also had known risk factors for ASF including older age, female sex, and history of osteoporosis. As such, the results of the present study do not suggest that concomitant DCE is a predictive factor for the risk of ASF following RTSA. This finding has two major caveats in that (1) only one patient in the entire cohort experienced an ASF by latest follow-up and (2) this study did not include a comparison group of patients with symptomatic ACJ OA who underwent RTSA without DCE.
Concomitant DCE and Shoulder ROM
The impact of DCE on shoulder ROM has been studied primarily in the setting of concomitant rotator cuff repair (RCR) as opposed to RTSA, and the highest-quality evidence available suggests that DCE does not have a significant effect on postoperative ROM. Wang et al. [18] conducted a meta-analysis of three randomized controlled trials involving 208 patients (91 RCR-DCE, 117 RCR) and found no significant difference in flexion, IR, or ER ROM between the two groups at minimum 2-year follow-up. Similarly, in one of the few studies conducted in the RTSA population, Cirigliano et al. [17] performed a retrospective matched-cohort analysis of 39 RTSA-DCE patients matched to 39 RTSA patients and found no significant differences in postoperative flexion, abduction, ER, or IR ROM between the two groups at minimum 2-year follow-up. In addition, while both groups experienced significant pre-to-postoperative improvement in flexion and abduction ROM and no significant change in IR ROM, the RTSA-DCE group experienced a significant decrease in ER ROM whereas the RTSA group did not. Thus, the prior evidence up to this point has not found concomitant DCE to have a significant positive impact on postoperative shoulder ROM.
In contrast to the Cirigliano et al.’s study [17], in the present study we found RTSA-DCE to be associated with significant pre-to-postoperative improvement in ER ROM as well as flexion and IR ROM, and furthermore, the improvements in flexion and IR ROM were significantly greater than those of the RTSA group. RTSA-DCE patients had significantly lower preoperative flexion and IR ROM compared to their RTSA counterparts, which suggests that RTSA patients with clinically symptomatic ACJ OA may have inferior baseline shoulder ROM compared to RTSA patients without symptomatic ACJ OA. This may be due to the effect of ACJ ankylosis leading to reduced scapulothoracic motion and, indirectly, glenohumeral joint motion [4]. The effect of ACJ OA on glenohumeral motion may only reach significance in glenohumeral joint OA, where there may be greater compensatory motion across the ACJ. RTSA-DCE patients achieved an average increase of 59.5° in shoulder flexion by latest follow-up compared to an average increase of 40.7° among the RTSA group. This inter-group difference in flexion ROM improvement (18.8°) represents a clinically significant difference based on the prior reported minimum clinically important difference of 12° for shoulder flexion after total shoulder arthroplasty [19].
These findings were further reinforced by the multivariate analysis, which found concomitant DCE to be a significant predictor of greater improvements in both flexion and IR ROM even when controlling for differences in demographic and clinical characteristics. The results of the present study suggest that DCE provide additive benefits in terms of improved shoulder ROM when performed for the treatment symptomatic ACJ OA in the setting of RTSA. While there is a subset of patients who may have ACJ pain without significant arthritis, no recommendations can be made regarding whether DCE has the potential to help isolated ACJ pain without arthritis.
Clinical Considerations
Based on the results of the present study, it is unclear whether concomitant DCE is specifically indicated in patients with symptomatic ACJ OA undergoing RTSA in order to reduce the risk of postoperative ASF. Nonetheless, the results of the present study suggest that RTSA with concomitant DCE alleviates shoulder pain and improves shoulder ROM among patients with symptomatic ACJ OA comorbid with other shoulder pathologies (cuff tear arthropathy, massive irreparable rotator cuff tear, primary glenohumeral OA), and may be indicated for these purposes. It is important to note that only symptomatic ACJ OA was treated with DCE in this study. Routine DCE is not recommended for asymptomatic radiographic ACJ OA given that prior randomized controlled trials have found no significant difference in postoperative pain or ROM between patients who underwent RCR with versus without DCE for the treatment of rotator cuff tears with radiographic ACJ OA [18,20].
Limitations
The present study has several limitations. First, this study was retrospective in nature and had short-term follow-up with minimum and mean follow-ups of 6 and 19 months, respectively. Second, the study was conducted as a single surgeon series with a single implant type in a single patient population in the United States, which improves the comparability of the RTSA-DCE and RTSA groups within this study but decreases its generalizability to other RTSA populations. This is particularly important to consider when applying the results of the present study to non-U.S. populations in which BMI is lower and/or osteoporosis is more prevalent. Third, as mentioned previously, there was no control group of patients with symptomatic ACJ OA who were treated with RTSA without concomitant DCE. Since there may have been other clinical differences between patients with and without symptomatic ACJ OA undergoing RTSA, it cannot be definitively concluded that the addition of DCE improves pain and shoulder ROM independent of the RTSA procedure itself. Fourth, preoperative glenoid retroversion was not measured and reported since many patients did not have CT and/or MRI scans that were accessible from the study institution’s electronic medical record system. Fifth, preoperative bone densitometry scores could not be obtained for the majority of patients in either cohort, and the present study cannot account for the effect of baseline bone density on ASF risk.
CONCLUSIONS
Concomitant DCE in RTSA improves shoulder flexion and IR AROM, alleviates shoulder pain, and does not increase the risk of acromial stress fractures.
Notes
Author contributions
Conceptualization: ACK, MSV, YWK. Data curation: DSS, NG, MGA. Formal Analysis: ACK, DSS, YWK. Investigation: ACK, DSS, NG, MRB, MB, MGA, YWK. Methodology: ACK, MSV, YWK. Project administration: MSV. Software: DSS. Supervision: ACK, MB, YWK. Visualization: DSS. Writing – original draft: ACK, DSS, NG, MRB, MB, YWK. Writing – review & editing: ACK, DSS, MB, MGA, MSV, YWK.
Conflict of interest
None.
Funding
None.
Data availability
Contact the corresponding author for data availability.
Acknowledgments
None.