Prevalence of rotator cuff diseases in adults older than 40 years in or near Chuncheon city, Korea
Article information
Abstract
Background
To determine the prevalence of rotator cuff diseases in a population older than 40 years in or nearby Chuncheon city, Republic of Korea.
Methods
Sixty shoulders of 30 people older than 40 years who participated in a health lecture were examined for free by an orthopedic surgeon. Visual analog scale of pain and American Shoulder and Elbow Surgeons scores were assigned, and routine physical examination was performed. Ultrasonography was performed on the shoulder.
Results
On ultrasonographic examination, there were one shoulder with full thickness rotator cuff tear, 20 of 60 (33%) with partial thickness rotator cuff tear, five of 60 (8%) with calcific tendinitis, one of 60 (2%) with tear of the long head of the biceps, and five of 60 (8%) with tendinitis of the long head of the biceps. Participants older than 60 years showed significantly high proportions of lesion of the long head of the biceps and rotator cuff diseases (P=0.019 and P=0.015, respectively). Participants who performed physical labor had high proportions of rotator cuff tear and rotator cuff disease (P=0.001 and P<0.001, respectively).
Conclusions
Rotator cuff diseases showed a high prevalence in aged persons and resulted in a decrease in shoulder function.
INTRODUCTION
Shoulder pain is the third most common musculoskeletal pain and is estimated to compose 16% of all cases of musculoskeletal pain in primary medical care [1,2]. There are 15 musculoskeletal pain cases per 1,000 primary medical care cases each year, totaling about 1% of all adults receiving primary medical care annually [1,2]. Patients who experience shoulder pain for more than 1 year compose 60% of all shoulder pain patients; if not treated, these patients will experience severe disabilities, poor quality of life, and loss of occupation [1,2].
Shoulder pain is defined as chronic when it has been present for more than 6 months, regardless of any treatment the patient has previously received. The most common medical cause of chronic shoulder pain is rotator cuff disease, which includes tendinosis of the rotator cuff or long head of the biceps, partial- or deep-thickness tear of the long head of the biceps tendon, and calcific tendinitis. Other medical causes of chronic shoulder pain include adhesive capsulitis, osteoarthritis of the arm and shoulder joints, instability of the arm and shoulder joints, and acromioclavicular joint disease [1].
Despite active studies that have been conducted overseas on the treatment and prevalence of shoulder pain [1-5], studies on the prevalence of shoulder pain and that of rotator cuff diseases that cause shoulder pain in Korea remain limited [6]. Accordingly, we examined 60 shoulder cases of 30 adults older than 40 years of age living in Chuncheon city, Korea and nearby areas to determine the prevalence of rotator cuff diseases that cause shoulder pain in this population.
METHODS
Materials
We conducted this study in compliance with the principles of the Declaration of Helsinki. The study’s protocol was reviewed and approved by the Institutional Review Board of Chuncheon Sacred Heart Hospital (IRB No. 2020-04-011-003), and the need for informed consent was waived.
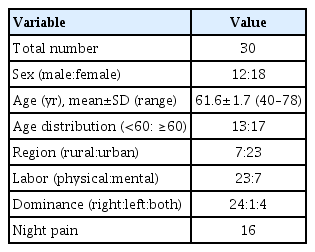
A total of 60 shoulder cases of 30 people over 40 years of age who participated in a health lecture held at the university hospital was included. The average age of study participants was 61.6±1.7 years (range, 40–78 years). Twelve patients were male and 18 were female. Seven patients resided in rural areas, while 23 resided in urban areas. Twenty-three were manual workers and seven were office workers. Sixteen complained of night pain (Table 1).
Method
For functional assessment of shoulder joints, the American Shoulder and Elbow Surgeons (ASES) scoring system established by the American Shoulder and Elbow Society in 1994 was deployed, and a physical examination was performed. Among 57 participants in the health lecture, 30 underwent ultrasound tests for both shoulder joints performed by an orthopedic specialist with 5 years of experience who focused on treating shoulder and elbow joints. Additionally, the 30 study participants also underwent score assessment and physical examination performed by two orthopedic nurses with 7 years of experience.
Participants who reported pain during the examination for presence of shoulder joint pain were asked further about the presence and extent of night pains, medical history of analgesics, and location of pain. A visual analog scale (VAS) was used to score the severity of pain, ranging from 0 points for no pain to 10 points for the most severe pain. Ultrasound tests have been used to identify tendinitis or tear of the long head of the biceps tendon, partial- or full-thickness tears of the rotator cuff, and rotator cuff diseases including calcific tendinitis.
Diagnosis of full-thickness tear of the rotator cuff was performed in accordance with the criteria as follows (Fig. 1) [7]: (1) the supraspinatus is not visible due to retraction of torn supraspinatus below the acromioclavicular joint; (2) loss or discontinuity in the local rotator cuff muscle accompanied by continual loss of normal anterior arch in the subdeltoid bursa; (3) loss of normal supraspinatus muscle parenchyma accompanied by increased distance between the supraspinatus and long head of the biceps tendon and exposure of the bare area of the bone and cartilage; (4) hypoechoic or anechoic extension observed through the full parenchyma of the rotator cuff; (5) fluid in the subacromial and subdeltoid bursa with or without fluid in the sheath of the long head of the biceps tendon.

Sonographic finding of the full-thickness rotator cuff tear. The arrow indicates the full-thickness rotator cuff tear.
Partial-thickness tear of the rotator cuff was diagnosed by a local hypoechoic or anechoic defect of the bursa or a joint near the rotator cuff in two perpendicular planes (Fig. 2) [8]. Calcification of the rotator cuff appears as a hyperechoic lesion on ultrasound imaging (Fig. 3). Depending on the amount and stage of calcification, the type of lesion can appear clear with acoustic shadowing or could be blurry or a type with no shadowing [9,10].

Sonographic finding of the partial-thickness rotator cuff tear. The arrow indicates the partial-thickness rotator cuff tear.

Sonographic finding of calcific tendinitis of the rotator cuff. The arrow indicates a calcific deposit of the rotator cuff. The asterisk indicates acoustic shadowing.
In the transverse sonographic view, tenosynovitis of the long head of the biceps tendon appears like a fried egg due to a halo effect of hypoechoic effusion near the dense shadow of the long head of the biceps tendon (Fig. 4) [11]. A partial-thickness tear could appear as a crevice (Fig. 5), while a full-thickness tear may not be visible because of an involution. Rupture is often accompanied by medial dislocation of the long head of the biceps tendon [12].

Sonographic finding of long head of the biceps tendinitis. The arrow indicates the long head of the biceps tendon. The asterisk indicates effusion surrounding the long head of the biceps tendon. The shape is similar to that of a fried egg.
Statistical Analysis
The Mann-Whitney U-test was used to compare the measured mean values, and a statistical analysis was performed using the SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA), with statistical significance established at P<0.05.
RESULTS
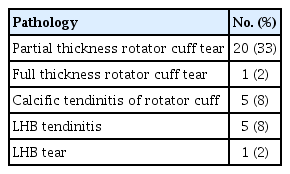
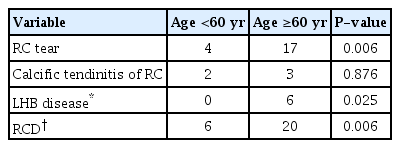
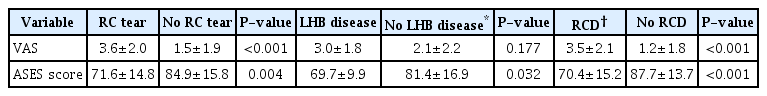
Of the 60 shoulder cases, 39 were painful, with 15 experiencing moderate degree of pain with a VAS score of 4 points or higher. The average VAS and ASES scores were 2.2±0.3 (0–8) points and 80.2±2.1 (35–100) points, respectively. During ultrasound examination, one shoulder showed a full-thickness rotator cuff tear, 20 of 60 (33%) showed a partial-thickness rotator cuff tear, five of 60 (8%) presented with calcific tendinitis, one of 60 (2%) demonstrated a tear of the long head of the biceps tendon, and five of 60 (8%) presented tendinitis of the long head of the biceps tendon (Table 2). Of the participants aged 60 years or older, the rate of rotator cuff rupture, long head of the biceps tendon lesion, and rotator diseases was significantly higher (P=0.006, P=0.025, and P=0.006, respectively) than those of younger participants (Table 3). Significantly high rates among manual workers were found regarding rotator cuff rupture and rotator cuff disease (P=0.002 and P<0.001, respectively). Meanwhile, significantly low ASES scores were observed among manual workers’ shoulders (P=0.025) (Table 4). In addition, VAS and ASES scores were significantly lower in shoulders presenting rotator cuff rupture (P<0.001 and P=0.004). Lower ASES scores were noted in shoulders with long head of the biceps tendon lesion (P=0.032). The VAS and ASES scores were significantly lower among those with rotator cuff disease relative to those without rotator cuff disease (P<0.001 and P<0.001) (Table 5).
DISCUSSION
The majority of patients in Korea who experience shoulder pain postpone visiting the hospital until no effect is achieved with a variety of conservative treatments such as physical therapy or acupuncture or significant dysfunction or severe pain is experienced. Because of this, it is difficult to identify and treat the cause of the pain early [6]. In this research, among 60 shoulder cases, 39 (65%) were painful and 15 (25%) experienced a moderate degree of pain with a VAS score of four points or higher. There is a difference in the distribution of causal diseases of shoulder pain by age. In patients younger than 40 years, shoulder instability or mild rotator cuff disease (i.e., impingement syndrome or tendinosis) is the most common cause, while, in patients older than 40 years of age, risk of developed chronic rotator cuff disease (partial or deep tear), adhesive arthritis, or glenohumeral osteoarthritis increases [1,2,13].
Manual occupations and leisure activities show correlations with shoulder pain. Sports with frequent collisions or activities like lifting of heavy materials can trigger shoulder instability or osteoarthritis in acromioclavicular joints, and upward movement of arms in activities or sports may result in a morbid condition of the rotator cuff [1,13]. This research reported significantly higher rates of rotator cuff rupture and rotator cuff disease in manual workers compared to office workers (P=0.002 and P<0.001, respectively).
Previous treatments that aggravate or alleviate pain or causative factors could be clues in attempting to diagnose rotator cuff disease. Night pain that comes on after sleeping on the injured shoulder or a trauma history may be related to rupture of the rotator cuff. A painful arc induced by lifting activities involving the arm is not only related to rotator cuff rupture, but also to tendinosis. Past history of shoulder surgery is important because of early and late complications that may appear such as adhesive arthritis and glenohumeral osteoarthritis [1,13].
Hermans et al. [14] reported that the incidence of rotator cuff disease including tendinosis and rupture was 33% to 81% in their five studies performed using magnetic resonance imaging or ultrasound. In addition, Tashjian [15] observed deep-thickness rotator tear at a rate of 25% among those in their 60s and at a rate of 80% among those in their 80s using magnetic resonance imaging or ultrasound. In this study, there was one patient (1/60, 2%) with a full-thickness rotator cuff tear; 20 patients (20/60, 33%) with partial-thickness rotator cuff tear; and a significantly high ratio of rotator cuff rupture, long head of the biceps tendon lesions, and rotator cuff disease in those aged 60 years and older (P=0.006, P=0.025, P=0.006, respectively).
Oliva et al. [16] reported the prevalence of calcific tendinitis of the rotator cuff as 2.7% to 22% and that it was especially prevalent in women aged 30 to 35 years. In this research, five of 60 (8%) cases of calcific tendinitis were observed. Murthi et al. [17] reported that, of more than 200 shoulders that underwent arthroscopic subacromial decompression surgery for impingement syndrome, 80 (40%) showed degenerative change of the long head of the biceps tendon. Beall et al. [18] reported that, among 111 patients who underwent arthroscopic or open surgery for shoulder pain, 23 (23%) showed partial- or deep-thickness rupture of the long head of the biceps tendon. In this research, five patients (5/60; 8%) showed tendinitis of the long head of the biceps tendon, and one patient (1/60, 2%) showed a tear of the long head of the biceps lesion.
Rotator cuff diseases of the shoulder appear with a high prevalence in elderly people and result in a decrease in shoulder function. Also, manual laborers more often experience rotator cuff disease than do office workers. Therefore, exploring more preventive and therapeutic considerations is thought to be appropriate in particular for old-aged manual laborers.
Acknowledgements
We would like to express sincere gratitude to two clinical research nurses, Byeong-Yi Choi and Ok-Hwa Park, for helping with measurement of participant visual analog scale and American Shoulder and Elbow Surgeons scores and with the ultrasound tests. We also am grateful to specialist Byung-Chan Kwak, who helped with data organization.
Notes
Financial support
None.
Conflict of interest
None.