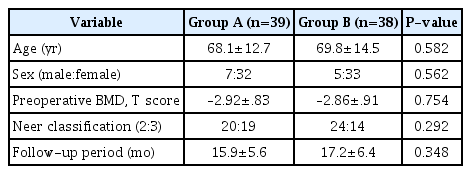
Comparison between MIPO and the deltopectoral approach with allogenous fibular bone graft in proximal humeral fractures
Article information
Abstract
Background
The purpose of this study was to investigate the clinical differences between open reduction and plate fixation via a deltopectoral approach with allogenous fibular bone graft and a minimally invasive plate osteosynthesis (MIPO), in Neer's classification two-, three- part proximal humeral fractures.
Methods
In this retrospective study, 77 patients with two-, three-part proximal humeral fractures were treated at two different institutions. Clinical and radiological evaluations were performed in 39 patients, who underwent MIPO at one institution (group A), and 38 patients, who underwent a deltopectoral approach with allo-fibular bone graft (group B) at another institution. The results between the groups were compared.
Results
The MIPO technique was significantly less time consuming and caused less bleeding than the deltopectoral approach with allo-fibular bone graft (P<0.05). The duration of the fracture union was significantly reduced in group A (14.5±3.4; range, 10–22 weeks) compared to group B (16.4±4.3; range, 12–28) weeks (P<0.05). There were no statistically significant differences between the two groups when evaluating the visual analog scale and Constant scores between the two groups, 1 year postoperatively. In radiological evaluation, there was no difference in radiological outcomes between the two groups. There were no statistically significant differences in malunion between the two groups.
Conclusions
The MIPO technique and deltopectoral approach with allo-fibular bone graft for two-, three-part proximal humeral fractures, show similar clinical and radiological results. However, allogenous fibular grafts require longer surgery, cause more bleeding, and result in longer fracture healing time than MIPO technique.
INTRODUCTION
Proximal humeral fractures are relatively common fractures, accounting for about 5% of all fractures and are more frequent in older osteoporosis patients [1]. In most cases without severe displacement, good outcomes can be achieved through non-surgical treatment [2]. However, in cases in which bone fragments have large displacement or angulation, surgical treatment is required to restore normal shoulder function [3]. Surgical treatment methods include plate fixation, intramedullary nailing, and replacement arthroplasty; however, internal fixation with a locking plate is the most commonly used treatment method [4]. Patients with severe comminuted fractures or osteoporosis are more likely to develop complications such as fixation failure, interposition, and angulation during normal plate fixation. These complications often lead to poor clinical outcomes. Recently, allogenous fibular bone graft with relatively high bone strength and similar size to the inner diameter of the proximal humerus has been used to prevent these problems. Furthermore, recent studies have shown that in cases of severe comminuted fractures, superior clinical results were achieved using the graft method [5-7].
The deltopectoral approach was previously used for plate fixation in proximal humeral fractures. However, this approach requires a large incision range and considerable dissection of the soft tissue to secure the field of view of the lateral part of the humerus [8]. In order to address these drawbacks, plate fixation with MIPO can shorten the surgery time and minimize bleeding and soft tissue injury, leading to superior fracture healing compared to the conventional deltopectoral approach [8,9]. In some studies, fixation with MIPO has demonstrated superior clinical outcomes compared to open reduction [8,10]. However, due to the limited visibility during surgery, especially in Neer classification three-, four-part with severe displacement, skillful operation is required for proper reduction. Due to the limited approach, performance of bone grafts including allogenous fibular bone grafts is difficult, especially when there is no greater tuberosity fracture or the extent of displacement is not severe [11].
Both allogenous fibular bone graft and MIPO have been introduced to minimize the problems of fixation failure, displacement, angulation, and nonunion after plate fixation of proximal humeral fractures. However, there have been no studies investigating the differences between the clinical results of these two treatment methods. The aim of this study was to investigate the clinical differences between plate fixation via the deltopectoral approach with allogenous fibular bone graft and MIPO without bone graft in proximal humeral fractures.
METHODS
This study was approved by the Institutional Review Board of National Health Insurance Service Ilsan Hospital (IRB No. 2017-04-036).
Patient Selection
This study is a retrospective analysis of the medical records of patients diagnosed with proximal humeral fractures who underwent internal fixation with locking plates by the same shoulder surgeon with similar clinical experiences in two different medical institutions from January 2014 to December 2016. Patients over 19 years old with two-, three-part proximal humeral fracture who underwent surgical treatment were included. Patients under 19 years of age, with associated clavicle or scapula fractures, neurological injuries such as brachial plexus injury, periprosthetic fracture, and those without at least 1 year of follow-up were excluded from the study. One surgeon performed locking plate fixation using MIPO in all patients with Neer classification two-, three-part fractures except for cases of greater tuberosity fractures alone. The other surgeon at another institution performed locking plate fixation and allogenous fibular bone graft via the deltopectoral approach in all two-, three-part fracture patients. Cases of four-part fractures were excluded from the analysis because MIPO was not performed in any. A total of 77 patients met the inclusion criteria. Clinical and radiological results were analyzed and compared for 39 patients who underwent MIPO (group A) and 38 patients who underwent allogenous fibular bone graft (group B).
Operative Technique
All patients underwent surgery in the beach chair position and the surgery was performed using image amplification equipment (C-arm) monitoring the status of reduction. Surgeries for both groups utilized the same locking plate type (PHILOS; Synthes, Paoli, PA, USA).
For MIPO, a 3-cm skin incision was made from the anterolateral side of the acromion to the distal part. The anterior raphe of the deltoid was detached and a finger was placed to feel the axillary nerve under the deltoid of the distal incision line. This was lifted to protect the nerve. Under the deltoid on the lateral side of the periosteum, blunt dissection was performed to create space to insert the plate. Greater tuberosity fracture with displacement cases were reduced while monitoring with image amplification equipment and fixed with two Kirschner wires. Upon securing enough space to place the plate under the deltoid and along the humeral surface, the axillary nerve was lifted and protected using a finger and the plate was inserted into the space. While monitoring using image amplification equipment, the plate was placed at an estimated height of 5 mm distal to the greater tuberosity. With an oblong-shaped hole in the distal plate as a reference, an approximate 3-cm incision was made in the distal part. Intramuscular dissection was performed to expose the distal plate. For indirect reduction, a pin was inserted into the anterior humeral head, and the reduction was performed using the joystick method. Alternatively, a conventional screw was inserted in the oblong-shaped hole in the distal plate for indirect humeral head reduction. After investigating the state of reduction with the image amplification equipment, the humeral head was fixed by six locking screws from the proximal plate to the third row. The arm was used to secure adequate visualization of the distal plate, and the remaining locking screws were inserted to complete the procedure. Since the medial inferior screws of the fourth row of the plate were placed near the axillary nerve, these were not inserted in all patients (Fig. 1).
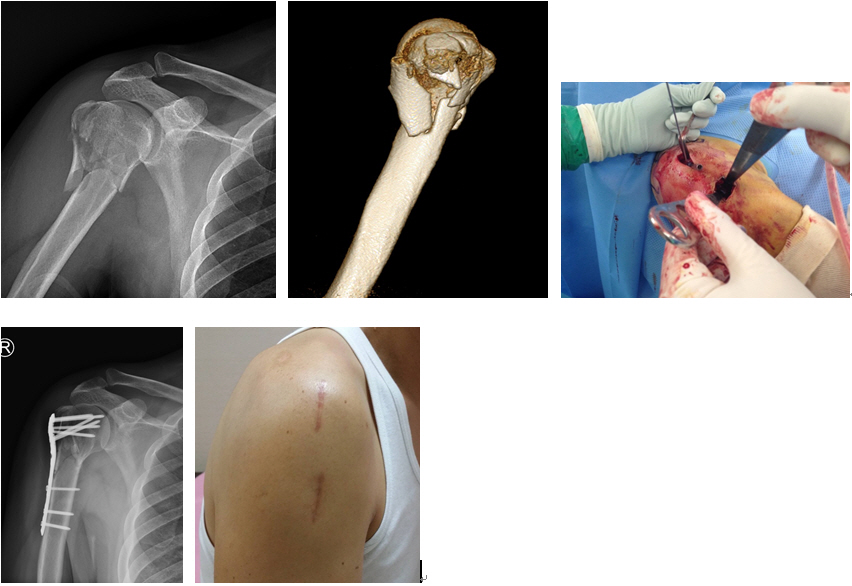
A 50-year old man with comminuted proximal humeral fracture who was treated with minimally invasive plate osteosynthesis technique. (A) Preoperative anteroposterior radiography. (B) Preoperative three-dimensional computed tomography scan. (C) Intraoperative gross photo. (D) Postoperative anteroposterior radiography. (E) Final scar from surgery.
In the allogenous fibular bone graft group, the deltopectoral approach was performed in all patients. Commencing at the coracoid process end, an ~10 cm incision was made in the lateral inferior direction toward the deltoid attachment. The subcutaneous tissue was dissected with the cephalic vein placed to the lateral side, and a blunt dissection was performed between the deltoid and the pectoralis major muscle. The fractured proximal humerus was exposed by dissection of the attachment site under the deltoid and removal of the bursa tissue. After the allogenous fibula bone was trimmed to enter the humerus inner diameter, the fracture site was opened to secure a space. The allogenous fibula bone was inserted while monitoring with the image amplification equipment, resulting in indirect reduction of the humerus fracture site by allogenous fibula bone. In cases with greater tuberosity fractures, a few threads were passed through the supraspinatus tendon and infraspinatus tendon, applying traction to the fragments for reduction; temporary fixation was performed using K-wires. Complete reduction state of the fracture site was confirmed with the image amplification equipment, and the plate was secured by fixing the screw to complete the surgery (Fig. 2).
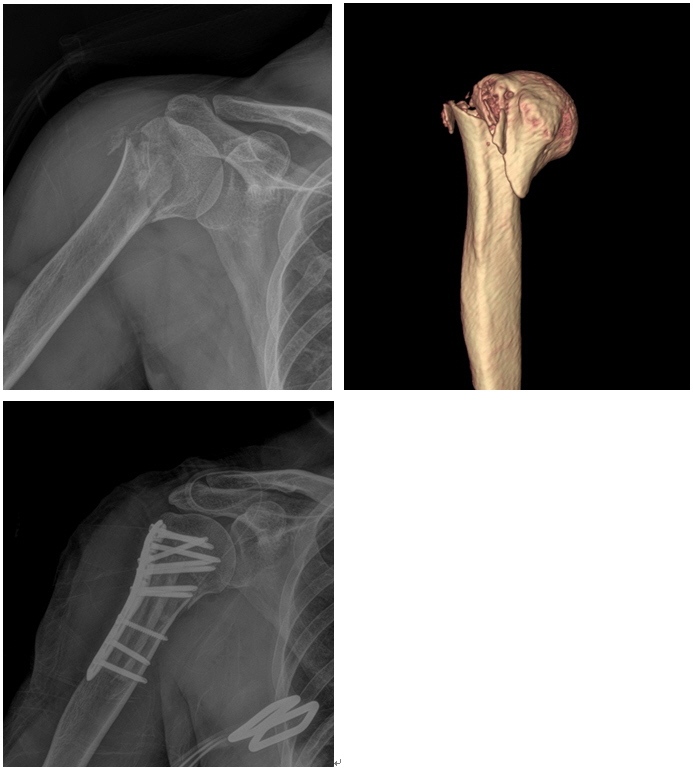
A 64-year-old man with Neer classification two-part proximal humeral fracture who was treated with open plating with allogenous fibular bone graft. (A) Preoperative anteroposterior radiography. (B) Preoperative three-dimensional computed tomography scan. (C) Postoperative anteroposterior radiography.
All patients were immobilized for 3 to 6 weeks using a sling after surgery. After pain was mitigated, the patients began passive exercise and assisted active exercise on a set schedule. Muscle strength exercise was performed after fracture union.
Clinical and Radiological Assessments
For clinical evaluation, the amount of bleeding during surgery was measured by referring to the medical record prepared by the anesthesiologist, and the surgery time was defined as the time from the first skin incision to completed suture. The visual analog scale (VAS) and Constant score were measured 1 year after surgery for functional evaluation. After the surgery, all patients were treated as outpatients, visiting the hospital on a regular basis. The anterior-posterior (AP) X-ray and axillary X-ray images were examined to determine the reduction and maintenance status of the fracture site, the extent of fracture healing, and the occurrence of complications such as the avascular necrosis of the humeral head. Fracture union was defined as the presence of at least three bridging calluses observed in the AP and axillary X-ray images. For radiological evaluation, neck-shaft angle was measured on the final follow-up AP images (Fig. 3A) [12]. Malunion was defined as a neck-shaft angle less than 120° on postoperative radiographs during the follow-up period [11]. Plate height was measured as the distance from the lateral end of the humeral greater tuberosity to the upper end of the plate in the final follow-up AP image (Fig. 3B).
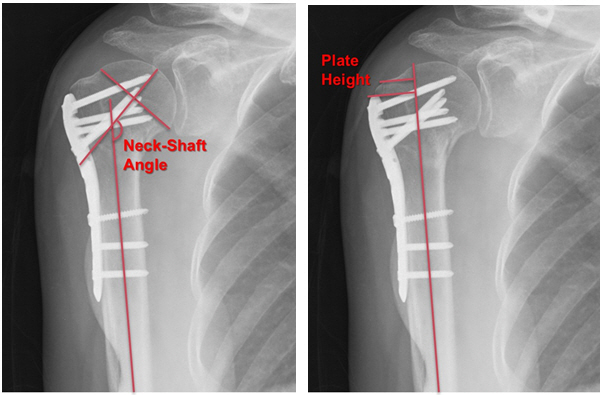
Radiographic evaluation at last follow-up. (A) Neck-shaft angle: angle between a line drawn on the central axis of the humeral shaft and a line drawn perpendicular to the humeral anatomical neck. (B) Plate height: a distance between the lateral edge of greater tuberosity of the humerus and upper margin of the plate.
RESULTS
The group that underwent plate fixation using MIPO (group A) consisted of 39 patients; and 38 patients were in group B, the group that underwent plate fixation using the deltopectoral approach with allogenous fibular bone graft. Group A had 20 cases of Neer classification two-part fractures (51.3%) and 19 cases of three-part fractures (48.7%); group B had 24 cases of two-part fractures (63.2%) and 14 cases of three-part fractures (36.8%). There were no statistical differences in the basic characteristics between the two groups prior to surgery (Table 1).
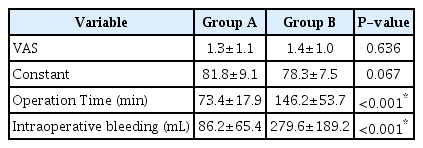
The surgery time was significantly shorter in group A (73.4±17.9 minutes) than in group B (146.2±53.7 minutes) patients (P<0.001). Intraoperative bleeding was also significantly lower in group A (86.2±65.4 mL) than in group B (279.6±189.2 mL; P<0.001). There was no statistically significant difference between the two groups in the evaluation of clinical function by VAS score and Constant score at the 1-year postoperative follow-up (Table 2).
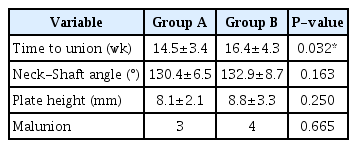
Postoperative radiological evaluation showed fracture union in both groups, and no nonunion was observed. The mean time for fracture union after surgery was 14.5±3.4 weeks (range, 10–22 weeks) in group A patients and 16.4±4.3 weeks (range, 12–28 weeks) in group B patients. Fracture union time was statistically significantly shorter for the group A patients (P=0.032). The neck-shaft angle measured on the AP X-ray images after surgery was 130.4°±6.5° (range, 117.8°–141.1°) in group A and 132.9°±8.7° (range, 112.7°–155.1°) in group B, indicating no difference between the two groups. The plate height was 8.1±2.1 mm (range, 3.6–13.4 mm) in group A and 8.8±3.3 mm (range, 3.0–15.1 mm) in group B, indicating no difference between the two groups. At the radiological evaluation of the final follow-up, the occurrence of malunion (3 cases [7.7%] in group A and 4 cases [10.5%] in group B) (Table 3) did not show a statistically significant difference between the two groups.
DISCUSSION
There have been a number of comparative studies on the clinical and radiological outcomes of different approaches in the surgical treatment of proximal humeral fractures [8,13-18]. Conventionally, the deltopectoral approach is the most commonly used approach for the proximal humerus. This approach is performed in the anterior direction but has the disadvantage of difficulty in maneuvering the fragments in the greater tuberosity area. Also, since the plate is positioned on the lateral side of the humerus, visibility is limited [11]. An extended anterolateral deltoid-splitting approach can be performed; however, there is a possibility of axillary nerve injury with this approach [19]. Hepp et al. [13] reported that this approach had better clinical outcomes compared to the deltopectoral approach due to the deltoid injury occurring in the operation process. In comparison to the deltopectoral approach, MIPO has been introduced and widely used because this method minimizes deltoid injury [20] and facilitates the placement of the plate. This method also ensures biological healing without compromising the blood flow at the periosteum [21]. There have been various reports on differences in clinical and radiological results between the MIPO and deltopectoral approaches. In particular, the recent meta-analysis by Li et al. [17] showed that MIPO had better outcomes than open reduction in terms of bleeding during surgery, operation time, postoperative pain, time taken for bone union, and functional score. However, this method required a longer radiation exposure time during the surgery and had a higher incidence of axillary nerve injury. Sohn et al. [15] reported no significant differences in the clinical and radiological evaluation of the two approaches in prospective studies, but MIPO was significantly less time-consuming. This can be advantageous in the treatment of polytrauma patients. In this study, allogenous fibular bone graft, which is not a simple open reduction, was performed in all patients; as a result, similar to previous findings, MIPO involved less bleeding during surgery and less surgical time. This was significantly different compared to the allogenous fibular bone graft group. Additionally, the time required for the fracture healing was less in the MIPO because, in order to perform allogenous fibular bone graft, spreading the fracture site for space is necessary. With MIPO, however, periosteum is kept intact. This is advantageous in terms of fracture healing. In this study, no axillary nerve injury was found among the patients who underwent MIPO. Axillary nerve injury can be prevented during the surgery by prior palpation of the area in which the axillary nerve passes under the deltoid and protecting the nerve using a finger. The nerve is also protected by performing blunt dissection using Cobb retractor, by use of the opposite finger when inserting a plate, and by inserting the plate with deltoid lifted.
Attempts have been made in order to prevent problems such as cutout or loosening of the screw or varus malalignment that may occur after the plate fixation procedure in patients with severe osteoporosis or comminuted fracture. One method used has been the intramedullary allogenic bone graft [22-24]. In addition, several studies compared clinical and radiological results with and without allogenous bone graft in patients who underwent open reduction using the same locking plate. Cha et al. [25] reported that, in radiological evaluation in the postoperative follow-up, allogenous bone graft maintained the reduction better. Furthermore, Cui et al. [26] also recently reported that in terms of clinical results, the allogenous bone graft group had better outcomes. In this study, however, there was no difference in clinical and radiological results between the patients who underwent plate fixation through MIPO and those who underwent allogenous fibular bone graft in open reduction in the final postoperative follow-up. There was also no difference in the number of malunion occurrences.
Considering that the bone densities measured in the two groups were similar and that the fracture patterns of the two groups evaluated by Neer classification were also similar, the findings indicate that the neck-shaft angle is maintained after surgery to the same extent as providing sufficient medial support with a bone graft although there was no medial calcar screw insertion in the MIPO. In the case of MIPO with accompanying medial comminution, the immobilization period was longer than that of other patients and rehabilitation was performed slowly. The results indicate that with the open reduction, excess intervention on the fracture site is inevitable during the allogenous fibula bone graft process through open reduction, which certainly causes injury to the periosteum and in the soft tissue. Such intervention of the fracture site can be minimized in the simple MIPO, and, barring the presence of a severe comminuted fracture, sufficient support of the fracture site can be provided.
Neer classification four-part fractures were not included in this study. In the case of four-part fractures, difficulty arises in precise reduction of the fracture site through MIPO. In particular, there are cases when allogenous fibular bone graft is needed, such as severe comminuted fracture of the medial cortical bone, but treatment by MIPO has limitations. Recently, Noh et al. [27] reported that allogenous fibular bone grafts with MIPO for three-, four-part fractures showed good clinical results. Sohn and Shin [11] examined the difference in clinical and radiological results according to the type of fracture in the group of patients with proximal humeral fractures who underwent MIPO. This group reported that difficult arises in achieving good outcomes with MIPO in four-part fractures. Although not included in this study, the authors attempted MIPO in the case of a four-part fracture; but sufficient reduction was not possible, so the surgery proceeded with an extended anterolateral deltoid-splitting approach. The most important aspect in the internal fixation of fractures is the sufficient anatomical reduction of the fracture site rather than the surgical approach. Therefore, the flexibility is required in choosing MIPO or open reduction for sufficient reduction of the fracture site.
In this study, the two surgeons performed surgical treatment on the same group of patients only with their respective preferred surgical method. One surgeon performed the surgery with a belief that MIPO alone could provide sufficient fixation for two- and three-part fractures. Another surgeon preferred open reduction using allogenous fibular bone graft in all patients with two- or three-part fracture to facilitate reduction. This allowed for support of the medial cortex of inserted bone by use of an intramedullary nail. Furthermore, the two medical institutions are adjacent to each other, and the patient groups are similar. The two surgeons have similar clinical and surgical experiences, and the general characteristics of the two patient groups did not differ. Under these conditions, we believe that this study was suitable to compare between the two surgical methods.
Based on the results of this study, performing allogenous fibular bone graft in two- or three-part fractures does not seem to have a significant advantage over performing MIPO alone. Rather, allogenous fibular bone grafting caused longer surgery times, increased bleeding, and prolonged fracture healing. In particular, considering the additional cost from the use of allogeneic bone and risk of complications such as infection, we believe that the concurrent allogenous fibular bone graft does not have advantages for general use. Kim et al. [28] also reported that the performance of allogenous fibular bone graft did not significantly affect the clinical outcomes in three-part fractures.
This study had some limitations. First, the population size was relatively small. Also, this was a retrospective study, and different surgeries were performed by two different surgeons in two medical institutions. Although both practitioners are shoulder surgeons with similar clinical experience, ruling out the possibility of subjective intervention by the practitioner in terms of classifying fractures and determining the need for surgical method is difficult. However, considering that the surgery was performed using the same instrument and there were no complications such as malunion after surgery, we believe that the difference between the surgeons did not have a significant impact on the results. The importance of this study is that this is the first study to compare the differences between plate fixation through MIPO and allogenous fibular bone graft through open reduction.
The MIPO and allogenous fibular bone graft through open reduction showed similar clinical and radiological results in the fixation using locking plate in Neer classification two- or three-part proximal humeral fractures. However, allogenous fibular bone grafts required longer surgical time, caused more bleeding, and required a longer time for fracture healing compared to MIPO. Hence, careful consideration is required when selecting the fixation method according to fracture comminution.
Notes
Financial support
None.
Conflict of interest
None.