Short- to mid-term outcomes of radial head replacement for complex radial head fractures
Article information
Abstract
Background
The purpose of the current study was to investigate short- to mid-term outcomes and complications following radial head replacement (RHR) for complex radial head fractures and to identify factors associated with clinical outcomes.
Methods
Twenty-four patients with complex radial head fractures were treated by RHR. The mean age of the patients was 49.8 years (range, 19–73 years). Clinical and radiographic outcomes were evaluated for a mean follow-up period of 58.9 months (range, 27–163 months) using the visual analog scale (VAS) score for pain, the Mayo elbow performance score (MEPS), the quick disabilities of the arm, shoulder and hand (Quick-DASH) score, and serial plain radiographs. Complications were also evaluated.
Results
At the final follow-up, the mean VAS score, MEPS, and Quick-DASH score were 0.6±1.1, 88.7±11.5, and 19.4±7.8, respectively. The mean range of motion was 132.7° of flexion, 4.7° of extension, 76.2° of pronation, and 77.5° of supination. Periprosthetic lucency was observed in six patients (25%). Heterotopic ossification was observed in four patients (16.7%). Arthritic change of the elbow joint developed in seven patients (29.2%). Capitellar wear was found in five patients (20.8%). Arthritic change of the elbow joint was significantly correlated with MEPS (P=0.047). Four cases of complications (16.6%) were observed, including two cases of major complications (one stiffness with heterotopic ossification and progressive ulnar neuropathy and one stiffness) and two cases of minor complications (two transient ulnar neuropathy).
Conclusions
RHR for the treatment of complex radial head fractures yielded satisfactory short- to mid-term clinical outcomes, though radiographic complications were relatively high.
INTRODUCTION
Radial head fractures are relatively common in orthopedic injuries, comprising 1.7%–5.4% of all fractures, 33% of those being around the elbow joint [1]. Although radial head fractures are often stable injuries, one-third are associated with another bone or soft tissue injury, including coronoid fracture, ligamentous injuries, or elbow dislocation [2]. The goal of treatment is to restore the structure of the radial head, which functions as an important stabilizer to varus and valgus stress of the elbow [3]. The Mason classification is commonly used for radial head fractures [4]. Type I and II fractures are treated either non-operatively or by open reduction and internal fixation (ORIF). Type III and IV fractures are treated by ORIF or radial head replacement (RHR). However, the ideal treatment method continues to be controversial.
Numerous studies have compared the clinical outcomes of ORIF and RHR for Mason type III or IV fractures. Several studies have reported that ORIF achieves more satisfactory results in complex radial head fractures [5,6]. Conversely, some studies have reported that RHR produces superior outcomes compared with ORIF by providing early stability [7,8]. ORIF can result in a malunion or a painful, stiff elbow due to bone resorption and loosening [9,10]. Ring et al. [10] emphasized that fractures with more than three articular fragments had an unsatisfactory result after ORIF. In complex radial head fractures that are considered unreconstructable by ORIF, RHR offers better results than ORIF by achieving effective radiocapitellar contact, which improves the stability of the elbow [11].
RHR is indicated in cases of unreconstructable isolated radial head fractures and complex elbow injuries such as elbow fracture-dislocation, terrible triad injuries, Monteggia fractures, or Essex-Lopresti lesions [2]. Although RHR produces satisfactory outcomes [12,13], several studies have reported that it has a high percentage of complications and a higher risk of requiring reoperation [14-16]. With these distinct benefits and risks, it remains to be determined whether RHR should become the primary treatment for complex radial head fractures. The primary aim of the current study was to investigate short- to mid-term outcomes and complications after RHR for complex radial head fractures. The secondary aim was to identify the factors associated with clinical outcomes following RHR.
METHODS
The current study was approved by Institutional Review Board of Keimyung University Dongsan Hospital (IRB No. 2020-11-006). Cases for 29 patients with RHR for complex radial head fractures at a single institution between 2006 and 2018 were retrospectively reviewed. The indications for RHR were complex radial head fractures with associated injuries including ligamentous injuries, terrible triad injuries, Monteggia fractures, or Essex-Lopresti lesions. Inclusion criteria were as follows: (1) RHR for complex radial head fracture, (2) available medical records and radiographic findings, and (3) follow-up period of more than 2 years following surgery. Exclusion criteria were (1) fracture sequelae and (2) failed ORIF. After applying the inclusion and exclusion criteria, 24 patients were included in the current study.
The mean age of the patients was 49.8 years (range, 19–73 years). There were 11 women and 13 men. According to the Mason classification, 12 patients had type III fracture and 12 had type IV fracture. One patient had an open fracture. The mean interval from initial trauma to surgery was 8.7 days (range, 1–67 days) (Table 1). The EVOLVE radial head system (Wright Medical Technology, Memphis, TN, USA) was used in 10 cases, the Anatomic radial head system (Acumed, Hillsboro, OR, USA) in seven cases, the ExploR radial head system (Zimmer-Biomet, Warsaw, IN, USA) in five cases, and the RHS radial head system (Tornier, Montbonnot-Saint-Martin, France) in two cases.
Additional fixation of adjacent bone and ligamentous injuries was performed for complex elbow injuries. Eleven patients had lateral collateral ligament repair, seven had fixation of the coronoid or the olecranon, two had medial collateral ligament repair, and one had triceps tendon repair. After surgery, patients were immobilized with a splint for 1 week. If no complications including wound problems or instability were present, passive rehabilitation using a hinged brace was begun 1 week postoperatively.
The mean follow-up period for patients was 58.9 months (range, 27–163 months). Clinical outcomes were assessed using the visual analogue scale (VAS) score for pain, the Mayo elbow performance score (MEPS), the quick disabilities of the arm, shoulder and hand (Quick-DASH) score, and active range of motion (ROM) of the elbow joint. For all patients, serial plain radiographs including anteroposterior, lateral, and both oblique views were used to evaluate periprosthetic lucency, heterotopic ossification, arthritic change of the elbow joint, and capitellar wear. Periprosthetic lucency was evaluated based on the number of zones and the amount of lucency around the prosthesis, and it was classified into four types (none, mild, moderate, or severe), as described by Grewal et al. [17]. Heterotopic ossification was graded according to the classification of Hastings and Graham [18]: type 1 does not cause a functional outcome; type 2 has some functional limitation: 2A represents an elbow flexion contracture of 30o or greater and limited flexion of less than 130°, 2B represents limited forearm rotation of less than 50° pronation or less than 50° supination, and 2C represents heterotopic bone causing limitations in both planes of motion; and type 3 has ankyloses that prevent elbow motion. Arthritic change of the elbow joint was assessed on anteroposterior and lateral radiographs at the final follow-up evaluation and classified into four grades (normal, mild, moderate, or severe), as described by Broberg and Morrey [19]. Capitellar wear was graded as none, mild, moderate, or severe, as described by Lamas et al. [20]. Periprosthetic lucency, arthritic change of the elbow joint, and capitellar wear that were above the moderate degree were considered significant. Complications were classified as either minor, those that did not compromise the outcome or require any further treatment, or major, those that compromised the outcome or required a reoperation .
Statistical Analysis
Statistical analysis was conducted using IBM SPSS ver. 26.0 (IBM Corp., Armonk, NY, USA). Kendall’s tau B correlation analysis and Mann-Whitney U-tests were conducted to determine the correlations between final clinical scores and various parameters such as age, sex, Mason classification, time interval from initial trauma to surgery, periprosthetic lucency, heterotopic ossification, arthritic change of the elbow joint, and capitellar wear. Statistical significance was set at P<0.05.
RESULTS
Clinical Outcomes
At the final follow-up evaluation, the mean VAS score for pain was 0.6±1.1. Fifteen patients had no pain, eight had mild pain, and one had moderate pain. The mean MEPS was 88.7±11.5, with 14 excellent, 9 good, and 1 poor result. The mean Quick-DASH score was 19.4±7.8. The mean ROM was 132.7°±7.4° of flexion, 4.7°±10.8° of extension, 76.2°±10.6° of pronation, and 77.5°±5.3° of supination.
Radiographic Outcomes
Based on the plain radiographs at the final follow-up evaluation, significant periprosthetic lucency was found in six patients (25%): two moderate and four severe; of the remaining patients, seven had mild periprosthetic lucency, and 11 patients had none. Significant heterotopic ossification that affects functional outcomes was found in four patients (16.7%): two with type 2A and two with type 3; 16 of the remaining patients had type I, and four patients had no heterotopic ossification. Significant arthritic change of the elbow joint was found in seven patients (29.2%), all moderate, while nine patients had a mild degree of arthritic change and eight patients were normal. Significant capitellar wear was found in five patients (20.8%), all moderate, while 10 patients had mild capitellar wear and nine patients had none (Table 2).
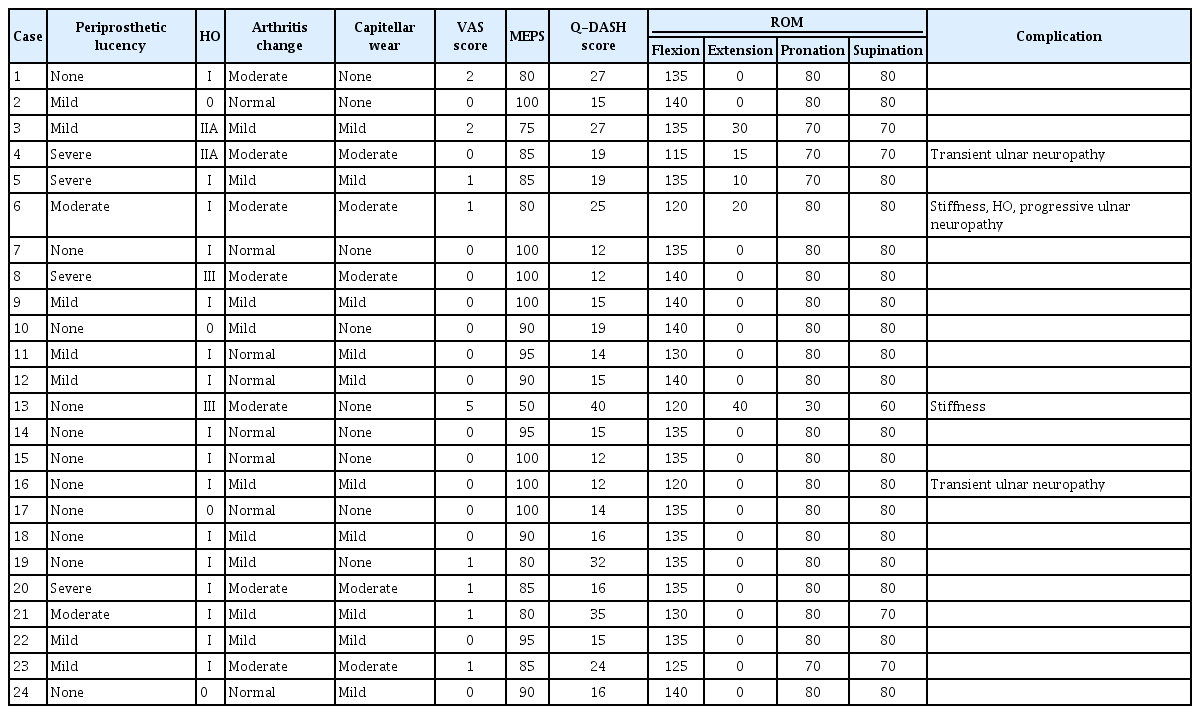
Summary of the outcomes and complications after radial head replacement in patients with complex radial head fracture
There were no significant correlations between the final clinical scores and various parameters including age, sex, Mason classification, time interval from initial trauma to surgery, periprosthetic lucency, heterotopic ossification, and capitellar wear (P>0.05). However, arthritis change of the elbow joint was significantly correlated with MEPS (P=0.047) (Table 3).
Four cases of complications (16.7%) in 24 patients were observed, including two cases of major complications and two cases of minor complications. The two patients with major complications (8.3%) required a reoperation. One patient had stiffness with heterotopic ossification and progressive ulnar neuropathy and underwent arthrolysis and ulnar nerve anterior transposition at 6 months after surgery. The other patient with RHR for open fracture had severe stiffness 3 months after surgery. Four months after surgery, he underwent arthrolysis and removal of the implant for severe ankylosis. The two patients with minor complications had transient ulnar neuropathy but were completely recovered within 4 months.
DISCUSSION
The present study revealed that RHR for complex radial head fractures produced satisfactory short to mid-term clinical outcomes, although the rate of radiographic complications was relatively high. Arthritic change of the elbow joint was correlated with clinical scores. The results presented here indicate that RHR is an effective option for treatment of complex radial head fractures.
In complex radial head fractures, the results after ORIF are highly variable and have had many failures [21]. Even a successful ORIF can often result in osteonecrosis of the fragments, failure of hardware which generates stiffness, and unstable or painful elbow [10]. RHR is indicated in cases of unreconstructable isolated radial head fractures and complex elbow injuries [2]. Indications for RHR in the current study were complex radial head fractures with associated injuries including ligamentous injuries, terrible triad injuries, Monteggia fractures, or Essex-Lopresti lesions. Recently, RHR has been widely used in the treatment of complex radial head fractures. However, the use of RHR has been debated due to a relative lack of studies on the long-term outcomes [14,22]. Several reports have compared ORIF and RHR in complex radial head fractures [23,24]. In a systematic review, Dou et al. [11] reported that patients with Mason type III fractures receiving RHR had a significantly higher satisfaction rate compared to those with ORIF, as well as better Broberg and Morrey scores and a lower rate of complications. In a recent systematic review with meta-analysis, Li and Chen [9] reported a higher complication rate for ORIF than RHR for Mason type III fractures (58.1% vs. 13.9%), but the satisfaction rate was higher with RHR than with ORIF (91.7% vs. 51.6%). Bone non-union/bone absorption was the main reported complication of ORIF at 50%.
Tarallo et al. [12] reported on 31 cases of RHR for Mason type III fractures with a mean follow-up of 30 months. Cases presented with good clinical results based on the MEPS: excellent in 77% of the patients, good in 10%, and fair in 4%. Sershon et al. [13] reported on 16 cases of RHR for radial head fractures with a mean follow-up period of 10.5 years with good to excellent MEPS in 15 patients (94%), one patient reporting a fair outcome, and no patients reporting a poor outcome. In the present study, at a mean follow-up of 58.4 months, based on the MEPS, excellent results were obtained in 14 patients (58.3%), good in nine patients (37.5%), and poor in one patient (4.2%). The current findings are consistent with those of previous studies, suggesting that RHR is a reasonable option, producing good clinical outcomes in patients with complex radial head fractures.
Several studies have reported the relationship between radiographic findings and clinical outcomes of RHR [25,26]. Ha et al. [1] performed a 10-year retrospective review of 258 radial head implants in 244 patients. Radiographic complications included heterotopic ossification (46.9%), arthritic change of the elbow joint (27.9%), loosening (19.8%), fracture (2.3%), and hardware dislocation (2.7%). Overall, there were 62 reoperations (24.0%), and heterotopic ossification (53.2%) was the most common cause. A significant correlation between radiographic complications and clinical outcomes was reported. Age, sex, side, and type of arthroplasty did not correlate with either the clinical or radiographic outcomes. Chen et al. [26] reported long-term outcomes after RHR for unreconstructable radial head fractures where 26 of 32 patients had good to excellent results. At a mean follow-up of 8.9 years, the mean MEPS was 83.4 points, and the mean Quick-DASH score was 11.7. Additionally, periprosthetic lucency did not correlate with functional or pain scores. Fehringer et al. [25] reported on 17 patients who underwent metal RHR with smooth stems for comminuted radial head fractures with a minimum 2-year follow-up. Results indicated that “mean stem radiolucency” did not correlate with proximal radial forearm pain. The current study revealed a significant correlation between arthritic change of the elbow joint and MEPS. Periprosthetic lucency, heterotopic ossification, and capitellar wear did not correlate with clinical scores. However, further long-term follow-up studies of a larger scale are needed to account for the possibility of late progression.
Various factors (e.g., patient characteristics and types of RHR implant) that affect clinical outcomes, complications, and reoperation of RHR have been reported. Duckworth et al. [15] reported on 105 patients who underwent RHR for complex radial head fractures. All implants were uncemented monopolar prostheses, with 86% being metallic and 14% being silastic. Twenty-nine patients (28%) underwent reoperation due to one of the following complications: stiffness (n=12), painful loosening (n=5), isolated pain (n=4), subluxation (n=3), synovitis (n=2), ulnar neuropathy (n=2), or infection (n=1). Results demonstrated that silastic implants and lower age were independent risk factors for reoperation. Lott et al. [2] retrospectively reviewed 18 stable and 50 unstable elbow injury groups treated with RHR by a single surgeon during a 15-year period. The results showed that the unstable elbow injury group achieved satisfactory functional ROM with no difference in radiographic outcomes, complication rates, or implant survivorship compared with the stable elbow injury group. In a recent systematic review and meta-analysis, Agyeman et al. [27] examined fixation methods to determine if “fixed” or “unfixed” resulted in better clinical outcomes. The results identified 878 unduplicated patients, 522 fixed and 356 unfixed. Implant fixation type did not appear to affect clinical outcomes of RHR. However, rigidly fixing the implant (cement implant) may have increased the risks of reoperation and complications. In the current study, there were no significant correlations between the final clinical scores and age, sex, Mason classification, or time interval from initial trauma to surgery. Because of the small sample size, we could not analyze the outcomes according to implant design. Our overall complication and reoperation rates were 16.6% and 8.3%, respectively, including two cases of major complications (one stiffness with heterotopic ossification and progressive ulnar neuropathy and one stiffness) and two cases of minor complications (two transient ulnar neuropathy). These results were either in line with or better than previous RHR studies.
The current study had several limitations. First, it was a retrospective study with a small number of cases. Second, heterogeneous RHR implants were used, which could have affected clinical outcomes. Third, the follow-up period was relatively short and heterogeneous. Additionally, exact radiographic results that are important in long-term implant survival were not provided. Future long-term prospective studies are needed to evaluate clinical and radiographic outcomes after RHR for complex elbow fractures.
RHR for the treatment of complex radial head fractures yielded satisfactory short to mid-term clinical outcomes, though radiographic complications were relatively high. Results suggest that radiographic complications did not compromise clinical outcomes, and only arthritic change of the elbow joint was correlated with clinical scores. Further long-term studies are needed to fully understand the clinical outcomes and complication rates of RHR.
Notes
Financial support
This study was supported by the National Research Foundation of Korea, funded by the Korean government (grant number 2017 R1D1A1B03035113 and 2014R1A5A2010008).
Conflict of interest
None.


