Current concepts in the treatment of midshaft clavicle fractures in adults
Article information
Abstract
Midshaft clavicle fractures are the most common fracture of the clavicle accounting for 80% of all clavicle fractures. Traditionally, midshaft clavicle fractures are treated with conservative treatment even when prominent displacement is observed; however, recent studies revealed that nonunion or malunion rate may be higher with conservative treatment. Moreover, recent studies have shown better functional results and patient satisfaction with surgical treatment. This review article provides a review of clavicle anatomy, describes the current clavicle fracture classification system, and outlines various treatment options including current surgical options for clavicle fracture in adults.
INTRODUCTION
Clavicle fractures are upper extremity fractures, and are one of the most common broken bones seen in the emergency room setting, accounting for 35% to 44% of shoulder girdle fractures and 2% to 5% of all adult fractures [1-3]. Direct trauma to the clavicle, as in contact sports or motorcycle and bicycle accidents, is the most common cause of fracture. Males are more often affected than females, and clavicle fractures most commonly occur in patients younger than 30 years of age. Although 88.2% of all clavicle fractures occur in younger adults, a bimodal peak is observed in elderly patients due to simple falls from moderate height or falls from bed [4].
Most clavicle fractures occur in the midshaft accounting for about 80% of all clavicle fractures, followed by distal clavicle and medial clavicle fractures [5]. Traditionally, most clavicle fractures are treated nonoperatively; however, various strategies for the surgical treatment of displaced midshaft fractures have been reported recently, including interfragmentary screw fixation, intramedullary (IM) fixation, cerclage wiring, and plate fixation. Recently, attempts to use three-dimensional (3D) printing technology on fracture surgery have been made [6,7].
Although numerous studies have reported on the management of midshaft clavicle fractures, definitive treatment strategies have not been defined and the various surgical techniques used have not been described. In this article, we review the anatomy of the clavicle, review both surgical and nonsurgical options for midshaft clavicle fractures reported thus far, and discuss the optimal treatment options for fractured clavicles in adults.
ANATOMY OF THE CLAVICLE
The human clavicle is a unique double-curved S-shaped 3D structure with a complex morphology. It offers the only direct link between the axial and appendicular skeleton [8,9]. It is highly variable within a given population; variation exists not only in length, which is approximately 140 to 150 mm (range, 118–162 mm) and diameter but also in its cross-section and the degree of bowing. In addition, personal deviation in human clavicle anatomy is large and variations between males and females have been reported [10-12]. Generally, the human clavicle is presumed to be anatomically symmetric; however, there are only a few studies assessing symmetricity of the human clavicle. Cunningham et al. [13] assessed side-to-side variation in clavicle length in uninjured adults with computed tomography (CT) and reported symmetry in 71.5% of all patients. A recent study by Hoogervorst et al. [14] reported that 30% of patients had side-to-side asymmetry of 5 mm or more, and there was a significant association between clavicle length and dominant side or sex.
The human clavicle is prone to fracture due to multiple reasons. It is one of the least-protected bones by muscle or fat, since it is located superficially just beneath the skin and platysma muscle [1,15]. The clavicle articulates with the sternum medially forming the sternoclavicular joint and articulates with the acromion laterally forming the acromioclavicular joint. Both joints provide stability with muscle and ligamentous support. It is a relatively thin bone with a mean cortical thickness of 2.05 mm at the midpoint [16]. In the middle third of the clavicle, the thin diameter, curved shape, and absence of stability provided by articulation make it prone to fracture [15]. Also, it is prone to fracture between the midshaft and distal one-third, where the midshaft tubular structure transitions to a flat shape structure distally [17].
CLAVICLE FRACTURE CLASSIFICATION
Several classification systems for clavicle fractures have been introduced since the 1960s. The Allman classification was first introduced in 1967 [18], which is based on anatomic location and was the first widely accepted classification system for clavicle fractures. Fractures within the middle third were referred to as type I fractures, those within the lateral third were type II fractures, and medial third were type III. Later on, Neer [19] subclassified the fractures of the lateral third, which were categorized based on the fracture location in relation to the coracoclavicular ligament that provides stability of the medial fracture segment. However, these classification systems do not consider treatment options nor prognosis of fractures [20].
Robinson [3] introduced a more detailed classification based on fracture location, adding the concept of displacement, angulation, intra-articular extension, and comminution of the fracture, where subgroups A and B include fractures displaced less than and greater than 100%, respectively. The middle third fractures are also subdivided by the degree of comminution and fracture pattern, with simple or wedge-type fractures categorized as subgroup 1 and comminuted or segmental fracture patterns categorized as subgroup 2. Finally, medial and lateral fractures are subdivided based on intra-articular extensions.
For lateral clavicle fractures, Craig modified Neer type II fractures by separately classifying intra-articular and pediatric fractures by emphasizing the importance of the conoid ligament [21]. Recently, Cho et al. [22] suggested a new classification system considering fracture displacement, stability, and fracture location to help surgeons choose the most optimal treatment option for each type of fracture. This classification system defined type I fractures as stable and type II as unstable with significant displacement. Type II fractures are subcategorized into four subtypes by fracture location and whether the conoid or trapezoid ligaments are damaged.
CONSERVATIVE TREATMENT
Historically, the majority of midshaft clavicle fractures have been treated nonoperatively, famously based on two large case series by Neer [23] and Rowe [24] in the 1960s. Neer [23] reported a low nonunion rate of 0.13% within 2,234 patients and Rowe [24] reported a rate of 0.8% in 566 patients.
Immobilizing the involved shoulder with a figure-of-eight brace or bandage is the most widely used conservative treatment. The goal of applying a figure-of-eight brace is to elevate and extend the shoulder to bring the distal fragment close to the proximal fragment [24]. Recently, however, the use of sling immobilization has increased, since complaints including pain and discomfort were reported with immobilization using a figure-of-eight bandage. Moreover, there are multiple studies reporting that sling immobilization is superior to the figure-of-eight brace immobilization [25,26]. Although there was no difference in the rate of nonunion or union time between sling immobilization and figure-of-eight brace immobilization, lower satisfaction, lower functional scores, and higher pain scores were seen with the figure-of-eight brace immobilization. Other reported complications with the figure-of-eight brace include axillary skin irritation, temporary brachial plexus palsy, and deep venous thrombosis [27,28]. Immobilization is recommended for 4 to 6 weeks allowing for a passive range of motion not above 90° forward flexion. In most cases, the sling or brace is removed after 6 weeks. Also, a light amount of work may be allowed but weight-bearing is allowed only at 3 months and return to sports at 4 to 6 months after injury [29,30].
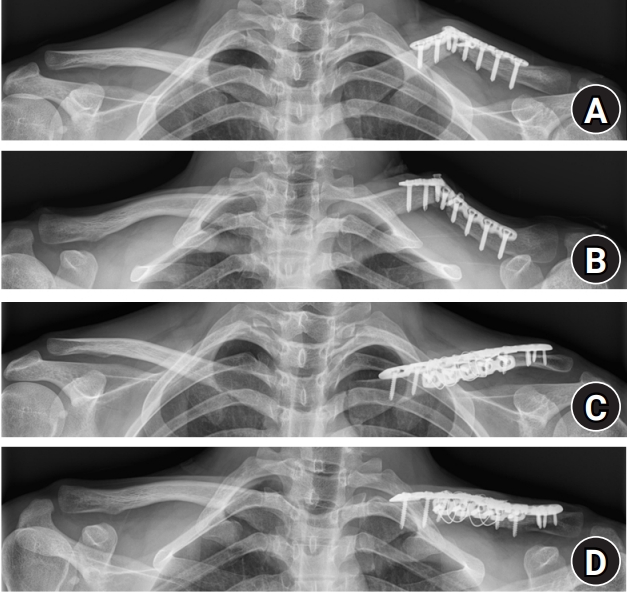
The low nonunion rates reported by Neer [23] and Rowe [24] cannot avoid criticism since pediatric fractures, in which nonunion is rare, were included. Higher nonunion rates in clavicle fractures with conservative treatment were reported in many studies ranging from 7% to 15%, and even with fracture union, complications such as shortening, angulation, malunion, and lower clinical outcomes were reported (Fig. 1) [29,31-33]. Recent studies excluding pediatric clavicle fractures reported a higher nonunion rate of 15% to 20% with nonoperative treatment with displaced clavicle midshaft fractures [32,34,35]. Moreover, unsatisfactory clinical outcomes and complications including cosmetic problems such as skin protrusion were reported [32,36].
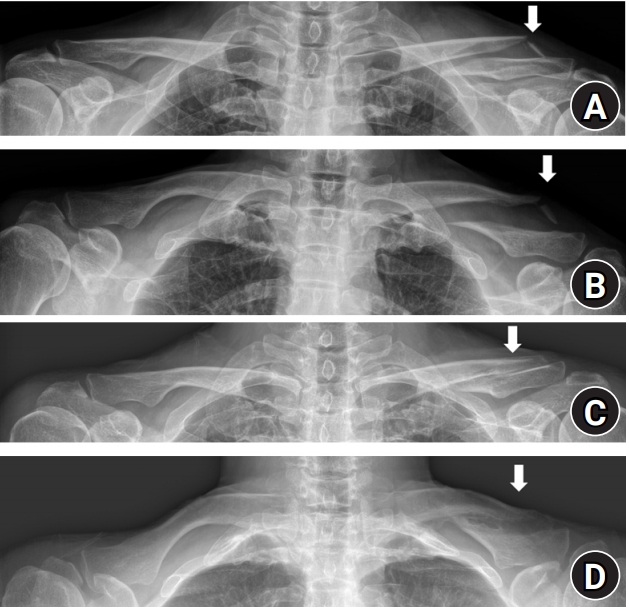
Serial radiographs from a 48-year-old man with conservative treatment of a midshaft clavicle fracture with comminution and shortening. Surgical treatment was recommended initially; however, since the patient underwent multiple surgeries due to Charcot joint arthropathy in the ankle, the patient refused operative treatment. Malunion is observed 3 years post-accident on plain radiographs. (A) Initial anteroposterior (AP) view. (B) Initial caudal view. (C) AP view 3 years post-accident. (D) Caudal view on 3 years post-accident. Arrows indicate fracture site.
Shortening of the clavicle after fracture should be carefully assessed as shortening greater than 2 cm may be prone to nonunion [35]. Also, shortening of the clavicle can affect the biomechanical principle of the shoulder girdle by altering the moment arm of shoulder muscles. Altered biomechanics of the shoulder girdle may result in muscle fatigability and impair shoulder function. Hill et al. [32] reported that initial shortening of more than 2 cm was highly associated with nonunion and unsatisfactory results including residual pain, evidence of brachial plexus irritation, and cosmetic problems. Wick et al. [37] recommended operative treatment for clavicle fractures with a shortening of more than 2 cm to avoid nonunion. In a study by Ledger et al. [38], shortening was measured by CT and showed that shortening greater than 1.5 cm was associated with weaker muscle strength compared to the contralateral side. With a self-administered shoulder questionnaire [39], the severity of symptoms was assessed and the functional status of the shoulder and poor clinical outcomes were found compared to the uninjured contralateral side. However, shortening alone as an operative indication is still in controversy. A recent systemic review conducted by Woltz et al. [40] reported that shortening alone is not an evidence-based indication for operative treatment.
SURGICAL TREATMENT
There have been many attempts to define the optimal treatment options for displaced midshaft clavicle fractures. Including the randomized controlled trial (RCT) performed by The Canadian Orthopaedic Trauma Society (COTS) [5], recent studies reported patients with open reduction and internal fixation (ORIF) showed lower rates of malunion and better clinical outcomes [41,42]. Although the optimal treatment for displaced midshaft clavicle fractures is not defined, it is still under investigation with multiple comparative studies comparing surgical and nonsurgical management and different methods of surgical fixation techniques.
Surgical treatment as an optimal treatment for clavicle fracture became a trend after the COTS study results [5] were released that showed the surgically treated group with superior plates showed lower rates of nonunion and faster time to union. In addition, clinical outcomes such as functional scores and satisfaction were better in the surgically treated group. The complications reported in the surgically treated group included implant irritation, wound infection, and wound dehiscence [41].
Surgical treatment, as assessed on plain radiographs when shortening is greater than 2 cm, is considered when displacement is greater than 100% and when a Z-type fracture, which is a comminuted fracture with a displaced and rotated butterfly fragment between major fragments, is seen and notable comminution is observed [5,35]. Also, in patients with young age and high level of activity, surgical treatment may be preferred.
Plate and screw fixation is commonly accepted as a standard method in surgical treatment. Other surgical techniques including fixation with IM nails, cerclage wiring, interfragmentary wiring, or bioabsorbable screws have been introduced (Figs. 2 and 3). Also, based on advancements in 3D printing technology, surgical treatment with the aid of 3D printing has been introduced [6,43,44].
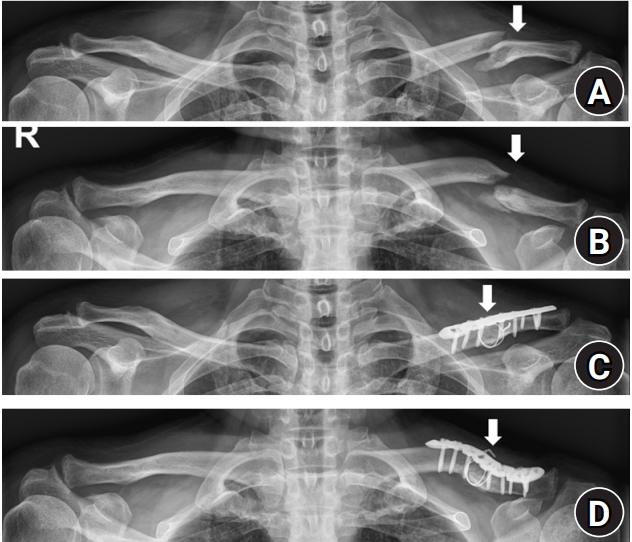
Radiographs of a 63-year-old man who sustained a comminuted left midshaft clavicle fracture. (A) Anteroposterior (AP) view. (B) Caudal view. The patient underwent plate fixation with two cerclage wirings. Union was achieved in 1-year postoperative radiographs. (C) AP view. (D) Caudal view. Arrows indicate fracture site.
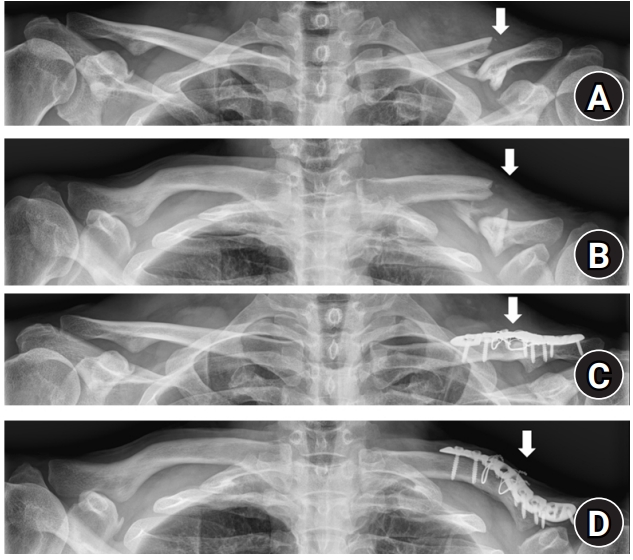
Radiographs of a 60-year-old man who sustained a comminuted left midshaft clavicle fracture. (A) Anteroposterior (AP) view. (B) Caudal view. The patient underwent plate fixation with four interfragmentary wirings. Union was achieved in 1-year postoperative radiographs. (C) AP view. (D) Caudal view. Arrows indicate fracture site.
Plate and Screw Fixation
Plate and screw ORIF is considered the gold standard surgical option. Plate and screw fixation provides rigid fixation with cortical compression and rotational control. Multiple RCTs have reported a lower nonunion rate compared with nonoperative treatment ranging from 0% to 2.8% when using plate and screw fixation [29,40]. However, secondary operation may be required mostly due to the prominent hardware causing cosmetic problems or implant irritation. Leroux et al. [45] reported that 25% of patients who underwent ORIF with plate and screw fixation required reoperation for removal. Other complications for plate and screw fixation include wound infection and wound dehiscence [5]. Complications around major neurovascular structures will be discussed below.
Superior Plating vs. Anteroinferior Plating
While the common plating positions are superior and anteroinferior (Fig. 4), the optimal position of the plate is still controversial. Superior plating has been traditionally used because it allows fixation on the tension side of the fracture. However, since complications have emerged, including hardware prominence and concern on screw trajectory angle which aims toward major vascular structures, anteroinferior plating has gained attention. By placing the plate anteroinferior, screws with greater length can be used which offer more stability, especially against rotational force [46-48]. Several biomechanical studies comparing strength based on plate position have been conducted with different results. Iannotti et al. [49] reported superior plating was the strongest biomechanical construct using midshaft clavicle fracture models with a transverse osteotomy after applying axial and torsional force. On the other hand, some studies reported that anteroinferior plating led to greater resistance to cantilever bending, although there was no significant difference in resisting axial or torsional forces [46,50,51].
Radiographs of a 23-year-old man who sustained re-fracture with metallic failure after plate fixation from another clinic. (A) Anteroposterior (AP) view. (B) Caudal view. The patient underwent double plate fixation with a superior plate and anteroinferior plate. Six-month postoperative radiographs are shown. (C) AP view. (D) Caudal view.
While the less prominent hardware in anteroinferior plating reduces the need for hardware removal later on, Hulsmans et al. [52] reported an equal rate of implant removal between the two techniques. In a study by Sohn et al. [53], no difference in implant irritation was found between the two techniques, and implant prominence problems in the study by Collinge et al. [54] were minimal. Since the location of the clavicle is superficial just beneath the skin and thin platysma muscle [15,30], surgeons must try to decrease implant irritation by meticulous dissection, which preserves the platysma fascial layer to be repaired over the plate.
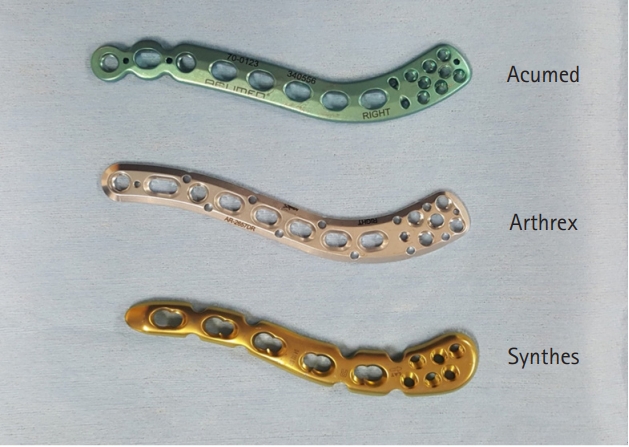
Precontoured Plates
To overcome the complex 3D anatomical features of the human clavicle, anatomical precontoured plates can be used (Fig. 5). Using a precontoured plating system is expected to shorten operation time since no additional bending is needed during surgery and since the plate is precisely anatomically contoured with the bone, cosmetic problems or discomfort by skin protrusion can be prevented. Fleming et al. [55] reported a 100% union rating with no mandatory need for removal using precontoured plates. Chandrasenan et al. [56] revealed that pre-contoured anatomical plates that are fit to the actual clavicle shorten the operation time.
However, due to the complex anatomic features of the human clavicle and diversity among individuals, some studies reported incompatibility of precontoured plates and high rates of implant irritation leading to the need for implant removal [57,58]. Malhas et al. [57] insisted that when using a plating system, it is advantageous to have multiple plate shape variations on hand during surgery due to the anatomic diversities of the human clavicle. Huang et al. [59] revealed that the apex of the superior bow was located on the lateral aspect of the clavicle, making the pre-contoured plate difficult to fit laterally.
Locking vs. Non-locking Plates
After their introduction, locking plates have been very popular for use with clavicle fractures. Locking plates have advantages for use with osteoporotic bone in that they lead to stronger fixation providing minimal contact between the bone and plate, preserving bone blood supply. Locking plates are also used in minimally invasive percutaneous plate osteosynthesis (MIPO). By avoiding periosteal stripping with soft tissue preservation, locking plates with the MIPO technique in clavicle fractures have reported rapid union [10]. On the other hand, concerns with the MIPO technique include the possibility of relatively large fracture gaps, which may result in poor secondary bone healing and shortened or lengthened clavicular malunion leading to functional deficits [60]. Also, strong soft tissue dissection is seldom required to advance the plate and rare complications such as pneumothorax have been reported after MIPO for midshaft clavicle fractures [61]. However, there are multiple studies supporting good clinical and radiologic outcomes using the MIPO technique for clavicle shaft fractures [62-64].
A prospective randomized trial comparing locking superior plate fixation and non-locking superior plate fixation for displaced midshaft fractures was reported. Complication rates and clinical results were similar; however, time to union was shorter with the locking plate group [65].
Complications (Neurovascular Risks) of Plate Fixation
Longitudinal incisions over the clavicle are generally used since vertical incisions have limitations in surgical exposure making it difficult to use longer plates. With longitudinal incisions, it is easy to extend the incision intraoperatively when necessary. During surgical approaches with longitudinal incision, branches of the supraclavicular nerves are at risk. When damaged on the way of approach to the fracture, sensory disorders such as desensitization may occur in the supraclavicular and infraclavicular region, anteromedial aspect of the shoulder, and/or anterosuperior region of chest wall. Wang et al. [66] reported 83% of sensory disorders after plate fixation in clavicle fractures and recommended using the vertical incision.
In addition to superficial sensory disorders, major neurovascular structures located beneath and posterior to the clavicle are a main concern in plate fixation. Damage to the major neurovascular structure during plate fixation is uncommon. Leroux et al. [45] reported only five neurologic complications and five vascular complications out of 1,350 clavicle fractures treated with plate fixation. Caution should be taken when fixation is performed on the medial half. In a cadaveric study by Galley et al. [67], the vascular risk was high in the most medial quarter. On the posterior side of the most medial quarter of the clavicle, the common carotid artery and in particular the internal jugular vein axis is at risk when drilling anterior to posterior. This was later supported by an image study performed by Sinha et al. [68] that showed in their contrast-enhanced CT assessment that drilling should be directed superiorly in the most medial quarter and posteriorly in the second medial quarter. They also suggested superior plating in two medial segments, when divided into three zones, rather than placing the plate on the anterior edge.
Intramedullary Nailing
IM nailing is another good option for surgically treating displaced midshaft clavicle fractures, with comparable results to plate fixation reported in some studies [69-71]. Its advantages include small incisions with less soft tissue dissection, which prevents supraclavicular nerve injury and promotes fracture healing. Also, IM nailing avoids the possibility of damaging major neurovascular structures located beneath the clavicle by drilling or protruded screws when performing plate fixation.
Indications for IM fixation are not different from those for plate fixation. However, severely comminuted fractures or segmental fractures may be contraindications for IM nailing [72]. Implants used in IM nailing include Kirschner wires (K-wires), titanium elastic nails (TENs; Synthes, West Chester, PA, USA), IM screws, and Hagie pins (Smith & Nephew, Andover, MA, USA). There are a number of studies reporting a 100% healing rate using IM nailing whether with Hagie pins or TENs [72]. A meta-analysis by Duan et al. [73] reported a higher rate of union and better functional outcomes with IM nails compared to conservative treatment.
Complication rates are relatively high in IM nailing, as Strauss et al. [74] reported a complication rate of 50% and van der Meijden et al.[70] reported an 85% complication rate. The most common complication using IM nailing is superficial infection around the exposed implant, which includes pin extrusion, skin irritation, or erosion. Other reported complications are implant failure including breakage or bending of the implant.
The better surgical treatment option between plate fixation and IM nailing is unclear as incompatible results have been shown in biomechanical studies. Zeng et al. [69] reported that IM nailing showed more physiologic stress distribution but with greater displacement and implant stresses under axial loads and cantilever bending force compared to plate fixation. However, Ni et al. [75] reported that plate fixation showed an even stress distribution and recommended plate fixation over IM nailing. Another biomechanical analysis using sawbones by Wilson at al. [76] showed that rotational stability was superior with plate fixation compared to IM nailing. In a systemic review by Hulsmans et al. [77], rotational stiffness did not differ significantly; however, plate fixation was superior in torque stiffness. Moreover, plate fixation showed more construct stiffness in a three-point bending test, where both ends of the clavicle were embedded and the load was applied superior to the inferior direction, and cantilever bending test compared to IM nailing.
In clinical studies, a systemic review by Houwert et al. [78] concluded no differences in functional outcomes or complications after plate fixation or IM nailing; however, the results of RCTs performed later showed evidence to the contrary. van der Meijden et al. [70] found that patients with plate fixation had less disability six months from surgery and more patients needed implant removal due to implant irritation in patients treated with IM nailing. Andrade-Silva et al. [71] reported that although no difference was found in time to union or complications, implant irritation rate was higher at 40% in the IM nailing group and at 14% in the plate fixation group. Park et al. [79] reported higher satisfaction with IM nailing, but early postoperative pain and fracture migration were higher with IM nailing, especially in the multi-fragmentary fracture type, suggesting plate fixation in this particular fracture type. A systemic review showed no differences in function or nonunion rate between the two methods, but after implant removal, patients with plate fixation were prone to re-intervention and refracture [80].
Three-Dimensional Printing-Assisted Surgery
3D printing technology has been widely used in orthopedics over the last decade. It has been actively applied in implant design and surgical guides in orthopedics [81,82]. Due to the complex anatomy and diversity between individuals, 3D printing technology aids surgeons to treat clavicle fractures by helping to choose the optimal implant and precontouring the implant preoperatively (Fig. 6).

Bending the plate preoperatively using a three-dimensional (3D) printed model. The plate was bent using benders to match the contour between the 3D printed model and the plate on the best fit location. (A) Arrow indicates a gap between plate and 3D printed model before bending. (B) Arrow indicates resolution of a gap after bending
Kim et al. [6] described a technique using a 3D printed clavicle model to choose the most suitable plate preoperatively. By choosing the best fit plate, displaced comminuted midshaft clavicle fractures were treated with the MIPO technique. van Doremalen et al. [43] adjusted the plate preoperatively with 3D printed models and suggested preoperative preparation with 3D printed models may reduce implant removal caused by plate-related discomfort. Fillat-Gomà et al. [44] showed improvement and enhanced surgical planning not only in clavicle fractures but also in other upper extremity fractures by 3D printing technology. They also applied the plate on a 3D-printed clavicle model and choose the best fitting plate with optimal stability.
There are some obstacles to overcome when using 3D printing technology. First, considerable time and cost is required. Particular CT data using a thin-slice CT protocol is required for reconstruction. Moreover to manufacture a 3D-printed model, a 3D printing system with adequate space is essential. Further studies are needed to prove the benefit of 3D printing technology, including cost-effectiveness. Second, further studies are needed to assess the symmetricity of the clavicle since the contralateral intact clavicle is used as a reference.
CONCLUSIONS
Midshaft clavicle fractures are common upper extremity injuries in adults. Although conservative treatment is the optimal treatment for nondisplaced clavicle fractures, it is still hard to say whether surgical or nonsurgical treatment is the optimal treatment option for displaced midshaft clavicle fractures. However, a consensus has been reached on high nonunion rates for displaced midshaft fractures in adults. Surgical treatment is recommended when shortening is greater than 2 cm, displacement is greater than 100%, Z-type fractures are present, and notable comminution is observed.
Notes
Financial support
None.
Conflict of interest
None.