Can indirect magnetic resonance arthrography be a good alternative to magnetic resonance imaging in diagnosing glenoid labrum lesions?: a prospective study
Article information
Abstract
Background
This study was designed to evaluate and compare the diagnostic value of magnetic resonance imaging (MRI) and indirect magnetic resonance arthrography (I-MRA) imaging with those of arthroscopy and each other.
Methods
This descriptive-analytical study was conducted in 2020. All patients who tested positive for labrum lesions during that year were included in the study. The patients underwent conservative treatment for 6 weeks. In the event of no response to conservative treatment, MRI and I-MRA imaging were conducted, and the patients underwent arthroscopy to determine their ultimate diagnosis and treatment plan. Imaging results were assessed at a 1-week interval by an experienced musculoskeletal radiologist. Image interpretation results and arthroscopy were recorded in the data collection form.
Results
Overall, 35 patients comprised the study. Based on the kappa coefficient, the results indicate that the results of both imaging methods are in agreement with the arthroscopic findings, but the I-MRA consensus rate is higher than that of MRI (0.612±0.157 and 0.749±0.101 vs. 0.449±0.160 and 0.603±0.113). The sensitivity, specificity, negative predictive value, positive predictive value, and accuracy of MRI in detecting labrum tears were77.77%, 75.00%, 91.30%, 50.00%, and 77.14%, respectively, and those of I-MRA were 88.88%, 75.00%, 92.30%, 66.66%, and 85.71%.
Conclusions
Here, I-MRA showed higher diagnostic value than MRI for labral tears. Therefore, it is recommended that I-MRA be used instead of MRI if there is an indication for potential labrum lesions.
INTRODUCTION
The glenohumeral joint is one of the most unstable joints in the body. Many elements are involved in the stability of this joint, including the labrum, a fibrocartilage structure that attaches to the margin of the glenoid [1] and deepens the glenoid cavity by about 30%. This increased depth increases the contact area between the head of the humerus and the glenoid cavity to stabilize the joint. Labrum damage and tears usually happen following shoulder dislocations and lead to pain and instability of the shoulder joint [2,3]. Labral lesions are divided into anterior (Bankart), posterior (reverse Bankart), and superior (SLAP) tears based on tear location [4-6].
Because of the severe pain and limitation of activity caused by labral lesions, the accuracy, efficiency, and cost-effectiveness of associated diagnostic tests need to be evaluated [7]. Physical examination is useful for diagnosing labral lesions; however, it is not enough to choose a type of treatment [8]. Moreover, detecting the exact location and size of the tear and determining the type of lesion is not easy in a physical examination because of the anatomical complexities of the shoulder joint. Therefore, clinicians turn to imaging to provide rich and useful information to support a patient’s medical history and physical examination and to visualize the pathoanatomy of shoulder dysfunction [9].
Magnetic resonance imaging (MRI) and magnetic resonance arthrography (MRA) are two imaging modalities used for labral lesions [10]. Shoulder MRI has become very popular as a screening method for diagnosing labral abnormalities [11]. MRA of the shoulder comprises two types: direct (D-MRA) and indirect (I-MRA). In the I-MRA method, a contrast substance is injected intravenously, increasing the joint space and indirectly enabling arthrography [12,13]. I-MRA is less invasive and more accessible than D-MRA because it does not require fluoroscopy [14,15]. Independence from the radiologist skills needed for D-MRA and costs that are relatively similar to those of MRI are other advantages of I-MRA [13,16].
Diagnosing labral pathologies is a challenge for shoulder surgeons. The gold standard for imaging to diagnose such pathologies is D-MRA; however, given the problems with that method, some physicians have suggested using I-MRA. We conducted this study to compare the diagnostic value of MRI and I-MRA in distinguishing various labrum pathologies.
METHODS
The protocol for this study was approved by the Institutional Review Board of Guilan University of Medical Sciences (IRB No. 847). All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975 (in its most recently amended version). Informed consent was obtained from all patients included in the study.
Study Design
This prospective descriptive-analytical study was conducted in 2020 in our university orthopedic clinic. All patients older than 18 years clinically suspected to have a labral injury based on history and positive labral tests (apprehension, relocation, load and shift, inferior sulcus sign, and crank tests) were entered into the study. Informed consent was obtained from all the participants, and patients with a history of fracture or surgery in the involved shoulder, underlying disease (diabetes, hypothyroidism, or rheumatoid arthritis), degenerative joint disease in the shoulder, or unwillingness to participate in the study were excluded. All patients underwent conservative treatment (physiotherapy, anti-inflammatory drugs, and activity reduction) for 6 weeks. In the event of no response to conservative treatment, MRI and I-MRA imaging were conducted. Patients underwent arthroscopy (as the gold standard of diagnosis) to conclude a final diagnosis and treatment plan.
Data Collection
Initial information (age, sex, damaged side, and cause of damage) was collected at the first visit and recorded on a data collection form. Anonymous MRI and I-MRA images were evaluated by an experienced radiologist at a 1-week interval. The criteria used in this study to diagnose labral lesions were as follows. (1) Contrast material extending into the labral substance. (2) Irregular labral margin. (3) Linear signal intensity not parallel to the glenoid labrum. (4) High signal intensity posterior to the long head of the biceps tendon origin. (5) High signal intensity extending inferior to the 3 o’clock position. (6) Detachment of the glenoid labrum. The results of the radiologist and arthroscopy were recorded on the data collection form.
Magnetic Resonance Protocol
Imaging was performed using a 1.5 tesla GE scanner with a shoulder array coil. The slice thickness was 3 mm, inter slice gaps were 10%, and the field of view was 150 mm. The following standard MRI sequences of the shoulder were used: coronal, sagittal, and axial proton density fat suppression; sagittal T1; and coronal T1FS. Patients were given an intravenous injection of gadolinium at 0.2 mL/kg (up to 15 mL), and after a delay of 10–15 minutes, during which the joint was exercised, and post-contrast coronal and axial T1FS imaging was performed.
Surgical Technique
All surgeries were performed under general anesthesia in the beach-chair position by a specialist shoulder surgeon (MMK). Anterior, posterior, and superior labral tears were evaluated with an arthroscope. If a tear was observed, it was repaired using an anchor suture.
Statistical Analysis
Frequency and percentage were used for descriptive data (age, sex, damaged side, and cause of damage). The diagnostic indices of sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy, as well as the kappa agreement and confidence interval (CI), were used to compare the results of MRI imaging with those of I-MRA based on arthroscopy as the gold standard for diagnosing labral lesions. The significance level was set at p˂0.05. All data were analyzed using IBM SPSS ver. 20 (IBM Corp., Armonk, NY, USA).
RESULTS
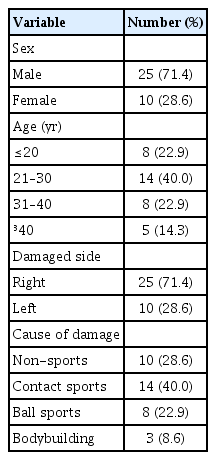
Of the 46 patients who met the inclusion criteria for the study, either responded to conservative treatment, and three were excluded because of follow-up unavailability. Thus, 35 patients did not respond to 6 weeks of conservative treatment and underwent MRI and I-MRA, followed by arthroscopy. The demographic characteristics of the patients are given in Table 1.
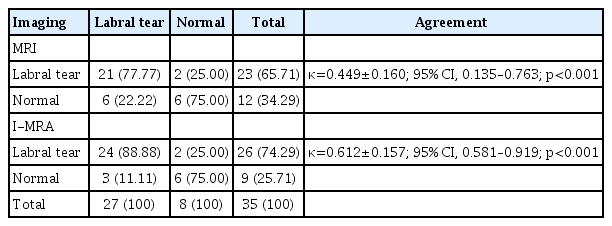
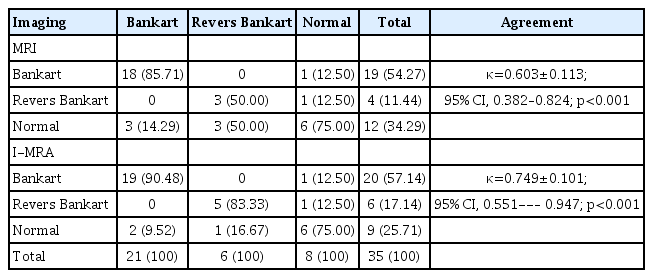
The arthroscopy results indicate that 27 patients had a labral tear (21 Bankart lesions, 6 reverse Bankart lesions), and eight patients had a normal labrum. According to the kappa test, MRI and I-MRA generally agreed with arthroscopy in diagnosing labral lesions, Bankart lesions, and reverse Bankart lesions. The two imaging methods did not differ significantly in the 95% CI kappa results (Tables 2 and 3). Moreover, no complications were seen after either type of imaging.
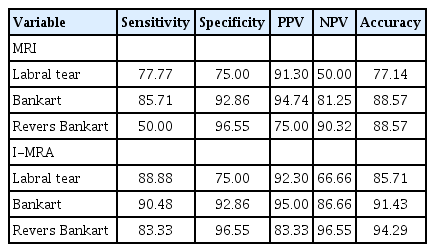
Table 4 shows the sensitivity, specificity, PPV, NPV, and accuracy of both imaging modalities. These measures for diagnosing labral lesions, Bankart lesions, and reverse Bankart lesions were higher for I-MRA than for MRI. The specificity of the two imaging modalities was similar.
DISCUSSION
Imaging is important in preoperative diagnosis of labral lesions because the clinical signs are often nonspecific. It is important for orthopedic surgeons to accurately describe the imaging outcomes of pathological labral abnormalities and use them to prevent unnecessary surgical treatments [17]. The main diagnostic imaging methods in these shoulder injuries are MRI, I-MRA, and D-MRA [17,18]. Most previous studies have compared the diagnostic value of MRI with that of D-MRA. We compared I-MRA and MRI with arthroscopy results as the gold standard of diagnosis.
In our study, 35 patients first underwent MRI and I-MRA, and those images were evaluated by a musculoskeletal radiologist at 1-week intervals and compared with the surgical outcomes. According to the kappa coefficient, the agreement between MRI and arthroscopy (0.449±0.160 and 0.603±0.113, respectively) was less than that between I-MRA and arthroscopy (0.612±0.157 and 0.749±0.101) in diagnosing labral tears and type of lesion. Although both diagnostic methods were in good agreement with arthroscopy, the agreement was better with I-MRA. Nonetheless, the difference between the two methods was not statistically significant because the 95% CI kappa ranges overlap.
Conventional MRI is a simple imaging technique whose images are useful in shoulder joint instability evaluations [19]. Conventional MRI with 3-T scanners has high accuracy in detecting SLAP lesions [5]. In this study, we used 1.5-T scanners, which are less accurate and sensitive than 3-T scanners. Phillips et al. [20] indicated that conventional MRI was not very accurate in diagnosing upper labrum tears. Unlike D-MRA, I-MRA is a non-invasive technique independent of radiologist skill and has lower costs and fewer complications [21]. Razzano et al. [21] indicated that I-MRA has sensitivity similar to that of D-MRA. According to the results of previous studies, I-MRA seems to be as useful as D-MRA in diagnosing labral lesions. Furthermore, I-MRA has fewer complications and is less costly for patients.
The sensitivity, specificity, NPV, PPV, and accuracy of MRI in detecting labral tears were 77.77%, 75.00%, 91.30%, 50.00%, and 77.14%, respectively, and the values for I-MRA were 88.88%, 75.00%, 92.30%, 66.66%, and 85.71%. Thus, it seems that I-MRA has greater diagnostic value than MRI. Fallahi et al. [22] found results similar to ours, with higher sensitivity (95% and 97% vs. 79% and 83%) and accuracy (93% and 95% vs. 84% and 86%) of I-MRA than MRI. Phillips et al. [20] indicated that the sensitivity and accuracy of D-MRA were higher than those of MRI, while the specificity was lower. Previous studies comparing the diagnostic value of these imaging modalities for SLAP lesions indicated that I-MRA has higher diagnostic value than MRI [22,23]. Apparently, the intravenous contrast injection and MR imaging of the shoulder used in the I-MRA method show labral tears more accurately than does conventional MRI. In other words, the presence of a contrast agent in the shoulder joint enhances the imaging sharpness of the joint cavity and surrounding structures and improves the diagnostic value for glenoid labral tears. Previous studies have indicated that I-MRA has a higher diagnostic value than MRI [24,25]. However, most of those studies were retrospective and had a small sample size. Neither method has any dangerous complications for patients.
Although this study was carried out prospectively, the small sample size is one of its limitations. The other limitations are exclusion of patients because of follow-up loss, poor quality of shoulder images due to the use of old devices, and interpretation of images by only one radiologist. Based on our results, more studies are suggested for comparing I-MRA with other imaging modalities in diagnosing labral lesions and other shoulder pathologies.
Compared with MRI, I-MRA seems to have higher diagnostic value for labral tears. Because the costs of I-MRA are similar to those of MRI and neither procedure has a high risk of complications, use of I-MRA instead of MRI is recommended when imaging is indicated for labral lesions.
Notes
Financial support
None.
Conflict of interest
None.