Botulinum toxin as adjunct therapy in surgical management of a periprosthetic scapular spine fracture: a case report
Article information
Abstract
Six months after undergoing reverse shoulder arthroplasty (RSA) a 73-year-old woman sustained a periprosthetic scapular spine fracture following a fall. She was treated with open reduction and internal fixation (ORIF), followed by botulinum toxin injection into the deltoid muscle to temporarily minimize strain at the fracture. Fracture union was achieved by 3 months, with excellent clinical function more than 1 year following fracture fixation and full resolution of deltoid function. Scapular spine fracture following RSA can be treated with ORIF and temporary deltoid paralysis using botulinum toxin in the immediate postoperative period to safely support fracture healing.
Level of evidence: V.
Scapular spine fractures are known complications of reverse shoulder arthroplasty (RSA), with an estimated incidence of 0.8%–1.3% of all RSA procedures [1,2]. Treatment of these fractures, however, is difficult. Limited series suggest high nonunion rates and poor function for conservative treatment strategies [2]. Nonunion is thought to result, in part, from the deforming forces imposed by the deltoid along the scapular spine [3]. Periprosthetic scapular spine fractures can be treated with open reduction and internal fixation (ORIF); however, the clinical results to date have been marginal. The distraction force of the deltoid muscle even after ORIF poses a challenge for fracture healing [4]. We hypothesized that administration of botulinum toxin directly to the deltoid muscle as an adjunct therapy following ORIF can promote fracture healing by reducing its distraction force. Botulinum toxin has multiple clinical applications within orthopedics in the treatment of muscle spasticity and hypertonicity; however, little has been described pertaining to its use in the setting of fracture care [5]. To our knowledge, use of botulinum toxin in the management of periprosthetic scapular spine fractures has not been reported. This study was exempt from Institutional Review Board review. The patient in this report provided consent for her case to be submitted for publication.
CASE REPORT
A 73-year-old woman with osteoporosis and vitamin D deficiency presented with right end-stage glenohumeral osteoarthritis. She was indicated for shoulder arthroplasty after failed non-surgical treatment. Her physical exam was notable for 170° of forward flexion, 45° of external rotation, and internal rotation to the L5–S1 vertebral level. Preoperative imaging of the right shoulder demonstrated advanced glenohumeral joint osteoarthritis with bone-on-bone apposition and an inferior osteophyte on the humeral neck (Fig. 1). Computed tomography (CT) revealed a B2 glenoid deformity, 21º of glenoid retroversion, and 75% posterior subluxation of the humeral head (Fig. 2). The patient underwent uncomplicated RSA using the AltiVate Reverse prosthesis (DJO Global) and was discharged from the hospital on postoperative day 2 (Fig. 3).

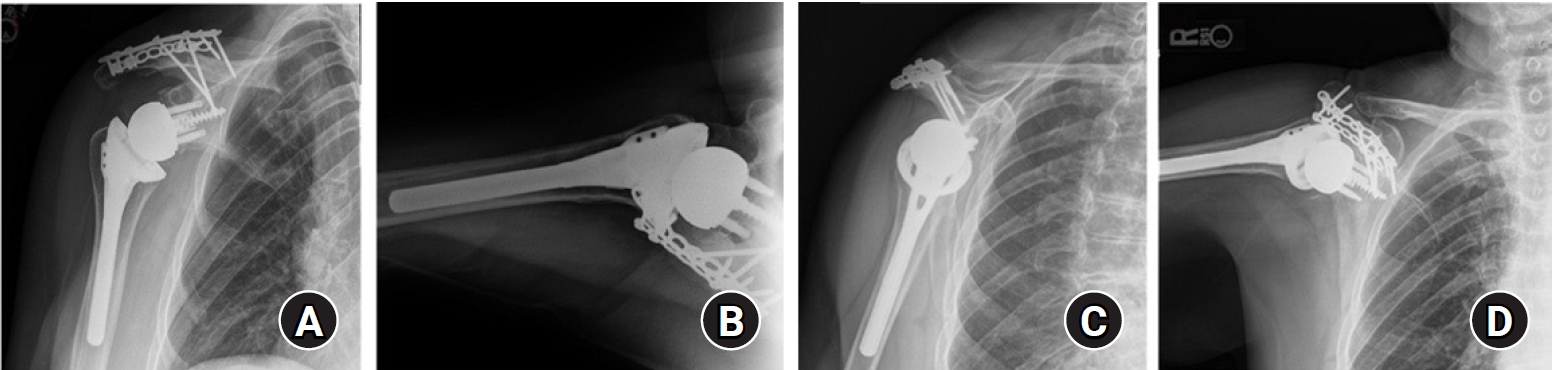
Preoperative anteroposterior (A) and axillary (B) X-rays of the right shoulder demonstrating significant glenohumeral osteoarthritis.
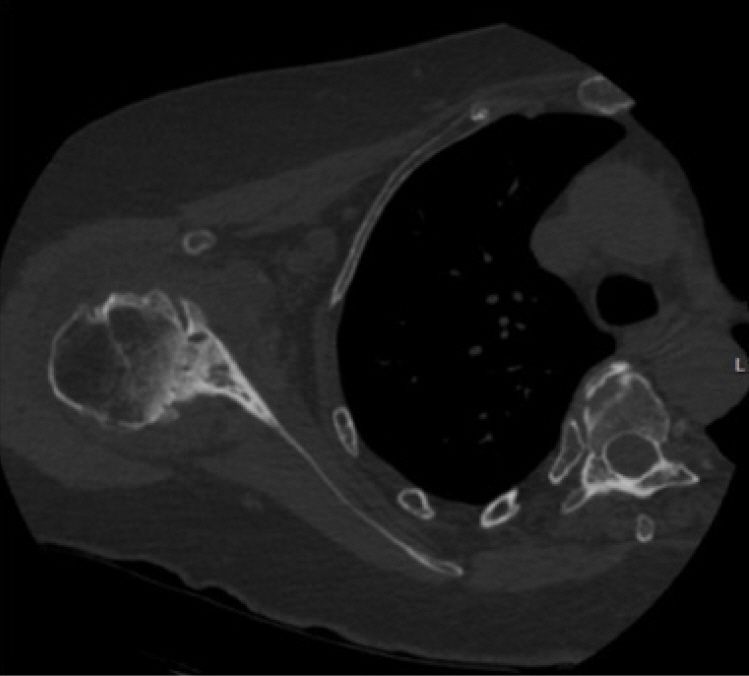
Axial computed tomography scan slice of the right shoulder demonstrating a Walch classification B2 glenoid deformity.
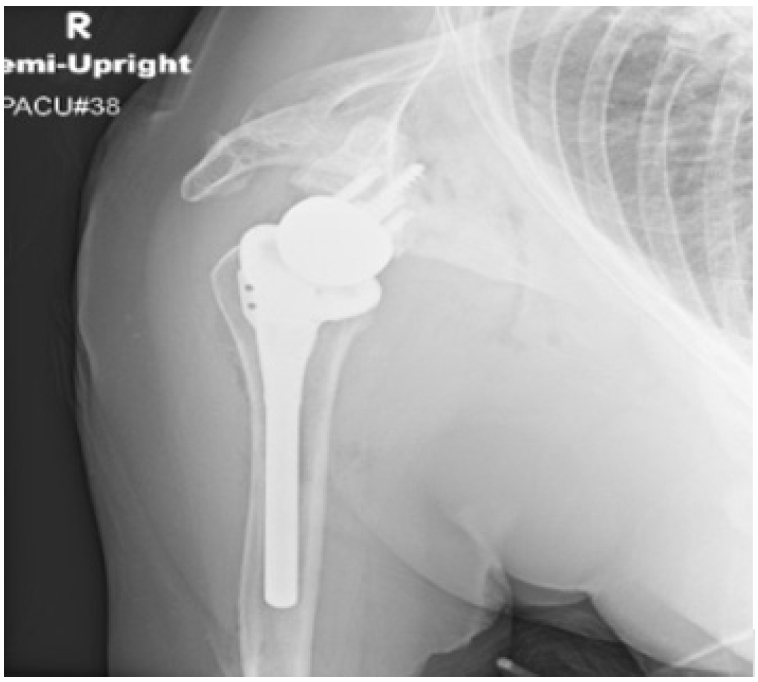
Immediate postoperative portable anteroposterior X-ray of the right shoulder obtained in the recovery room and demonstrating interval placement of an reverse shoulder arthroplasty prosthesis without evidence of fracture or dislocation.
The immediate postoperative course was unremarkable. At 6 months postoperative, she had 170º of forward elevation, 60º of external rotation, and internal rotation to the L1 vertebral level on the operative side with visual analog scale (VAS) pain score of 0/10. Twelve days after this office visit, the patient experienced a fall on her right shoulder while traveling internationally. Radiographs performed abroad suggested a scapular spine fracture, which was confirmed with repeat radiographs (Fig. 4) and CT scan (Fig. 5) upon return to the United States. Imaging demonstrated a Levy type 2 periprosthetic scapular spine fracture involving the acromion at the location of the entire middle deltoid attachment but not through the entire posterior deltoid attachment. There was one shaft-width anterior displacement of the spine of the scapula relative to the acromion with a mild degree of bayonet apposition. The patient’s physical exam was notable for ecchymosis; sensation intact to light touch over the upper lateral arm and radial, median, and ulnar distributions; a 2-plus radial pulse; 5-out-of-5 strength in the flexor pollicis longus, extensor pollicis longus, and interossei muscles; tenderness over the scapular spine; and gross mobility at the fracture site. The patient was indicated for fracture fixation. She was able to use all three heads of the deltoid against manual resistance but was pain limited.
Anteroposterior (A) and axillary (B) X-rays of the right shoulder demonstrating a periprosthetic scapular spine fracture 6 months after reverse shoulder arthroplasty.
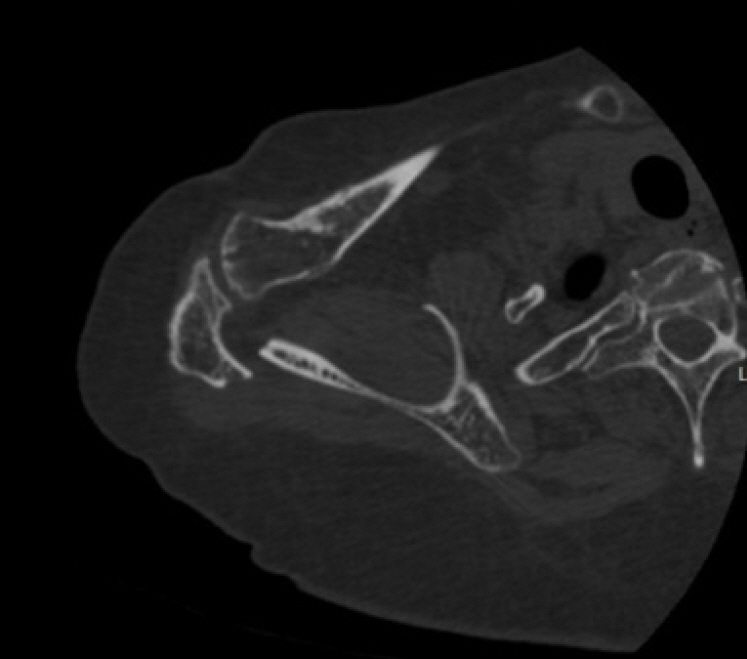
Axial computed tomography image of the right shoulder 6 months after reverse shoulder arthroplasty, demonstrating a displaced scapular spine fracture.
Surgical approach consisted of a transverse incision directly over the scapular spine to expose the fracture site. The scapular spine fracture was reduced anatomically and fixed using a 12-hole 2.7-mm reconstruction plate (Synthes) on the superior portion of the scapular spine and a 12-hole 2.4-mm plate on the posterior surface of the scapular spine. Postoperatively, the patient was placed in a shoulder immobilizer with an abduction pillow to prevent weightbearing, and allowed to perform passive range of motion about the shoulder in all planes. On postoperative day 3, the patient received a botulinum toxin injection into the ipsilateral right deltoid muscle to decrease shear forces across the fracture. Using sonographic guidance with sterile and local anesthetic technique a 22-gauge 3.5-inch needle was used to inject 8 units of botulinum toxin reconstituted in 3 mL of normal saline into each of the anterior, middle, and posterior deltoid muscle bellies. A total of 24 units of botulinum toxin was delivered into the deltoid muscle unit. The injection was delivered roughly half-way between the acromion origins and humeral insertions. The injection remained local and was not intended to affect the entire muscle. Though the appropriate dose of botulinum toxin in this setting has not been established, adequate paralysis was confirmed on clinical exam at the patient’s first follow-up appointment by inability to activate the deltoid muscle. Six weeks after scapular spine ORIF, the patient was healing well upon X-ray examination (Fig. 6) and able to maintain non-weightbearing of the right upper extremity without active range of motion. Her sling was discontinued, and she was advanced to 5-pound maximum lifting on the right side. At 2 months postoperatively, deltoid strength was recovering and noted as 4/5, the patient reported no pain and was assigned physical therapy to begin active range of motion. Seventeen months following periprosthetic fracture fixation, the patient had VAS pain score of 0/10 and excellent range of motion including forward elevation 170°, external rotation 60°, and internal rotation to T10 (Fig. 7). Radiographs demonstrated a well-fixed RSA prosthesis and union of the previous scapular spine fracture (Fig. 8). Deltoid function was noted as 5/5 for all three heads.
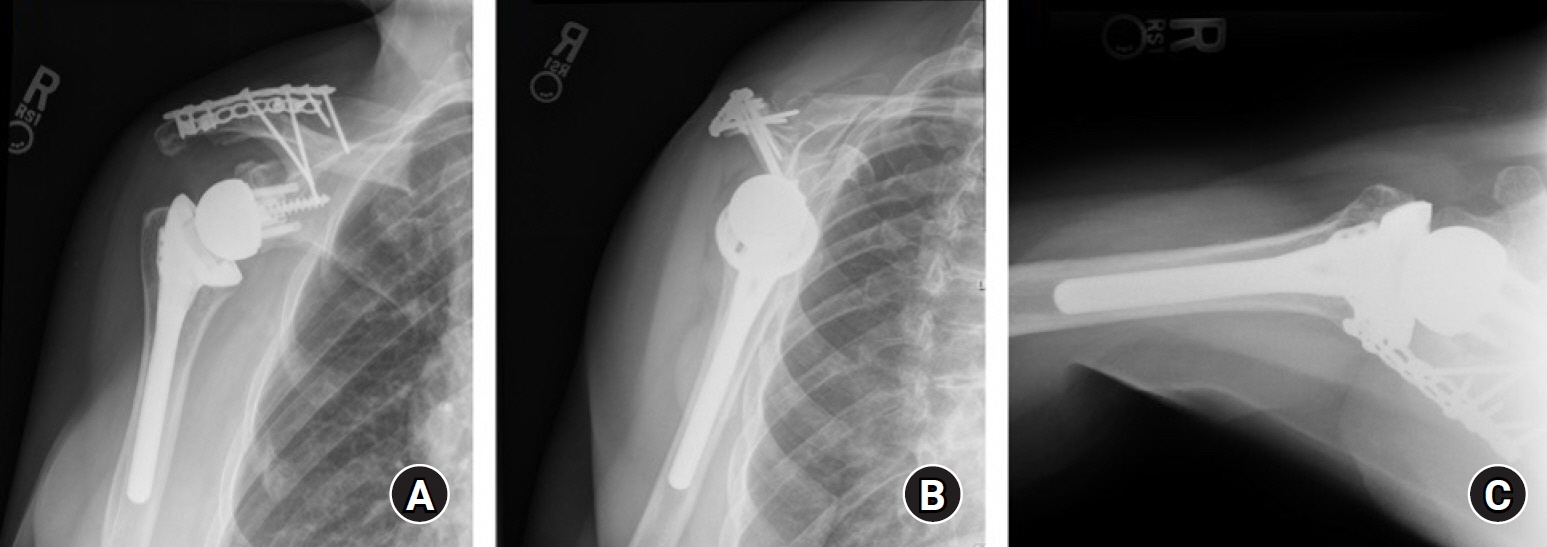
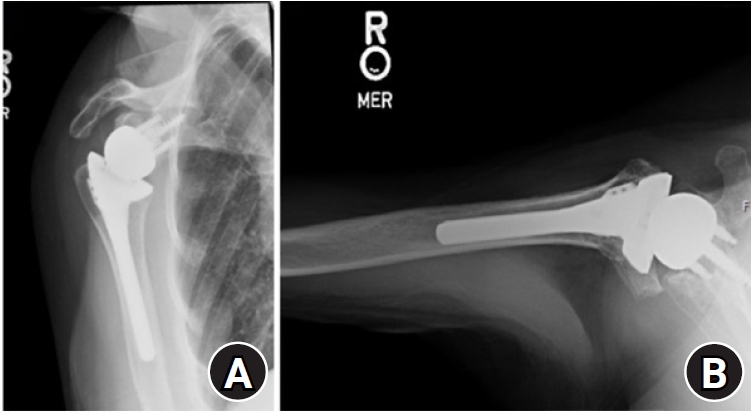
Anteroposterior (A), Y-scapular (B), and axillary (C) X-ray images obtained at the 2-month postoperative visit after open reduction and internal fixation of a periprosthetic scapular spine fracture and botulinum toxin injection.
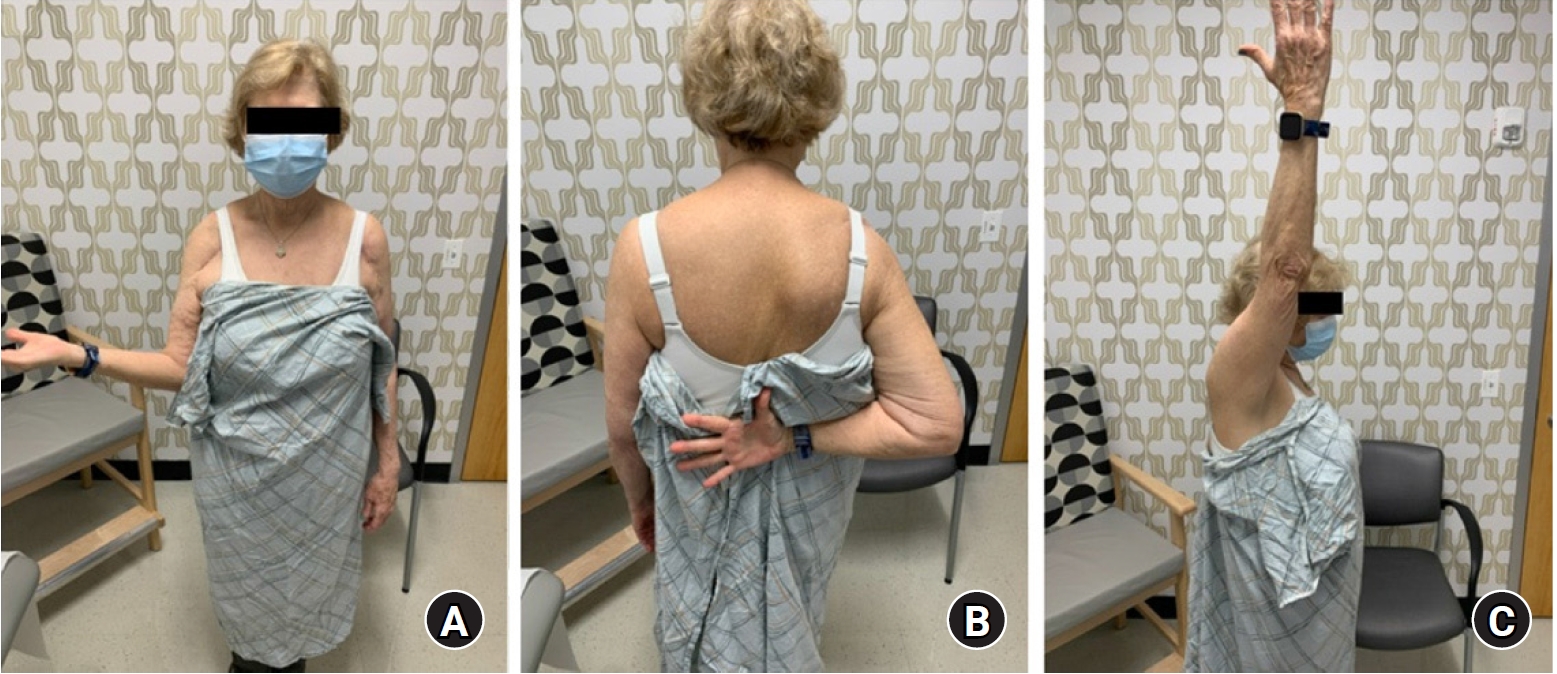
Clinical photographs at 17 months postoperatively from a right periprosthetic scapular spine fracture open reduction and internal fixation demonstrating 60º of external rotation (A), internal rotation to the T10 vertebral level (B), and 170º of forward flexion (C).
DISCUSSION
Since 2014, RSA has been performed more frequently than anatomic total shoulder arthroplasty in the general population, supported by impressive clinical results [6]. With a rise in procedural volume, the RSA-related complications will increase concomitantly. Periprosthetic scapular spine fractures are a relatively common complication producing underwhelming clinical outcomes regardless of treatment [7]. The etiology of these fractures is likely multifactorial. Poor bone quality, either osteopenia or osteoporosis, certainly contributes to these fractures, and successful use of teriparatide in this setting has been described [8]. An additional theorized etiology is that the deforming stresses imposed by the deltoid are magnified by medialization and distalization of the glenohumeral center of rotation during RSA; this lengthens the deltoid and increases the abductor moment arm for shoulder abduction [7,9]. Additionally, the coracoacromial ligament has been shown to be an important stabilizing structure of the scapular ring – its transection results in increased scapular spine strain after RSA [9]. For these biomechanical reasons, scapular spine fractures in the setting of RSA have proven difficult to heal, both after non-operative and surgical management.
The first medical indication for botulinum toxin use was for treatment of strabismus, although more than 30 medical uses have been described [10]. Botulinum toxin acts by cleaving the soluble N-ethylmaleimide-sensitive factor attachment protein receptor complex found at cholinergic nerve terminals. When this occurs in muscle tissue, acetylcholine vesicles cannot fuse to the cellular membrane, are unable to enter the neuromuscular synaptic junction, and paresis results [10]. The onset of paresis from botulinum toxin injection typically occurs 2 to 5 days after injection [10]. The duration of action of botulinum toxin A when administered directly into human skeletal muscle is approximately 3 to 4 months, though the half-life has proven difficult to study. Given the duration of action, a single injection was sufficient to support fracture healing. Known largely for its cosmetic application, botulinum toxin was first described in orthopedics in the early 1990s for treatment of spasticity in pediatric cerebral palsy. The literature has shown that use of botulinum toxin A in cerebral palsy is effective in temporarily improving spasticity, as well as fine and gross motor function [11].
In the presented case, botulinum toxin was used to aid fracture healing by theoretically decreasing shear forces at a rigid fracture construct. This technique has been described in experimental settings and select case series. In one instance, researchers studied orthognathic fracture healing with botulinum toxin A injection into the masseter muscle [12]. Compared to the no treatment group, those who received botulinum toxin A in their masseter muscle had significantly fewer plate fractures [12]. Similarly, an experimental study in rabbit mandibular fractures demonstrated significantly greater bone healing scores, bone volume-total volume values, and trabecular diameter values in the botulinum toxin A study group compared to a placebo group [13]. In another animal study, rat femur fractures experienced increased biomechanical and histopathologic healing when treated with botulinum toxin A compared to no treatment, though the fracture callus diameter was smaller [14]. In one of the few clinical case reports on the topic, a patient with an undefined tic disorder sustained clavicle fracture treated with surgical fixation and botulinum toxin A injection, ultimately allowing fracture union without complication [15]. Finally, a retrospective review by Freibott et al. [16] demonstrated the clinical utility of botulinum toxin injections in the treatment of post-traumatic elbow stiffness caused by heterotopic ossification. The results of these studies in addition to the presented case provide anecdotal evidence that botulinum toxin A can be of benefit in select orthopedic treatments. Though this is a relatively low-risk intervention, there are risks inherent to intramuscular injections and the botulinum toxin itself. In particular, diffusion or leakage of botulinum toxin into surrounding tissues, or rarely, into the systemic circulation can occur and cause adverse or unintended effects. Additionally, immunogenicity to botulinum toxin can render dosing ineffective.
Periprosthetic scapular spine and acromion fractures are challenging complications in the setting of RSA and can lead to inferior patient function and outcomes. In this case, the patient experienced a traumatic scapular spine fracture that was treated with surgical fixation and perioperative botulinum toxin injection into the deltoid muscle. The high risk for nonunion in this particular fracture prompted the use of botulinum toxin to reduce the forces imposed by the deltoid. While not appropriate for most fractures, botulinum toxin-induced muscle paralysis can be considered to optimize the strain environment around fractures at high risk for nonunion. Further basic science and clinical study are warranted to better characterize the effects of botulinum toxin on fracture healing.
Notes
Author contributions
Conceptualization: SAT.Data curation: AEW, CMB, DSW, SAT. Formal Analysis: AEW, CMB, DSW, SAT. Investigation: AEW, CMB, DSW, SAT. Methodology: AEW, CMB, DSW, SAT. Project administration: AEW, CMB, DSW, SAT. Resources: AEW, CMB, DSW, SAT. Software: AEW, CMB. Supervision: DSW, SAT. Visualization: DSW, SAT. Writing – original draft: AEW, CMB. Writing – review & editing: AEW, CMB, DSW, SAT.
Conflict of interest
None.
Funding
None.
Data availability
None.
Acknowledgments
None.