Ten technical aspects of baseplate fixation in reverse total shoulder arthroplasty for patients without glenoid bone loss: a systematic review
Article information
Abstract
The aim of this systematic review was to collect evidence on the following 10 technical aspects of glenoid baseplate fixation in reverse total shoulder arthroplasty (rTSA): screw insertion angles; screw orientation; screw quantity; screw length; screw type; baseplate tilt; baseplate position; baseplate version and rotation; baseplate design; and anatomical safe zones. Five literature libraries were searched for eligible clinical, cadaver, biomechanical, virtual planning, and finite element analysis studies. Studies including patients >16 years old in which at least one of the ten abovementioned technical aspects was assessed were suitable for analysis. We excluded studies of patients with: glenoid bone loss; bony increased offset-reversed shoulder arthroplasty; rTSA with bone grafts; and augmented baseplates. Quality assessment was performed for each included study. Sixty-two studies were included, of which 41 were experimental studies (13 cadaver, 10 virtual planning, 11 biomechanical, and 7 finite element studies) and 21 were clinical studies (12 retrospective cohorts and 9 case-control studies). Overall, the quality of included studies was moderate or high. The majority of studies agreed upon the use of a divergent screw fixation pattern, fixation with four screws (to reduce micromotions), and inferior positioning in neutral or anteversion. A general consensus was not reached on the other technical aspects. Most surgical aspects of baseplate fixation can be decided without affecting fixation strength. There is not a single strategy that provides the best outcome. Therefore, guidelines should cover multiple surgical options that can achieve adequate baseplate fixation.
INTRODUCTION
The worldwide incidence of reverse total shoulder arthroplasty (rTSA) has increased exponentially since the introduction of the first rTSA by Grammont et al. in 1987 [1-3]. Despite innovations in surgical technique and implant designs, rTSA-related complications occur in 19%–68% of patients [4-8]. The incidence of baseplate loosening following rTSA ranges from 1.2% to 11.7%, and it usually requires revision surgery [9-13]. Revision procedures following rTSA are associated with higher complication rates, worse functional outcomes, and decreased patient satisfaction compared to those of primary rTSA [13-16]. Therefore, it is important to prevent revision procedures in order to improve patient outcomes. However, achieving optimal glenoid baseplate fixation can be challenging. Several screw- and baseplate-related surgical fixation aspects, such as screw placement and baseplate characteristics, are believed to be critical for achieving optimal glenoid baseplate fixation.
Although various studies have assessed screw- and baseplate-related surgical fixation aspects in rTSA, there is still no consensus on how to achieve optimal glenoid-implant fixation in rTSA. Insight into optimizing glenoid-implant fixation in rTSA is important to reduce aseptic baseplate loosening requiring revision surgery, scapular notching, postoperative fractures, and suprascapular nerve (SSN) injury. Optimizing glenoid-implant fixation in rTSA may also improve patient outcomes. This review was performed with the goal of collecting the available evidence on the following ten technical aspects of baseplate fixation in rTSA: screw insertion angles; screw orientation; screw quantity; screw length; screw type; baseplate tilt; baseplate position; baseplate version and rotation; baseplate design; and anatomical safe zones.
METHODS
This systematic review process followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and was registered in the International Prospective Register of Systematic Reviews (identification number 245912) [17]. Ethical approval is not required for this type of study under Dutch law.
Search Strategy
The literature search was conducted in PubMed, Embase, Web of Science, Cochrane Central Library, and Emcare using a systematic search strategy (Supplementary Material 1) created by a librarian (JWS). The articles were selected from January 2000 to July 2022. The list of references was imported into EndNote (version X9) to remove duplicate articles. The references were subsequently exported to the web application Rayyan for study selection.
Study Selection
Three authors (RWAS, LAH, and RCB) independently screened the titles and abstracts before assessing the full texts for eligibility. Any discrepancies were resolved by discussion between the authors. Studies were included according to the following eligibility criteria: (1) inclusion of least three patients, all of whom were >16 years old; (2) analysis of at least one baseplate fixation aspect (screw insertion angle, screw orientation, screw quantity, screw length, screw type, baseplate tilt, baseplate position, baseplate version and rotation, anatomical safe zones) in rTSA; (3) data regarding clinical outcomes, biomechanical outcomes, and/or anatomical outcomes. We excluded studies of patients with: (1) glenoid bone loss (Walch type ≥B1); (2) bony increased offset-reversed shoulder arthroplasty; (3) rTSA with bone grafts; and (4) augmented baseplates. In addition, studies were excluded if the full text was unavailable, if data were not extractable or if it was any of the following study types: systematic review, meta-analysis, conference abstract, case report (defined as inclusion of less than three patients), expert opinion, or animal study. Finally, the reference lists of the retrieved articles were reviewed for additional articles (citation snowballing).
Critical Appraisal and Data Extraction
Methodological quality of the clinical and cadaver studies was appraised using the Critical Appraisal Skills Program (CASP) [18] and the Quality Appraisal for Cadaveric Studies (QUACS) checklists [19]. The CASP checklist was classified into low (<8 points) and high (≥8 points) levels of quality. The QUACS checklist was classified into poor (≤6 points), moderate (7–9 points), and good (≥10 points) levels of quality. Quality assessments, authors, year of publication, and data extraction of all included studies were independently extracted by three authors (RWAS, LAH, and RCB). Any discrepancies were resolved by discussion between the authors.
Statistical Analysis
Data was presented using descriptive statistics. Outcomes were not synthesized, as it was inappropriate to generate pooled effect sizes due to the between-study heterogeneity in methodology and outcomes. A brief summary of the reviewed material was presented after each section.
RESULTS
Literature Search
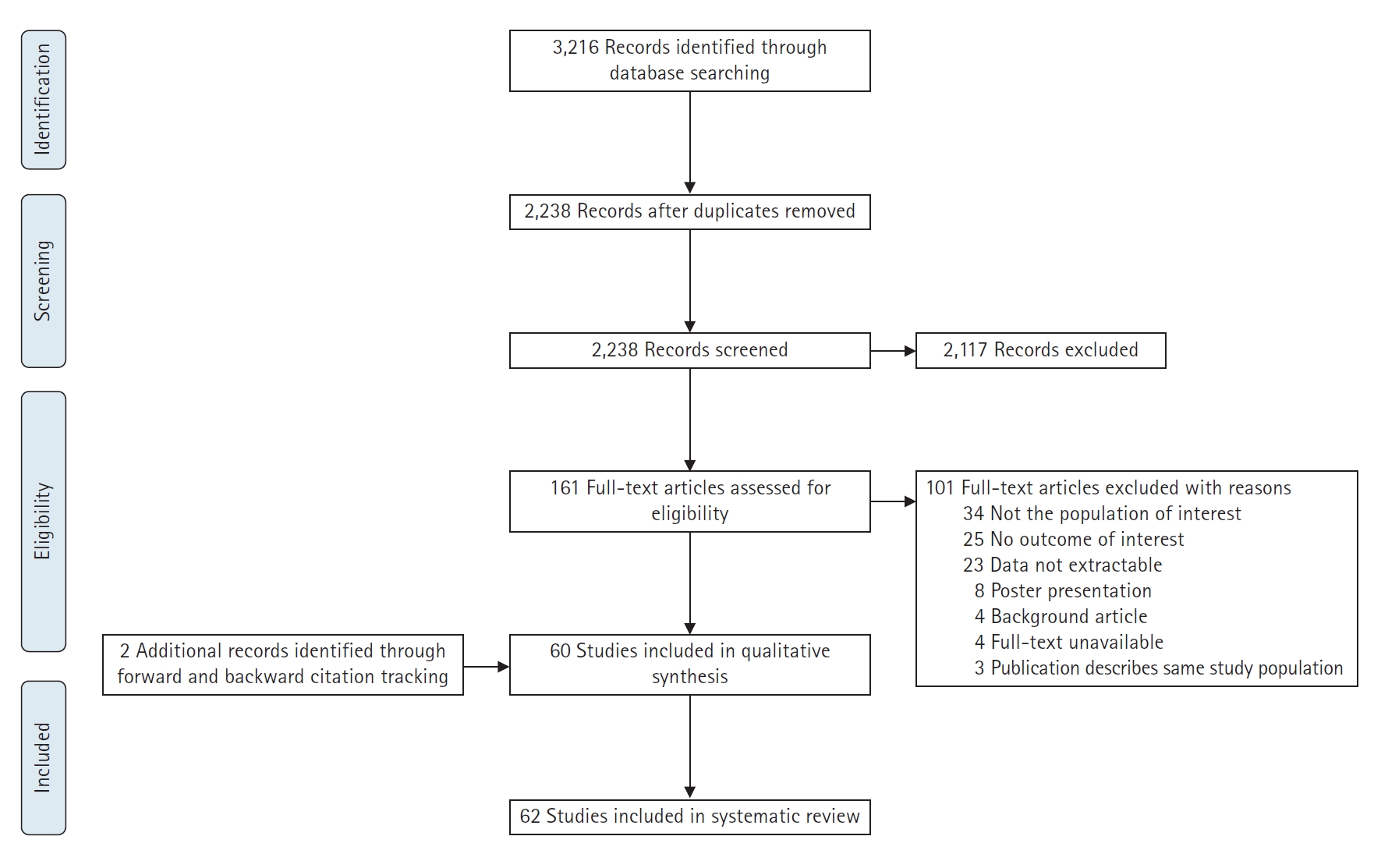
The literature search (Supplementary Material 1) identified 3,216 records. After removing duplicates, the titles and abstracts of 2,238 articles were screened. Thereafter, 161 full texts were assessed. Of these, 60 studies fulfilled the inclusion criteria. Another two studies were identified by reference checking; therefore, a total of 62 studies were included in the quality assessment (Fig. 1). The quality of clinical studies was low in 5 and high in 16 studies (Supplementary Material 2). The quality of cadaver studies was poor in zero, moderate in nine, and good in four studies (Supplementary Material 3). As zero studies were excluded after quality assessment, all 62 studies were suitable for analysis, including: 41 experimental studies (13 cadaver, 10 virtual planning, 11 biomechanical, and 7 finite element studies) and 21 clinical studies (12 retrospective cohort and 9 case-control studies).
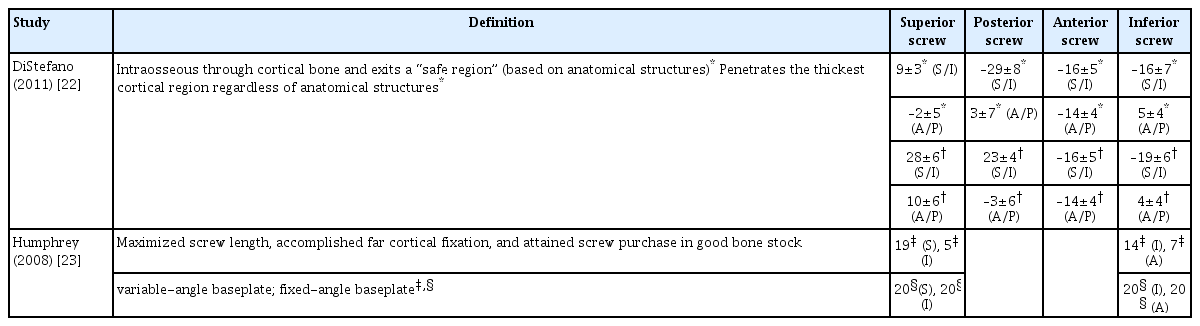
Screw Insertion Angle
A finite element study in which four different diverging screw insertion angles (0°, 10°, 20°, and 30°) were tested showed that an increasing screw insertion angle resulted in reductions in the baseplate micromotions: 90–110 µm (screw insertion angle of 0°) and 48–59 µm (screw insertion angle of 30°) [20]. Meanwhile, a finite element study in which five different screw insertion angles (0°, 10°, 17°, 15°, and 34°) were analyzed showed that screw insertion angles of 17° provided the most optimal stress distribution on the humeral spacer [21]. A virtual planning study determined the optimal screw insertion angle according to two scenarios, as follows: (1) entire intraosseous screw trajectory, exiting in a “safe anatomical region” (i.e., avoiding injury to the SSN, which runs between the 2- and 8-o’clock positions with the right shoulder as reference); (2) in-out-in screw trajectory with penetration in the thickest cortical region regardless of anatomical structures [22]. The optimal screw insertion angles, according to this study, are summarized in Table 1. Additionally, because there are no important neurovascular structures located at the inferior scapular pillar, the authors emphasized that inferior screws should be angled into the inferior scapular pillar. The angles of the posterior and superior screws highly depend on surgeons’ preferences. For instance, superior screws could be directed laterally or inferiorly to the suprascapular notch, whereas posterior screws could be angled toward the lateral scapular spine area or to thin cortical areas (provided that the length is short). Compared with scenario 2, similar screw insertion angles for the inferior screws were found in a cadaver study (n=10), in which variable and fixed baseplates were used (Tables 1 and 2) [23]. To summarize, there were considerable differences in optimal screw insertion angles described in these experimental studies.
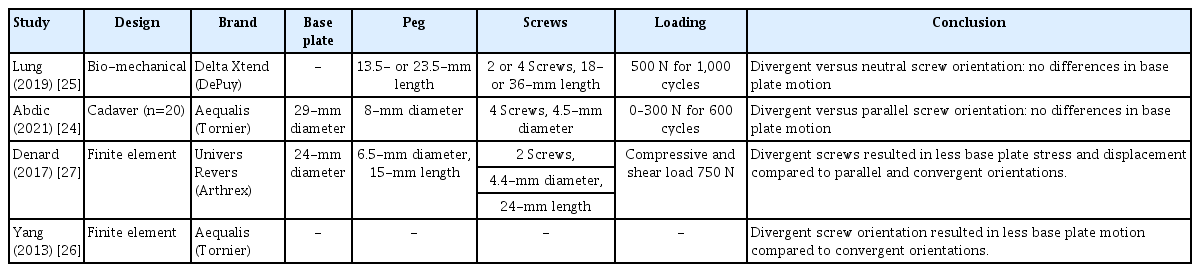
Screw Orientation
A cadaver study (n=20) reported no significant differences in baseplate micromotions measured by axial eccentric loading (0–300 N for 600 cycles) between the baseplates secured with divergent or parallel oriented screws (2.0 µm, standard error: 0.7 vs. 4.0 µm, standard error: 1.5, respectively) [24]. Additionally, a biomechanical study using cycling loading (500 N for 1,000 cycles) observed no significant differences in baseplate micromotions among baseplates secured with neutral or divergent oriented screws, as follows: inferior 247±22 and 193±23 µm; superior 121±17 and 108±18 µm; anterior 180±16 and 153±17 µm; posterior 188±22 and 148±23 µm [25]. Contrarily, a finite element study showed that baseplates secured with divergent oriented screws demonstrated less baseplate micromotions than did those secured with convergent oriented screws [26]. Likewise, another finite element study using compressive and shear load of 750 N demonstrated that divergent oriented screw fixation resulted in less baseplate stress and displacement than did baseplates secured with convergent or parallel oriented screws (Table 3) [27].
In summary, two out of four experimental studies suggested that baseplates should be secured with divergent oriented screws. In contrast, two experimental studies found no differences in baseplates micromotions while using different screw orientations.
Screw Quantity
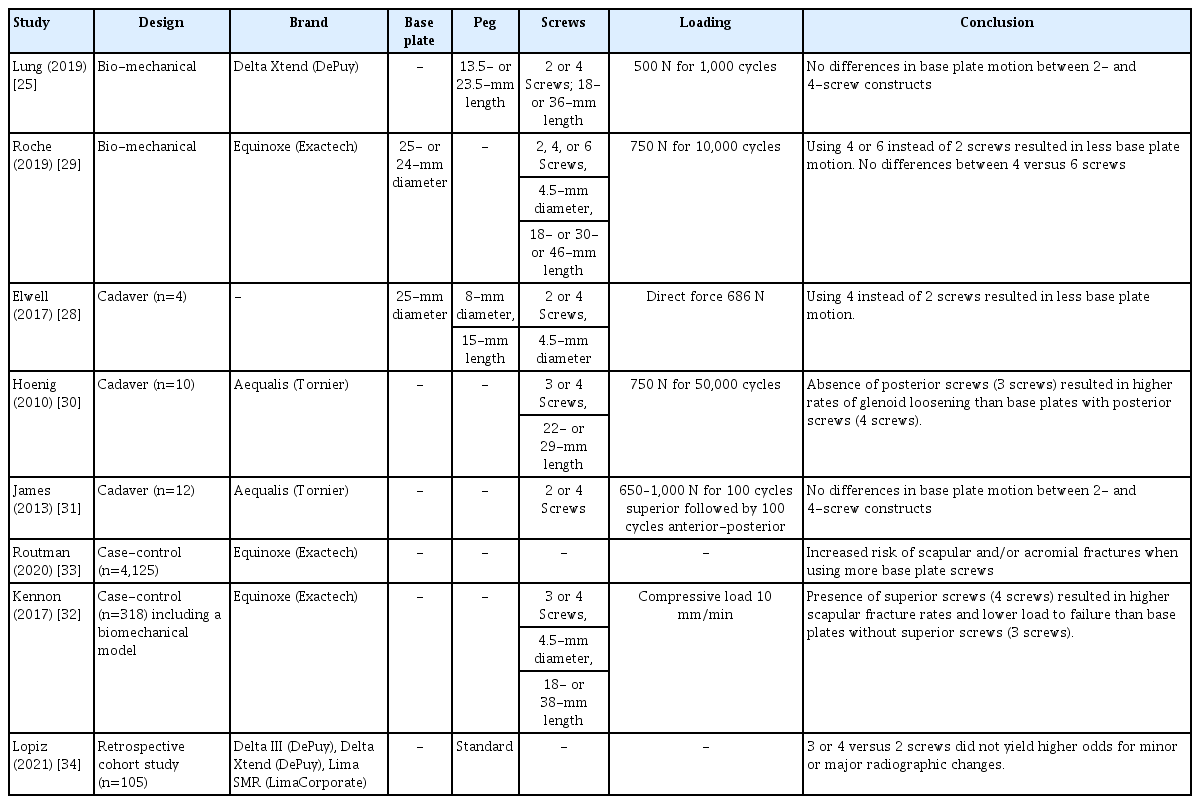
A cadaver study (n=4) reported reduced baseplate micromotions among baseplates secured with four screws when compared to those secured with two screws (18.3±5.9 vs. 35.0±14.9 µm; P=0.01, respectively) [28]. Additionally, a biomechanical study in which baseplates were constructed with two, four, or six screws reported more displacement both pre- and post-cyclic loading (750 N for 10,000 cycles) in baseplates secured with two screws than in baseplates secured with four or six screws (two screws 116±36 and 125±44 µm; four screws 82±22 and 91±23 µm; six screws 92±20 and 108±42 µm, pre- and post-cyclic loading, respectively). However, no differences were observed between four versus six screws (P=0.18 and P=0.18, pre- and post-cyclic loading, respectively) [29]. Furthermore, a cadaver study (n=10) analyzed the added value of the posterior screw by measuring the amount of vertical displacement of the glenoid component during cyclic loading (750 N for 50,000 cycles); this group found a three-fold higher rate of glenoid loosening in baseplates without posterior screws compared to those with posterior screws [30]. Contrarily, no significant differences in baseplate displacement were identified in another cadaver study (n=12) using cycling loading (650–1,000 N for 100 cycles in superior directions followed by 100 cycles in anterior-posterior directions). This group was primarily looking for mean differences in displacements between two and four screws constructs of: anterior 42 µm; posterior 41 µm; superior 13 µm; and inferior 14 µm [31]. Similar outcomes were reported in a biomechanical study using cyclic loading of 500 N for 1,000 cycles. This group found mean displacements between two and four screws, respectively, as follows: inferior 235±23 and 205±22 µm; superior 130±18 and 99±17 µm; anterior 180±16 and 155±16 µm; posterior 187±23 and 149±22 µm [25].
A case-control study (n=3,180) including a biomechanical model using compressive loading (10 mm/min) reported that superior screw insertion within four-screw constructs was associated with: a higher incidence of scapula body fractures (4.4% vs. 0.0%, superior screws yes/no, respectively); and a lower load to failure (1,077 N vs. 1,970 N, superior screws yes/no, respectively) [32]. Similar findings were reported in a case-control study (n=4,125) with a minimum follow-up of 2 years. In this study, patients with acromial and/or scapular spine fractures had more baseplate screws than did those without fractures (4.05±0.51 vs. 3.83±0.79, respectively; P=0.02) [33]. In contrast, another retrospective study (n=105) showed that utilizing three or four screws (vs. only two screws) did not increase the odds of minor or major radiographic changes (Table 4) [34].
To summarize, three out of five experimental studies demonstrated that baseplates should be secured with four screws. However, two out of three clinical studies reported higher occurrences of scapular and/or acromial fractures as the number of baseplate screws increases.
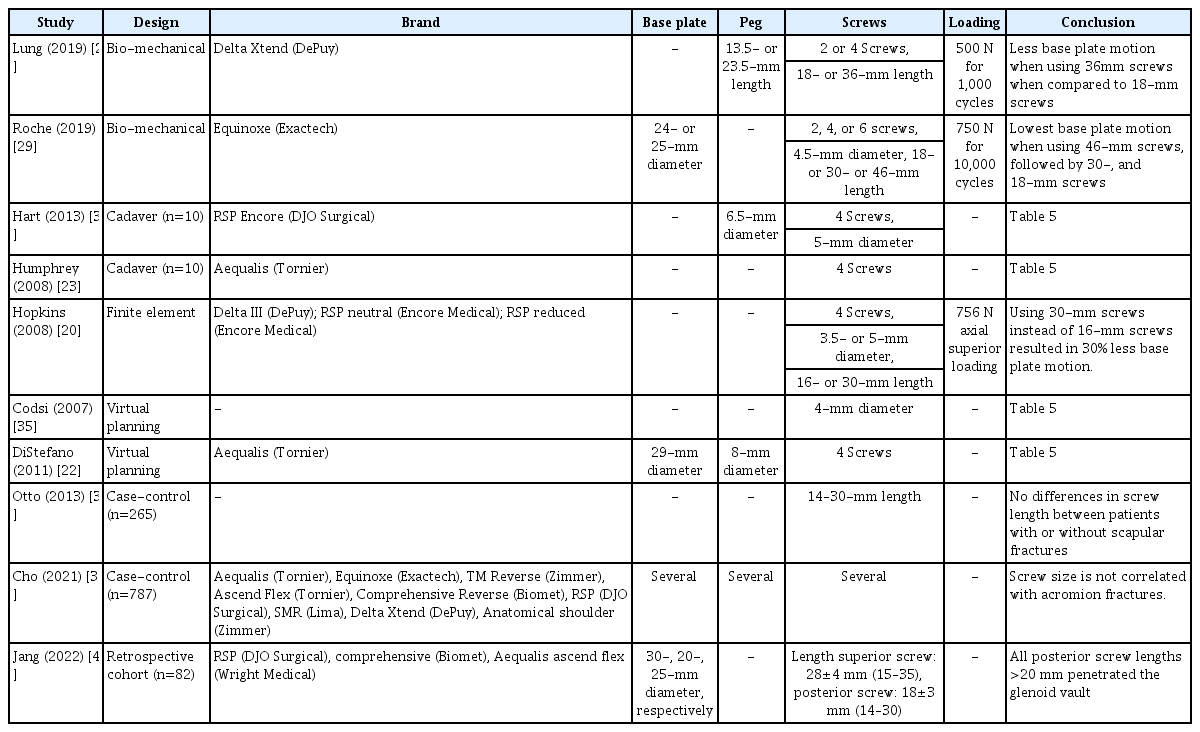
Screw Length
Five experimental studies analyzed the optimal screw lengths based on anatomical structures and/or maximum cortical fixation (Table 5) [22,23,35,36]. A finite element analysis study reported a 30% reduction rate in the baseplate micromotion using 30-mm instead of 16-mm screws [20]. Likewise, a biomechanical study reported lower baseplate micromotions after cycling loading (500 N for 1,000 cycles) among baseplates secured with 36-mm compared to 18-mm screws. This group described mean displacements with 36-mm vs. 18-mm screws, respectively, as follows: inferior 258±23 and 182±22 µm; superior 114±18 and 115±17 µm; anterior 190±17 and 143±16 µm; posterior 182±23 and 154±22 µm [25]. Additionally, a biomechanical study observed that the lowest baseplate displacements (both pre- and post-cyclic loading 750 N for 10,000 cycles) occurred in baseplates secured with 46-mm screws, followed by baseplates secured with 30- and 18-mm screws (46-mm screws: 74±15 and 73±8 µm; 30-mm screws: 101±12 and 111±16 µm; 18-mm screws: 115±39 and 140±45 µm, pre- and post-cyclic loading, respectively) [29]. The last cadaver study (n=7) described the use of long screws and showed that outside-in screws, as well as long screws, are risk factors for scapular fractures [37].
A case-control study reported no significant differences in the screw length of posterior and superior screws between patients with (n=53) or without (n=212) scapular spine fractures (23 vs. 22 mm, respectively) [38]. Similarly, a case-control study assessed the relationship between increasing screw length and the occurrence of acromial fractures, but did not find an association [39]. Additionally, a retrospective cohort study (n=82) assessed the incidence of glenoid penetration and found that all posterior screws with a length >20 mm (n=82) penetrated the glenoid vault (Table 6) [40].
Taken together, seven experimental studies reported benefits of fixating the baseplates with screws that are at least 30 mm in length. Two clinical studies reported no significant differences in screw length between patients with or without scapular fractures. One clinical study strongly advised against using >20 mm posterior screws.
Screw Type
The authors of a biomechanical study suggested using at least two locking screws, because they require a higher load to failure (2,153±115 N) compared to constructs with four non-locking screws (1,832±35 N) (P<0.01) [41]. Another biomechanical study demonstrated that baseplates secured with four locking screws had less baseplate micromotion than did those secured with four non-locking screws (P=0.02) [42]. Contrarily, another biomechanical study tested four screw combinations (1 locking screw vs. 3 non-locking screws, 2 vs. 2, 3 vs. 1, and 4 vs. 0) using cyclic loading (750 N for 10,000 cycles). This group reported no significant differences in baseplate micromotions after cycling loading between the following combinations (reported with their mean micromotions): 1 locking screw (97.1±47.2 µm); 2 locking screws (76.7±34.5 µm); 3 locking screws (72.4±15.3 µm); 4 locking screws (68.1±15.3 µm) [43]. Another biomechanical study analyzed the use of locking versus non-locking screws from another perspective. These authors concluded that if the central element punctured well into the cortical bone, non-locking anterior and posterior screws were sufficient. On the contrary, if the central element was too short, the anterior-posterior screws were required to have a locking function [44]. Furthermore, a cadaver study (n=10) compared the position of locking screws (superior-inferior locking screws with anterior-posterior compression screws versus anterior-posterior locking screws with superior-inferior compression screws) and found no difference in micromotion between these different positions (Table 7) [25].
In summary, two out of four biomechanical studies recommended securing baseplates with at least two locking screws. One biomechanical study showed that locking screws were particularly important if the central peg did not puncture into the cortical bone. The cadaver study demonstrated that the position of the locking screws does not improve the fixation strength.
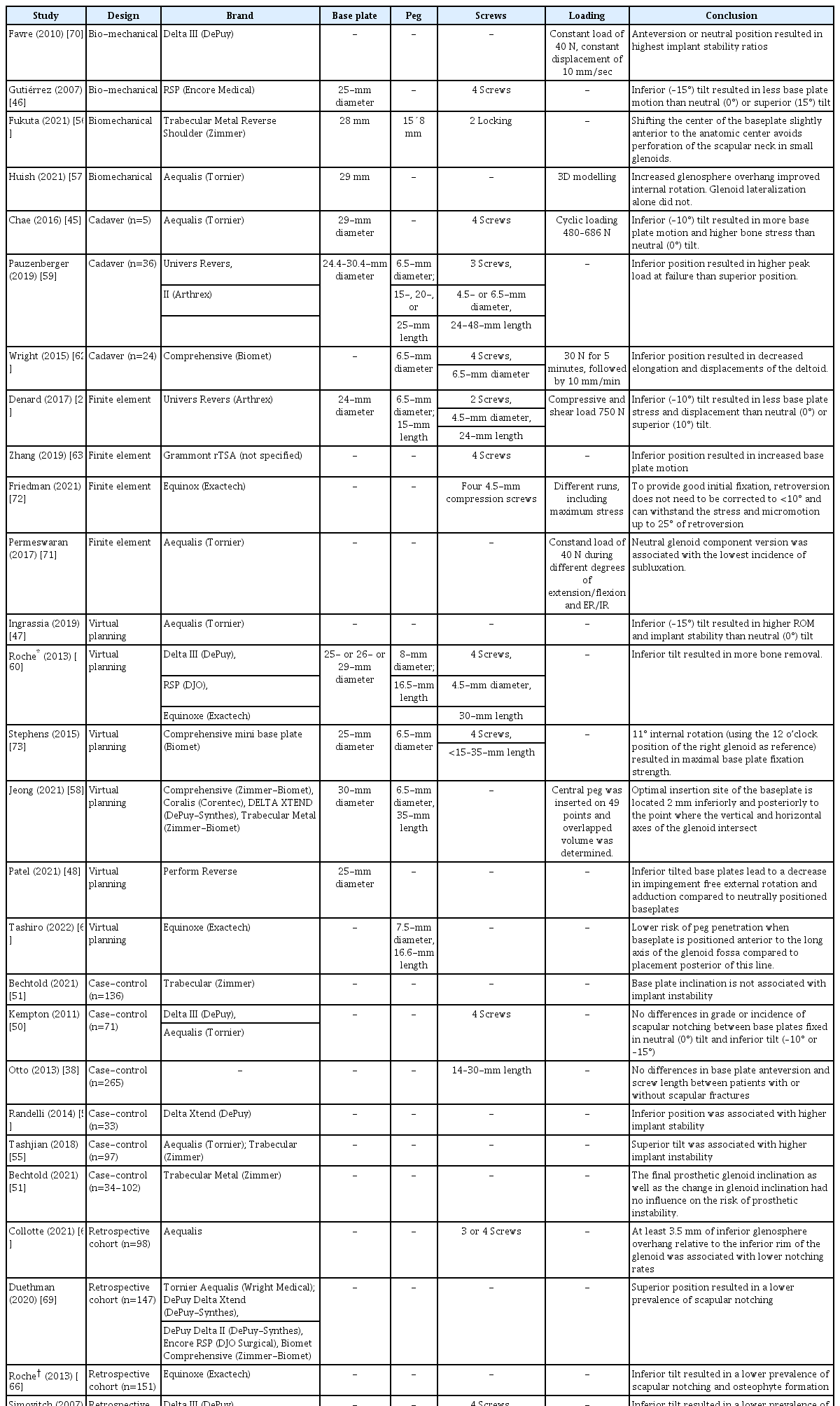
Baseplate Tilt
Previous experimental studies that described the relationship between tilt and baseplate stress and impingement are contradicting [27,45-48]. A retrospective cohort (n=146) with a mean follow-up of 21 months reported that scapular notching significantly decreased when an inferior tilt was used. However, baseplate tilt angles did not affect the range of motion (ROM) or functional-, pain-, and satisfaction-scores [49]. Furthermore, another retrospective cohort (n=71) found no differences in the grade or incidence of scapular notching at a minimum of 12 months of follow-up between baseplates secured in neutral (0°) and inferior (–10° or –15°) tilt: 76.7% vs. 60.7%, respectively (P=0.08) [50]. Additionally, a case-control study (n=136) concluded that baseplate inclination was not related to the likelihood of developing implant instability [51]. A retrospective cohort (n=105) reported that superior tilt was associated with increased risks of scapular notching and signs of loosening (odds ratio [OR]: 2.52 and OR: 8.92, respectively) [34]. However, another retrospective study (n=154) described no significant difference in postoperative ROM, patient-reported outcomes (PROMS), scapular notching, and heterotopic ossification between inferior, neutral, and superior (up to 6°) glenoid baseplate inclination [52]. Comparable results were described in a retrospective case-control study (cases=34 and controls=102); the final prosthetic glenoid inclination, as well as the change in glenoid inclination, had no influence on the risk of prosthetic instability [51]. Additionally, a cohort study (n=61) concluded that glenoid inclination had no significant influence on clinical outcomes at a minimum follow-up of 2 years [53]. Contrarily, another case-control study (n=33) reported an association between baseplate tilt and implant stability, as follows: –10.2° tilt in stable versus 8.3° in unstable implants (P=0.01) [54]. Likewise, another case-control study (n=97) reported a 13% instability rate at a mean follow-up of 47 months, and the only factor found to be associated with it was superior tilt: OR: 1.15, P=0.01) (Table 8) [55].
To summarize, the evidence is inconclusive to formulate guidelines with regard to baseplate tilt. Nevertheless, all prior studies have recommended against superior tilt.
Baseplate Position
Despite contradictory results, most experimental studies preferred an inferior position of the baseplate to increase the peak load failure and improve rotation [56-63]. A retrospective cohort study (n=54) showed that patients with scapular notching had higher positioned baseplates (as measured from the baseplate’s inferior aspect to the inferior rim of the glenoid) than did those without scapular notching (2.8±3.3 vs. 0.6±2.0 mm, P=0.03, respectively) [64]. Another retrospective cohort study (n=77) demonstrated that patients with inferior notching had higher peg-glenoid rim distances than did those without inferior notching (24.7±3.0 vs. 20.1±2.5 mm, P<0.001, respectively) [65]. Furthermore, a retrospective cohort (n=151) concluded that patients with scapular notching and/or osteophyte formation had higher positioned baseplates than did those without either scapular notching or osteophyte formation (20.3 vs. 19.1 mm, respectively) [66]. Moreover, a cohort study reported significantly longer peg glenoid rim distances and shorter sphere bone overhang distances in 13 patients with scapular notching as compared to 58 patients without scapular notching (24.8±1.6 and 2.6±0.5 mm vs. 21.9±1.9 and 5.8±1.9 mm, respectively). However, no significant differences were found in shoulder function and active ROM between the two patient groups at the last follow-up (37.0±3 months) [67]. A retrospective review (n=105) with a minimum follow-up time of 5 years found an increased risk of severe scapular notching that was mainly associated with a high (the glenosphere grazed the inferior edge of the glenoid, OR: 2.68) or excessively high (the glenosphere was beyond the inferior edge of the glenoid, OR: 7.55) position [34]. A retrospective cohort (n=97) analyzing glenoid components with ≥3.5 mm of inferior overhang versus flush glenoid components described a significantly lower rate of radiographic notching (37% vs. 82.5%, respectively), better clinical outcomes, and higher subjective shoulder value if the glenoid component had at least 3.5mm of inferior overhang as compared to a flush glenoid component [68]. Contrarily, another retrospective cohort (n=147) concluded that inferior positioned baseplates were associated with increased rates of scapular notching. However, baseplate positions were not associated with the incidence of revision surgery (28.9 vs. 25.2 mm, P=0.17, revision yes/no, respectively) (Table 8) [69]. In summary, the majority of the experimental and clinical studies reported benefits of fixating baseplates inferiorly.
Baseplate Version and Rotation
A biomechanical study analyzed the differences between five different glenosphere positions (20° retroversion, 10° retroversion, neutral position, 10° anteversion, and 20° anteversion) on implant stability and concluded that baseplates should be secured in anteversion or a neutral position to attain the highest stability ratio [70]. A finite element analysis showed that a neutral glenoid component produced the greatest impingement-free ROM, as compared to 5° anteversion and 5°, 10°, and 20° retroversion [71].
A case-control study (including patients with scapular spine fractures (n=53) and controls without scapular spine fractures (n=212), reported no significant differences in baseplate anteversion between the two groups [38]. The baseplate was anteverted in 20% of the cases and in 17.6% of the controls [38]. According to a finite element analysis model, the baseplate retroversion does not need to be corrected to <10° to provide good initial fixation. Instead, it can withstand the initial stresses and micromotion up to 25° of retroversion (Table 8) [72]. A virtual planning study was the only study to examine the influence of internal baseplate rotation; the group reported that 11° of internal rotation from the 12 o’clock position resulted in the strongest superior screw fixation [73].
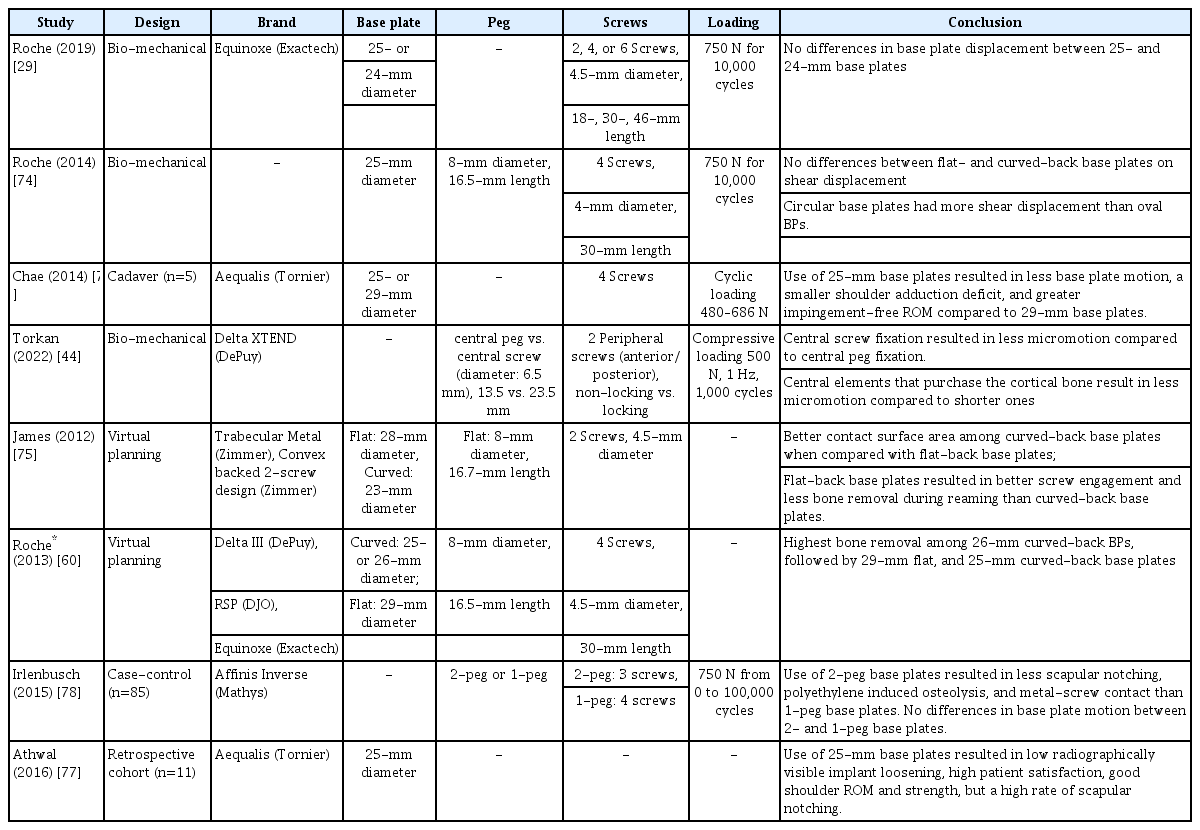
Baseplate Design
Curved back or flat back?
A biomechanical study reported no differences in shear displacement both pre- and post-cycling loading (750 N for 10,000 cycles) between curved-back and flat-back baseplates [74]. However, a virtual planning study showed better bone contact surface area in curved-back baseplates when compared to flat-back baseplates (P=0.01) despite the fact that flat-back implants had better screw puncture and less bone removal during fixation than did curved-back baseplates (P=0.03 and P=0.01, respectively) [75]. Another virtual planning study analyzed the amount of bone removed during reaming in three different baseplate designs (two curved-back and one flat-back baseplates). This group reported that the amount of bone removal was the highest among 26-mm curved-back baseplates, followed by 29-mm flat-back and 25-mm curved-back baseplates (Table 9) [60].
Circular or oval?
Only one study examined the outcomes of circular versus oval baseplates. This biomechanical study showed that circular baseplates had more shear displacement in both the superior-inferior and anterior-posterior directions both pre- and post-cyclic loading (750 N for 10,000 cycles) than did oval baseplates (Table 9) [73].
The smaller the better?
A cadaver study (n=5) demonstrated that 25-mm baseplates, when compared to 29-mm baseplates, resulted in less baseplate micromotion at the inferior third of the glenoid-glenosphere interface, a smaller shoulder adduction deficit, and a greater impingement-free ROM [76]. However, no differences in baseplate displacement between 25- and 24-mm baseplates were found in a biomechanical study using cyclic loading (750 N for 10,000 cycles) [29].
One retrospective cohort (n=11) analyzed the outcomes of a 25-mm baseplate in a cohort of relatively short patients (mean length: female, 156±8 cm; male, 171±2 cm). Despite a high rate of scapular notching (82%), outcomes at 3 years of follow-up were successful, including: no revision procedures, no radiographic evidence of implant loosening and acceptable ROM, PROMs, and strength (Table 9) [78].
In summary, one cadaver study reported superior outcomes of 25-mm and 29-mm baseplates, whereas one biomechanical study found no differences in baseplate displacement between 25- and 24-mm baseplates. One retrospective cohort demonstrated acceptable outcomes of 25-mm baseplates.
The 2- or 1-peg design?
A case-control study (n=85) in which 2- and 1-peg baseplates were compared reported a lower rate of scapular notching, polyethylene induces osteolysis, and metal screw contact when using 2-peg baseplates [77]. However, the amount of baseplate micromotion following cyclic loading (750 N from 0–100,000 cycles) did not differ between the two constructs (47 and 43 µm, 2- and 1-peg baseplates, respectively).
Central peg of central screw fixation?
A biomechanical study concluded that central screw fixation resulted in less baseplate micromotion than did central peg fixation. Also, the central elements that puncture the cortical bone result in less micromotion than do the shorter ones, which do not reach the cortex [44].
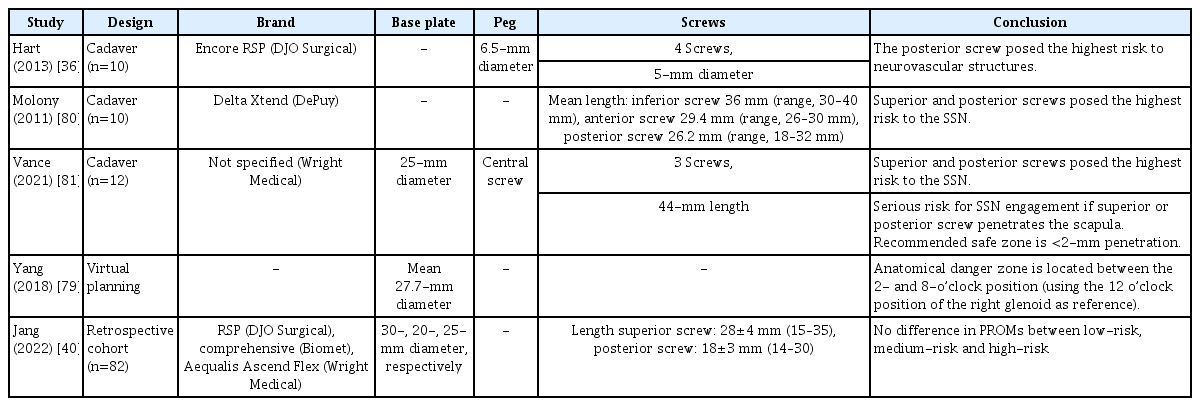
Anatomical Safe Zones
A virtual planning study (n=56) described a danger zone to assist surgeons to avoid SSN injury and revealed that the danger zone of the superior screw was located between the 2- and 8-o’clock positions (using the 12 o’clock position of the right glenoid as reference) [79]. The posterior screw touched the neurovascular structures in 33% of specimens in a cadaver study (n=10) [36]. Additionally, another cadaver study (n=10) showed that the superior and posterior screws posed the most risk to the SSN, with a 40% chance of touching the SSN [80]. Even higher rates of SSN engagement were reported in another cadaver study (n=12) in which the superior screw touched the SSN in 8 (66%) and the posterior screw in 6 specimens (50%). This group also concluded that overly long screws pose a serious risk for SSN injury and advised <2 mm penetration for superior or posterior screws [81].
One retrospective study (n=82) concluded that 13% of superior screws and 65% of posterior screws penetrated the glenoid vault. Among the superior screws, 64% had a high-risk of iatrogenic SSN neuropathy (screw tip placed within 5mm of the nerve), while only 6% of posteriorly inserted screws carried the same risk. Comparison analysis showed no difference in PROMs between the high- and low-risk (screw tip placed >5 mm of the nerve) penetrations (Table 10) [40].
In summary, four experimental studies proved that far-cortex penetration by the superior and posterior screw should be avoided to minimize the likelihood of neurovascular injuries. One experimental study described a danger zone of the superior screw between the 2- and 8-o’clock positions (using the 12 o’clock position of the right glenoid as reference). However, a clinical study showed that screw penetrations close to the SSN (high-risk) did not portend poorer clinical outcomes compared to screw penetrations far away from the nerve (low-risk).
DISCUSSION
As universal guidelines on baseplate fixation are lacking, this review sought to provide a narrative overview of the currently available evidence on ten baseplate fixation aspects in rTSA. So far, it can be deducted that: (1) Optimal screw insertion angles are unknown. Therefore, until more evidence is gathered, surgeons should focus on adequate screw puncture in anatomical safe zones and driving the inferior screw into the inferior scapular pillar; (2) Finite element studies advise the use of divergent screw patterns only, while cadaver studies conclude that both parallel or divergent patterns are sufficient for adequate stability; (3) An increasing number of screws leads to a reduced baseplate micromotion, but it is also associated with a higher risk of acromial fractures; (4) Posterior screws should be shorter or equal to 20 mm, while other screws should be 30 mm or longer; (5) If the central element does not puncture cortical bone, peripheral anterior and posterior locking screws are recommended. It is noteworthy that apart from one study, there seems to be a benefit of using at least some locking screws in baseplate constructs; (6) The optimal baseplate tilt is unknown, but the baseplate is best secured inferiorly in either slight anteversion or a neutral position; (7) There is no consensus on the best type of baseplate; and (8) Far cortex penetration should be avoided. Due to the lack of (large) clinical studies, methodological- and outcome-heterogeneity, these conclusions should be considered preliminary clinical advice.
Although this review is a collection of the best evidence available, several limitations should be acknowledged. First, the majority of the included studies were experimental studies. Therefore, their shortcomings, when compared to clinical studies, should be taken into consideration [82-84]. Furthermore, the biomechanical and virtual planning studies did not consider additional factors that are likely to affect rTSA biomechanics (e.g., stabilizing effects of ligaments, rotator cuff muscles, patients’ daily activities, and anatomical variations). Second, although no cadaver studies were judged as “poor” on quality assessment, only four out of 14 cadaver studies were assessed as having “good” quality. Third, most studies underreported their statistical results such as confidence intervals and/or standard deviations. Fourth, most included studies had methodological inconsistencies such as a lack of power, small sample size, short follow-up duration, and heterogenic outcomes. Furthermore, due to the between-study heterogeneity of the outcomes and patient characteristics, it was inappropriate to synthesize the outcomes to generate pooled effect sizes. In addition, this review only focused on studies including patients without glenoid bone loss, because baseplate fixation in patients with glenoid bone loss requires different fixation techniques compared to patients without glenoid bone loss [85]. Several clinical studies had to be excluded because they analyzed patients with and without glenoid bone loss, and data from these distinct patient groups were not extractable. A last limitation is that some studies used baseplate micromotion as the primary outcome and concluded on superiority relative to the comparison group, despite the fact that the amount of micromotion was far below the commonly accepted threshold of osseointegration failure (150 µm). Still, how much micromotion will result in clinical adverse events such as baseplate loosening and revision surgery remains unclear [86].
CONCLUSIONS
Most surgical aspects of baseplate fixation can be decided without affecting fixation strength. There is not a single strategy that provides the best outcome. Therefore, guidelines should cover multiple surgical options that can achieve adequate baseplate fixation. This also implies that surgeons can opt for their desired fixation method during surgery.
Notes
Author contributions
Conceptualization: RWAS, LAH, DFPD, MPJB. Formal analysis: RWAS, LAH, RCB. Methodology: RWAS, LAH, JWS, DFPD, MPJB. Resources: MPJB. Supervision: RCB, JWS, DFPD, MPJB. Validation: MPJB. Visualization: RWAS, LAH. Writing–original draft: RWAS, LAH. Writing–review & editing: RWAS, LAH, RCB, DFPD, MPJB.
Conflict of interest
The first author (RWAS) received funding as indicated in "Funding" section. No other potential conflicts of interest relevant to this article were reported.
Funding
The first author (RWAS) has received payments during the study period including <$10,000 from Anna Fonds NOREF (Mijdrecht, the Netherlands), <$10,000 from Michaël-van Vloten Fonds (Rotterdam, the Netherlands), and an amount between $10,000-100,000 from Prins Bernhard Cultuurfonds (Amsterdam, the Netherlands) and Flinders Foundation (Adelaide, Australia).
Data availability
None.
Acknowledgments
None.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.5397/cise.2023.00493.