|
 |
- Search
| Clin Shoulder Elb > Volume 25(2); 2022 > Article |
|
Abstract
Distal humerus fractures (DHFs) are challenging to treat due to the locally complex osseous and soft tissue anatomy. Adequate exposure of the articular surface of the distal humerus is crucial when performing an anatomical reconstruction of the elbow. Even though “triceps-on” approaches are gaining popularity, one of the most commonly used surgical treatments for DHF is olecranon osteotomy. The incidence of complications related to this approach is unclear. This review was performed to assess the type and frequency of complications that occur with the olecranon osteotomy approach in the treatment of DHF. A literature search was conducted in the PubMed/Medline, Embase, and Cochrane Library digital databases up to February 2020. Only English articles describing complications of olecranon osteotomy in the treatment of DHF were included. Data on patient and surgical characteristics and complications were extracted. Statistical analysis was performed using SPSS. A total of 41 articles describing 1,700 osteotomies were included, and a total of 447 complications were reported. Of these 447 complications, wound infections occurred in 4.2% of osteotomies, of which 1.4% were deep infections and 2.8% were superficial. Problems related with union occurred in 3.7% of osteotomies, 2% of which represented non-union and 1.7% delayed union. The high risk of complications in olecranon osteotomy must be considered in the decision to perform this procedure in the treatment of DHF.
Distal humerus fractures (DHFs) account for approximately 30% of all elbow fractures [1,2] with an incidence of 5.7/100,000 per year [1]. Treatment can be challenging due to the complex anatomic structure of the elbow joint and surrounding nerves, tendons and ligaments. Most DHFs are treated with open reduction and internal fixation using a double plating technique. Exposure of the articular surface of the elbow joint is important for successful anatomical reconstruction. However, due to the complex ligamentous anatomy and proximity of neurovascular structures, achieving adequate surgical exposure can be challenging.
Multiple approaches such as the triceps-splitting approach [3] and the triceps-sparing approach [4] have been described. Even though “triceps-on” approaches are gaining popularity, the most commonly used approach is to expose the distal humerus by performing olecranon osteotomy. Osteotomy increases exposure of the articular surface by 11%–22% compared to a triceps-splitting or -reflecting approach [5]. The osteotomy site is later fixed using tension band wiring, a screw, or a plate. Complications of olecranon osteotomy are commonly reported, including failure or pull out of the hardware used for fixation, which can result in malunion or non-union, skin penetration, infection or stiffness [2,6]. Although olecranon osteotomy is widely used by upper extremity and trauma surgeons, little is known about the frequency of associated complications. Better insight into the type and frequency of complications can aid surgeons in thoroughly informing their patients of the risks of this type of surgery. The aim of this study was to clarify the type and frequency of complications that occur after olecranon osteotomy in the treatment of DHFs and to evaluate the relative effectiveness of different types of osteotomy fixation.
This systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [6]. This review was registered in the PROSPERO (International Prospective Register of Systematic Reviews; registration number: RD42020150115).
A literature search was conducted in the PubMed/Medline, Embase, and Cochrane Library digital databases up to February 2020 to find articles that described complications or repeat operations among patients with DHF treated using the olecranon osteotomy approach. Search terms that were used were: ((((“Olecranon Process”[Mesh] OR olecranon*[tiab])) AND ((“Humerus”[Mesh] OR humerus[tiab] OR humeral[tiab]) AND (“Fractures, Bone”[Mesh] OR fractur*[tiab])))) NOT (((“Olecranon Process”[Mesh] OR olecranon*[tiab])) AND (“Osteotomy”[Mesh] OR osteotom*[tiab])).
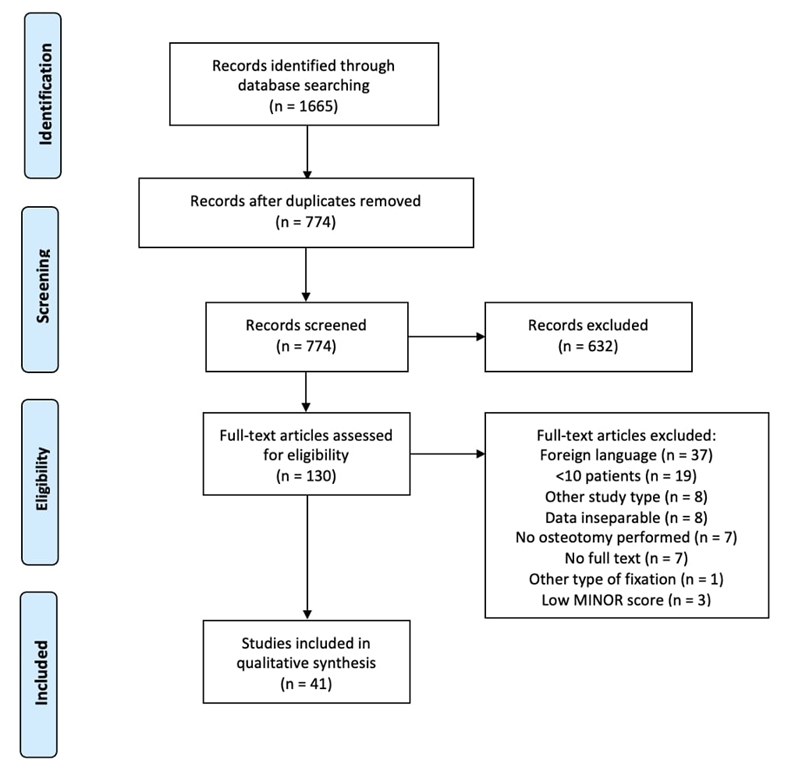
Two reviewers (KES and BJS) independently reviewed the articles by title and abstract screening. Duplicates were removed and titles were initially screened. One hundred thirty-one articles remained for whole-text screening; 90 of these were excluded, leaving 41 papers for in-depth evaluation (Fig. 1).
Studies were included in the systematic review if more than 10 patients with olecranon osteotomy in the surgical treatment of a DHF were included, patients were over 18 years old, and complications were described. Exclusion criteria were: (1) case reports, review articles, letters to the editor, conference abstracts, instructional courses, and animal/cadaver/in vitro studies; (2) a pediatric population; (3) lack of separate data on complications of olecranon osteotomy; (4) olecranon osteotomy used for treatment of other elbow pathology; (5) incomplete text; or (6) methodological index for non-randomized studies (MINOR) score lower than 10.
The methodological quality of the included articles was tested by two separate reviewers using the MINORS criteria [7] in which comparative and non-comparative studies are assessed for quality through a point system in which items that are required to be described are scored. The global ideal score is 16 for non-comparative studies and 24 for comparative studies.
Two reviewers (KS, BS) independently extracted data from each study using a predefined data extraction form. Two primary researchers (KS, BS) examined each of the articles independently and the senior author (MPJ van den Bekerom) resolved any disagreement. We extracted patient characteristics (sex and age, fracture classification, open or closed fracture, type of surgery, and type of fixation), study specific data (date of publishing, type of study, number of patients included, enrollment period, and duration of follow-up) and complication rate and type (wound complications, hardware failure, malunion or non-union, and removal of hardware).
Data were analyzed using IBM SPSS ver. 26.0 (IBM Corp., Armonk, NY, USA). The Kruskal-Wallis test was used for testing differences in complication rates between different fixation techniques of the osteotomy site. Data are shown as percentages and means with ranges and standard deviations.
A total of 1,665 articles were found using the described search criteria. After the duplicates were removed, 774 articles remained for screening. Another 632 articles were excluded, after which 131 full-text articles were assessed for eligibility. After full-text screening, 86 articles were excluded. Three more articles were excluded based on their low MINOR score, and one was excluded because of a different fixation technique of the osteotomy site. A total of 41 articles [8-48], including six prospective studies, were included in the qualitative synthesis. Articles were published between 1994 and 2020 and included 10 or more (upper limit of range, 184) osteotomies. Further information can be found in the flow diagram. Mean MINORS score was 13.4 (10–20). In these 41 articles, a total of 1,700 osteotomies in 2,030 patients were described. There were 997 males (48.8%), and the mean age was 45.3 years (range, 12–97 years). Fracture characteristics can be found in Table 1.
The mean time between injury and surgery was 1.7 days and the mean follow-up time was 22.6 months (range, 3–156 months). Most osteotomies were fixated with tension band wires (n=660), others were fixed with wires and screws (n=320), plates (n=114), and screws (n=6). Gofton et al. [22] described one case in which the osteotomy site was not fixated.
A total of 447 complications were reported. Of these 447 complications, 71 (4.2%) were wound infections, ranging from 0% to 23%. Of these, 23 (1.4%) were deep infections and 48 (2.8%) were superficial. Delayed union occurred in 29 osteotomies (1.7%), specified up to 14 months. There were 34 (2%) non-unions, and one (0.1%) malunion of the osteotomy site was described by Mardanpour and Rahbar [33]. Non-union was only specified by Schmidt-Horlohe et al. [39] (radiolucency at more than six months follow-up in association with pain) and Woods et al. [47] (radiolucency at more than nine months of follow-up). Other incidental complications, such as ulnar neuropathy, hardware failure, heterotopic ossifications and removal of hardware are described in Table 2. The only significant difference was in ulnar nerve neuropathy, which was found more frequently in osteotomy fixed with screws.
Olecranon osteotomy is a widely used approach in the surgical treatment of DHFs to establish adequate exposure of the articular surface of the distal humerus. However, this approach has high complication rates. As an alternative, less invasive techniques with potentially lower complications rates, such as the paratricipital approach, can be used [10,20,40,48]. To provide surgeons with better information on the incidence of complications related to this approach, we aimed to synthesize studies on this common approach. Therefore, this paper provides a systematic overview of the complication rate related to olecranon osteotomy in the surgical treatment of DHFs. Our data revealed that the olecranon osteotomy approach is not as forgiving as currently taught to orthopedic surgeons in training: the complication rate related to an olecranon osteotomy in the setting of DHF is high. Serious problems, such as wound infections (3.3%), delayed or non-union of the olecranon osteotomy (3.6%), ulnar neuropathy (5.5%), hardware failure (1.1%) and heterotopic ossifications (1%) are frequently encountered.
Use of olecranon osteotomy may not always be appropriate. However, in comminuted DHFs, the paratricipital approach does not provide sufficient exposure of the fracture and the joint; in these fractures, surgeons may prefer olecranon osteotomy for advanced exposure.
Difficulty achieving union can be related to inadequate reduction in complex DHFs that cannot be reconstructed anatomically, resulting in stress on the osteotomized olecranon. Delayed and non-union can also be the result of insufficient fixation. A next step in non-union of DHF can be a total elbow prosthesis. However, in the case of an earlier olecranon osteotomy, this is a more difficult surgery because of the cement that migrates into the osteotomy. In studies that compare the olecranon osteotomy approach to the triceps-splitting, triceps-lifting (paratricipital) or triceps-sparing approach, complications tend to be higher in the group that is treated via the olecranon osteotomy approach [10,20,40,48]. This may be due to the longer duration of surgery in addition to the implantation of material for osteosynthesis of the osteotomy site. Also, since the olecranon osteotomy is used more frequently in more serious fractures, these results may have been affected by bias. Based on our systematic review, 2.8% of patients had a superficial infection; however, a “superficial infection” was not well defined in most studies. As the olecranon is covered by a thin layer of skin, the osteotomy site is prone to rubbing of fixation materials, resulting in skin irritation. This can cause superficial or even deep infection. Because of the thin, soft tissue envelope of the olecranon, defining all infections as deep infections may be a safer approach.
To the best of our knowledge, this is the first review focused on complications related to olecranon osteotomy in the surgical treatment of DHF. Olecranon osteotomy is not as safe as generally considered; its high complication rate should not be underestimated. Articles comparing olecranon osteotomy to paratricipital tend to report higher complication rates, ranging from 45.8% to 55% in patients treated via the olecranon osteotomy versus 27.2% to 40.6% in patients treated via the paratricipital approach [11,20,40]. Complications related to osteotomy, such as delayed or non-union, hardware failure, and symptomatic removal of hardware, are prevented when the paratricipital approach is used. These preventable complications may require additional surgical interventions. This may discourage the use of olecranon osteotomy because the functional outcome of the paratricipital approach is often comparable to that of olecranon osteotomy. The complication rate might be underestimated, as detailed analysis with three-dimensional computed tomography is not available in most studies. As an osteotomy of the olecranon compromises the articular anatomy in most procedures, small articular steps and gaps and subtle malunion are not detected on simple radiographs, but may still cause posttraumatic osteoarthritis.
A limitation of this study is that some articles failed to separate data based on respective fixation type. Furthermore, not all articles described fracture characteristics and all types of complications. These data were not included in statistical analysis for the differences in complication rate. In this study, four different types of fixations were described: tension band wiring, screws with or without tension band, and plate fixation. No statistically significant differences were found in complication rates between these different fixation types except that more frequent ulnar nerve neuropathy was observed in osteotomies fixated with screws. However, since this was not specifically assessed in all articles, we cannot classify this as significant. Ulnar nerve neuropathy may be caused by the fixation of the osteotomy or the fixation of the fracture. We have concluded that there is no superior method for fixation in olecranon osteotomy. Randomized controlled trials (RCTs) testing the effectiveness of tension band wiring versus plate fixation are not yet available. Both tension band wiring and plate fixation of the osteotomy site have technical failures such as pull out or migration. Patients must be monitored frequently for wound healing and to identify and treat complications at an early stage. More high-quality research, such as a multi-center RCTs or a national database describing DHF treatment and outcomes, is needed to clarify the advantages and disadvantages of each technique.
Olecranon osteotomy is a frequently used approach that provides extended exposure of the articular surface of the distal humerus. However, the high risk of complications related to this approach must be considered in the decision to perform an osteotomy and/or to opt for “triceps-on” approaches. The advantages of the limited exposure increase do not outweigh the drawbacks and complications associated with this technique. Awareness of alternatives, such as the paratricipital approach, which has fewer complications and comparable functional outcomes, is essential. When selecting olecranon osteotomy, patients must be well-informed pre-operatively and monitored closely postoperatively to assess and treat possible complications at an early stage.
Table 1.
Fracture characteristics in numbers
| Variable | Tension band wire | Wire and screw | Plate | Screw |
|---|---|---|---|---|
| Sex | ||||
| Male | 419 | 100 | 14* | 40 |
| Female | 267 | 85 | 17* | 26 |
| Open | 42* | 58 | 12 | na |
| AO classification | ||||
| A2 | 9* | 0 | na | na |
| A3 | 4* | 0 | na | na |
| B1 | 1* | 0 | na | na |
| B2 | 0* | 0 | na | na |
| B3 | 1* | 0 | na | na |
| C1 | 114* | 43 | na | 1* |
| C2 | 237* | 68 | na | na |
| C3 | 178* | 74 | na | 1* |
Table 2.
Fixation types and complications
REFERENCES
1. Robinson CM, Hill RM, Jacobs N, Dall G, Court-Brown CM. Adult distal humeral metaphyseal fractures: epidemiology and results of treatment. J Orthop Trauma 2003;17:38–47.


2. Shearin JW, Chapman TR, Miller A, Ilyas AM. Ulnar nerve management with distal humerus fracture fixation: a meta-analysis. Hand Clin 2018;34:97–103.

3. Ziran BH, Smith WR, Balk ML, Manning CM, Agudelo JF. A true triceps-splitting approach for treatment of distal humerus fractures: a preliminary report. J Trauma 2005;58:70–5.


4. Bryan RS, Morrey BF. Extensive posterior exposure of the elbow: a triceps-sparing approach. Clin Orthop Relat Res 1982;(166):188–92.
5. Wilkinson JM, Stanley D. Posterior surgical approaches to the elbow: a comparative anatomic study. J Shoulder Elbow Surg 2001;10:380–2.


6. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097



7. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 2003;73:712–6.


8. Aksoy SM, Izdeş S, Kömürcü M, Bozkurt M, Başbozkurt M. Utilization of axillary brachial plexus block in the postoperative rehabilitation of intra-articular fractures of the distal humerus. Acta Orthop Traumatol Turc 2010;44:111–6.


9. Asfuroğlu ZM, İnan U, Ömeroğlu H. Open reduction and internal fixation in AO type C distal humeral fractures using olecranon osteotomy: functional and clinical results. Ulus Travma Acil Cerrahi Derg 2018;24:162–7.


10. Atif M, Hasan O, Mohib Y, Rashid RH, Hashmi P. Does surgical approach affect outcome after fixation of intra-articular fractures of distal humerus?: retrospective cohort study from a level-1 trauma centre in a metropolitan city. Ann Med Surg (Lond) 2019;43:48–51.



11. Azboy İ, Bulut M, Ancar C, et al. The comparison of triceps-reflecting anconeus pedicle and olecranon osteotomy approaches in the treatment of intercondylar fractures of the humerus. Ulus Travma Acil Cerrahi Derg 2016;22:58–65.


12. Babhulkar S, Babhulkar S. Controversies in the management of intra-articular fractures of distal humerus in adults. Indian J Orthop 2011;45:216–25.



13. Bhayana H, Pandey R, Dhammi IK, Baumann F, Bhatia U. Comparative study for assessment of functional outcome of intraarticular AO type C distal humerus fractures treated by parallel plating. Indian J Orthop 2019;53:190–5.



14. Biz C, Sperotto SP, Maschio N, Borella M, Iacobellis C, Ruggieri P. The challenging surgical treatment of closed distal humerus fractures in elderly and octogenarian patients: radiographic and functional outcomes with a minimum follow-up of 24 months. Arch Orthop Trauma Surg 2017;137:1371–83.


15. Caja VL, Moroni A, Vendemia V, Sábato C, Zinghi G. Surgical treatment of bicondylar fractures of the distal humerus. Injury 1994;25:433–8.


16. Cannada L, Loeffler B, Zadnik MB, Eglseder AW. Treatment of high-energy supracondylar/intercondylar fractures of the distal humerus. J Surg Orthop Adv 2011;20:230–5.

17. Chen G, Liao Q, Luo W, Li K, Zhao Y, Zhong D. Triceps-sparing versus olecranon osteotomy for ORIF: analysis of 67 cases of intercondylar fractures of the distal humerus. Injury 2011;42:366–70.


18. Coles CP, Barei DP, Nork SE, Taitsman LA, Hanel DP, Bradford Henley M. The olecranon osteotomy: a six-year experience in the treatment of intraarticular fractures of the distal humerus. J Orthop Trauma 2006;20:164–71.


19. Daroch MS, Sreen S, Vashisht D, Puri P. Management of intra-articular fractures of distal humerus with two column fixation with orthogonal plate construct. Int J Med Res Health Sci 2018;5:159–65.
20. Elmadag M, Erdil M, Bilsel K, Acar MA, Tuncer N, Tuncay I. The olecranon osteotomy provides better outcome than the triceps-lifting approach for the treatment of distal humerus fractures. Eur J Orthop Surg Traumatol 2014;24:43–50.


21. Eralp L, Kocaoglu M, Sar C, Atalar AC. Surgical treatment of distal intraarticular humeral fractures in adults. Int Orthop 2001;25:46–50.



22. Gofton WT, Macdermid JC, Patterson SD, Faber KJ, King GJ. Functional outcome of AO type C distal humeral fractures. J Hand Surg Am 2003;28:294–308.


23. Habib M, Tanwar YS, Jaiswal A, Singh SP, Sinha S, Lal H. Anconeus pedicle olecranon flip osteotomy: an approach for the fixation of complex intra-articular distal humeral fractures. Bone Joint J 2014;96:1252–7.

24. Hewins EA, Gofton WT, Dubberly J, MacDermid JC, Faber KJ, King GJ. Plate fixation of olecranon osteotomies. J Orthop Trauma 2007;21:58–62.


25. Jung SW, Kang SH, Jeong M, Lim HS. Triangular fixation technique for bicolumn restoration in treatment of distal humerus intercondylar fracture. Clin Orthop Surg 2016;8:9–18.



26. Kokly S, Castagna A, Mohamadreza M. Modified tension band wiring in adult distal humeral fracture types A2 and C1. Arch Bone Jt Surg 2019;7:325–30.


27. Kumar J, Katto MS, Ahmed MW, et al. Dual plating osteosynthesis technique used for fixation of inter-condylar distal humerus fractures via transolecranon approach. J Liaquat Univer Med Health Sci 2017;16:139–44.

28. Kural C, Ercin E, Erkilinc M, Karaali E, Bilgili MG, Altun S. Bicolumnar 90-90 plating of AO 13C type fractures. Acta Orthop Traumatol Turc 2017;51:128–32.



29. Lawrence TM, Ahmadi S, Morrey BF, Sánchez-Sotelo J. Wound complications after distal humerus fracture fixation: incidence, risk factors, and outcome. J Shoulder Elbow Surg 2014;23:258–64.


30. Li SH, Li ZH, Cai ZD, et al. Bilateral plate fixation for type C distal humerus fractures: experience at a single institution. Int Orthop 2011;35:433–8.


31. Liang J, Wang M, Zhao Y, Xu L, Li K. Factors affecting the functional outcome of open reduction and internal fixation on intercondylar distal humeral fractures in elderly patients. Eur J Orthop Surg Traumatol 2012;22:449–56.

32. Mahapatra S, Abraham VT. Functional results of intercondylar fractures of the humerus fixed with dual y-plate; a technical note. Bull Emerg Trauma 2017;5:36–41.


33. Mardanpour K, Rahbar M. Open reduction and internal fixation of intraarticular fractures of the humerus: evaluation of 33 cases. Trauma Mon 2013;17:396–400.



34. McKee MD, Kim J, Kebaish K, Stephen DJ, Kreder HJ, Schemitsch EH. Functional outcome after open supracondylar fractures of the humerus: the effect of the surgical approach. J Bone Joint Surg Br 2000;82:646–51.

35. McKee MD, Wilson TL, Winston L, Schemitsch EH, Richards RR. Functional outcome following surgical treatment of intra-articular distal humeral fractures through a posterior approach. J Bone Joint Surg Am 2000;82:1701–7.


36. Muzaffar N, Bhat K, Ahmad R, Wani R, Dar M. Functional results after osteosynthesis of distal humeral fractures with pre-contoured LCP system. Ortop Traumatol Rehabil 2014;16:381–5.


37. Patel J, Motwani G, Shah H, Daveshwar R. Outcome after internal fixation of intraarticular distal humerus (AO type B & C) fractures: preliminary results with anatomical distal humerus LCP system. J Clin Orthop Trauma 2017;8:63–7.



38. Ring D, Gulotta L, Chin K, Jupiter JB. Olecranon osteotomy for exposure of fractures and nonunions of the distal humerus. J Orthop Trauma 2004;18:446–9.


39. Schmidt-Horlohé K, Wilde P, Bonk A, Becker L, Hoffmann R. One-third tubular-hook-plate osteosynthesis for olecranon osteotomies in distal humerus type-C fractures: a preliminary report of results and complications. Injury 2012;43:295–300.


40. Singh R, Kanodia N, Singh H. Outcome following olecranon osteotomy versus paratricipital approach for complex intra-articular (AO 13-C) fracture of distal humerus: a prospective comparative study. J Shoulder Elbow Surg 2019;28:742–50.


41. Tak SR, Dar GN, Halwai MA, Kangoo KA, Mir BA. Outcome of olecranon osteotomy in the trans-olecranon approach of intra-articular fractures of the distal humerus. Ulus Travma Acil Cerrahi Derg 2009;15:565–70.

42. Tian D, Jing J, Qian J, Li J. Comparison of two different double-plate fixation methods with olecranon osteotomy for intercondylar fractures of the distal humeri of young adults. Exp Ther Med 2013;6:147–51.



43. Tyllianakis M, Panagopoulos A, Papadopoulos AX, Kaisidis A, Zouboulis P. Functional evaluation of comminuted intra-articular fractures of the distal humerus (AO type C): long term results in twenty-six patients. Acta Orthop Belg 2004;70:123–30.

44. Verma GC, Jilowa S, Singh J, Rathi D. Evaluation of functional outcomes of intra-articular fractures of distal humerus by open reduction and internal fixation. J Clin Diagn Res 2018;12:RC01–5.

45. Wagener ML, Dezillie M, Hoendervangers Y, Eygendaal D. Clinical results of the re-fixation of a Chevron olecranon osteotomy using an intramedullary cancellous screw and suture tension band. Strategies Trauma Limb Reconstr 2015;10:1–4.



46. Wiggers JK, Brouwer KM, Helmerhorst GT, Ring D. Predictors of diagnosis of ulnar neuropathy after surgically treated distal humerus fractures. J Hand Surg Am 2012;37:1168–72.


- TOOLS