 |
 |
- Search
| Clin Shoulder Elb > Volume 25(2); 2022 > Article |
|
Abstract
Background
Ultrasound (US)-guided techniques reported for the treatment of calcific tendinitis have mostly demonstrated good results. This study investigates the effect of US-guided barbotage using a spinal needle in patients with calcific tendinitis of the shoulder.
Methods
Thirty-six patients with calcific tendinitis of the shoulder treated by US-guided barbotage with a spinal needle and subacromial steroid injection were included in the study. We evaluated clinical outcomes based on American Shoulder and Elbow Surgeons (ASES) score, Constant score, and visual analog scale (VAS) for pain score. Radiological outcomes were assessed by X-ray imaging at each visit.
Results
Our results showed that US-guided barbotage and subacromial steroid injection produced good clinical and radiological outcomes in patients with calcific tendinitis of the shoulder. Of the 36 patients, only one required surgical treatment, while the others showed improvement without any complications. Compared to values before the procedure, calcific deposit size and VAS, ASES, and Constant scores showed significant improvement 6 weeks after the procedure. No significant correlation was found between the initial calcific deposit size and clinical outcomes at each time point.
Calcific tendinitis of the shoulder is a common condition, accounting for 7%–17% of shoulder pain cases [1-3]. It occurs more frequently in women (70% of cases) and among those in their 50s [4]. Calcific tendinitis is a self-limiting condition and can be treated conservatively with rest, physical therapy, oral pain medications like nonsteroidal anti-inflammatory drugs (NSAIDs), calcium deposit needle lavage, steroid injection, and extracorporeal shock wave therapy (ESWT) [5-9]. There is still some controversy about the optimal treatment modality for calcific tendinitis of the shoulder. Ultrasound (US)-guided techniques, such as barbotage and needle decompression for calcific tendinitis, have been reported [5,8,10-12], and most have demonstrated good outcomes. Some studies have reported that the initial size of calcium deposits do not affect the clinical outcomes in patients receiving conservative treatment [13,14]. However, treatment using US-guided barbotage with a needle has not yet been established as a standard technique.
This study analyzed the clinical and radiological outcomes of US-guided barbotage using a spinal needle and subacromial steroid injection for calcific tendinitis of the shoulder. We also investigated the influence of initial calcium deposit size on clinical outcomes. We think in patients with calcific tendinitis of the shoulder, US-guided barbotage using a spinal needle and subacromial steroid injection can yield satisfactory results both clinically and radiologically.
The study was approved by the Institutional Review Board/Ethics Committee (IRB No. CR321012), and informed consent was obtained from all participating subjects.
We evaluated 36 patients with calcific tendinitis who were treated with US-guided barbotage and subacromial steroid injection from January 2018 to December 2019. All subjects experienced shoulder pain for more than 3 months, irrespective of initial calcium deposit size. Patients with other shoulder diseases, such as rotator cuff tears (by US), glenohumeral joint arthritis, or infection, and those with a history of US-guided therapy for ipsilateral shoulder (steroid injection, barbotage, needle decompression), ESWT, or surgery were excluded from the study.
Clinical and radiological evaluations were performed before the procedure and at 6 weeks, 3, 6, and 12 months after the procedure. Routine radiological evaluations were performed using the shoulder anteroposterior view in neutral, axial, and Rockwood view. The Gärtner classification was used to assess calcific deposits the radiographs [15]. The calcific deposit size was determined at each follow-up visit using the longest measurement in any direction.
Clinical evaluations were performed using the American Shoulder and Elbow Surgeons (ASES) scores, Constant scores, and visual analog scale (VAS) for pain scores recorded at each visit. We analyzed the relationship between initial calcific deposit size and each outcome variable (VAS, ASES, and Constant scores) at different time points.
All US-guided barbotage and subacromial steroid injections were performed aseptically by a single orthopedic surgeon. First, a diagnostic US was performed, during which the biceps tendon, rotator cuff, and AC joint were checked for lesions. We also checked the location and characteristics of calcific deposits. The procedure was done in a sitting position. Examination was conducted with the patient's arm in a modified crass position. The skin was cleaned with 10% iodopovidone solution several times, aseptically draped, and treated with lidocaine for local anesthesia. After confirming the position of the calcium deposit, the needle was inserted in the short axis view. The calcific deposit was punctured with an 18-gauge needle. After confirming that the needle tip was located in a calcific deposit, it was aspirated with a 10-mL syringe, and if possible, this was repeated several times. Using a spinal needle, the deposit was punctured multiple times to achieve decompression. The final step was an injection of triamcinolone 40 mg/1 mL, hyaluronidase 0.5 mL, Ropiva 3 mL into the subacromial space under US guidance with an 18-gauge needle. All patients were prescribed 7 days of oral NSAIDs, with no specific activity restrictions.
The categorical data are reported as numbers with percentages for proportions. Continuous data are reported as median (interquartile range), and the Shapiro-Wilk test was used to determine normal distribution. A one-way analysis of variance (ANOVA) with repeated measures and Greenhouse-Geisser correction was used for patient data (with US-guided barbotage and steroid injection for calcific tendinitis of the shoulder), calcium deposit size (mm), VAS, ASES, and Constant scores recorded at different time points (before surgery, 6 weeks, 3, 6, and 12 months after the procedure). Post hoc mean comparisons with the Scheffé least significant difference test in Prism test were performed to identify time points that exhibited significant differences. Spearman's correlation analysis was performed to determine the correlation between the initial calcific deposit size and the clinical outcomes at each time point. A p-value <0.05 was considered statistically significant. R ver. 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria) was used to create a spaghetti plot and mean profile plot. All statistical analyses were conducted using the IBM SPSS 23.0 (IBM Corp, Armonk, NY, USA).
Thirty-six patients were treated with US-guided barbotage and subacromial steroid injection. Of them, 31 were women, and 5 were men. The average age of the subjects was 58 years (range, 53–61 years). While 28 patients received the injection in the dominant arm, 8 received it in the non-dominant arm. In the initial radiological evaluation, based on Gärtner classification, 18 patients had type I, while 13 had type II, and 5 had type III calcifications. The average initial calcific deposit size was 13.5 mm (range, 10.0–20.1 mm), VAS score was 6 points (range, 5.0–9.0 points), ASES score was 56 points (range, 51.5–73.5 points), and Constant score was 63 points (range, 48.0–75.0 points) (Table 1). None of the patients experienced any complications after US-guided barbotage and subacromial steroid injection.
Changes in calcific deposit size and the VAS, ASES, and Constant scores after US-guided barbotage and subacromial steroid injection were significant (Table 2, Fig. 1). Furthermore, all of the above variables showed a statistically significant changes from 6 weeks after procedure (Table 3). Of the 36 patients, one underwent arthroscopic calcification removal 4 months after the initial injection. The calcific deposit size in this patient decreased from 18.08 to 12.84 mm in 6 weeks, and VAS score dropped from 6 to 3 points. However, after 3 months, while the calcific deposit was still the same size, VAS score increased to 6 points. Although conservative treatment was recommended, further conservative treatment was refused; surgical treatment was explained and the patient consented to the procedure. After surgical treatment, pain was reduced and calcium deposits were not observed on postoperative X-ray. We found no significant relationship between initial calcific deposit size and outcome variables (VAS, ASES, and Constant scores) at different time points (Table 4).
Confirming our initial hypothesis, the study findings demonstrated reductions in pain and calcium deposit size in patients with calcific tendinitis of the shoulder who were treated with US-guided barbotage and subacromial steroid injection. Moreover, the initial calcific deposit size showed no significant correlation with clinical outcomes at each time point.
Until now, several conservative treatments have been used for patients with calcific tendinitis of the shoulder. ESWT has shown short-term and long-term clinical improvements in 53%–71% and 66%–91% of patients, respectively [15-18]. When introduced, barbotage was carried out under fluoroscopic guidance [19,20]. However, this method had the disadvantage of radiation exposure and difficulty accurately targeting calcium deposits. More recently, barbotage is increasingly being performed under US guidance, with no risk of radiation and more accurate localization of calcium deposits [10,21]. Hence, more US-guided procedures are being performed on patients with calcific tendinitis with good clinical success rates [5,6,11,14,22,23].
In a study of the US-guided needle procedure in a patient with calcific tendinitis of the shoulder, symptoms improved after 3 months, and a significant decrease in deposit size was observed after 6 months [5,23]. However, in our study, statistically significant improvement in symptoms and a decrease in deposit size were observed 6 weeks after the procedure. Unlike other studies that used an 18-gauge needle for multiple puncture decompression, we used an 18-gauge needle for aspiration and then performed multiple puncture decompression using a spinal needle, which can be used to perform decompression at deeper and more difficult angles. On the same day, a decrease in the calcific deposit size was confirmed by US; as deposit size decreased, symptoms improved.
In one study, barbotage was reported to yield better outcomes in cases with ill-defined calcifications (e.g., Gärtner type II or III classification) [11]. In another study, based on the Gärtner classification, shoulders were divided into two groups: (1) type I and (2) type II and III calcifications. The two groups presented no statistically significant differences in Constant and University of California Los Angeles scores [13]. Consistent with the latter study, we found good clinical outcomes in all patients irrespective of their Gärtner classification. Therefore, it appears that the degree of decompression of calcific deposits affects the outcome of the procedure more than patient Gärtner type.
In this study, there was no significant correlation between initial calcific deposit size and clinical outcomes at each time point. These findings were consistent with Cho et al. [13], showing no statistically significant differences in Constant and University of California at Los Angeles (UCLA) scores between calcific tendinitis patients with large- and small-sized initial calcific deposits and who received conservative treatment. Kim et al. [14] reported no significant correlation between initial calcific deposit size and clinical outcomes in calcific tendinitis patients receiving ESWT and US needle compression.
Our study has several limitations. First, there was no control group in this study. Although US-guided needle treatment had sufficiently good outcomes, a comparison with other conservative or surgical treatments would make the findings more robust. Second, as mentioned before, most study subjects were chronic patients since they had already received conservative treatments like oral medication and physical therapy at other hospitals, which had failed. Thus, in a wider population, treatment satisfaction may be increased. Given the subjective nature of the evaluation, clinical outcomes such as the ASES, Constant, and VAS scores may also have been overestimated in these subjects compared to other patients. Lastly, the number of patients in this study was small. A study with a larger sample size is needed to validate our findings. In patients with calcific tendinitis of the shoulder, US-guided barbotage using a spinal needle and subacromial steroid injection can produce clinically and radiologically satisfactory results.
Fig. 1.
Patient X-ray (A) before and (B) after the procedure, showing the change in calcific deposit.
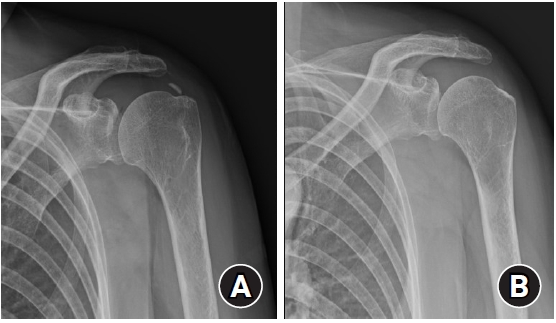
Table 1.
Baseline characteristics in patients with ultrasound-guided barbotage and steroid injections for calcific tendinitis of the shoulder
Table 2.
Result of one-way repeated measure ANOVA for time points (preoperative, 6 weeks, 3 months, 6 months, and 12 months) on treatment
| Variable | F | p-value |
|---|---|---|
| Calcium size | 45.029 | <0.001 |
| VAS score | 27.504 | <0.001 |
| ASES score | 37.126 | <0.001 |
| Constant score | 48.848 | <0.001 |
Table 3.
Result of post hoc comparisons of mean difference obtained through one-way ANOVA model
Table 4.
Correlation between the initial size of calcium deposit and clinical outcomes according to time points
REFERENCES
1. Harniman E, Carette S, Kennedy C, Beaton D. Extracorporeal shock wave therapy for calcific and noncalcific tendonitis of the rotator cuff: a systematic review. J Hand Ther 2004;17:132–51.


2. Harvie P, Pollard TC, Carr AJ. Calcific tendinitis: natural history and association with endocrine disorders. J Shoulder Elbow Surg 2007;16:169–73.


4. Mole D, Gonzalvez M, Roche O, Scarlat M. Introduction to calcifying tendinitis. In: Gazielly DF, Gleyze P, Thomas T, eds. The cuff. Paris: Elsevier; 1997. p. 141–3.
5. Aina R, Cardinal E, Bureau NJ, Aubin B, Brassard P. Calcific shoulder tendinitis: treatment with modified US-guided fine-needle technique. Radiology 2001;221:455–61.


6. del Cura JL, Torre I, Zabala R, Legórburu A. Sonographically guided percutaneous needle lavage in calcific tendinitis of the shoulder: short- and long-term results. AJR Am J Roentgenol 2007;189:W128–34.


7. Ebenbichler GR, Erdogmus CB, Resch KL, et al. Ultrasound therapy for calcific tendinitis of the shoulder. N Engl J Med 1999;340:1533–8.


9. Serafini G, Sconfienza LM, Lacelli F, Silvestri E, Aliprandi A, Sardanelli F. Rotator cuff calcific tendonitis: short-term and 10-year outcomes after two-needle US-guided percutaneous treatment: nonrandomized controlled trial. Radiology 2009;252:157–64.


10. Farin PU, Jaroma H, Soimakallio S. Rotator cuff calcifications: treatment with US-guided technique. Radiology 1995;195:841–3.


11. Farin PU, Räsänen H, Jaroma H, Harju A. Rotator cuff calcifications: treatment with ultrasound-guided percutaneous needle aspiration and lavage. Skeletal Radiol 1996;25:551–4.


12. Galletti S, Magnani M, Rotini R, et al. The echo-guided treatment of calcific tendinitis of the shoulder. Chir Organi Mov 2004;89:319–23.

13. Cho NS, Lee BG, Rhee YG. Radiologic course of the calcific deposits in calcific tendinitis of the shoulder: does the initial radiologic aspect affect the final results. J Shoulder Elbow Surg 2010;19:267–72.


14. Kim YS, Lee HJ, Kim YV, Kong CG. Which method is more effective in treatment of calcific tendinitis in the shoulder?: prospective randomized comparison between ultrasound-guided needling and extracorporeal shock wave therapy. J Shoulder Elbow Surg 2014;23:1640–6.


15. Gerdesmeyer L, Wagenpfeil S, Haake M, et al. Extracorporeal shock wave therapy for the treatment of chronic calcifying tendonitis of the rotator cuff: a randomized controlled trial. JAMA 2003;290:2573–80.


16. Daecke W, Kusnierczak D, Loew M. Long-term effects of extracorporeal shockwave therapy in chronic calcific tendinitis of the shoulder. J Shoulder Elbow Surg 2002;11:476–80.


17. Loew M, Daecke W, Kusnierczak D, Rahmanzadeh M, Ewerbeck V. Shock-wave therapy is effective for chronic calcifying tendinitis of the shoulder. J Bone Joint Surg Br 1999;81:863–7.


18. Wang CJ, Yang KD, Wang FS, Chen HH, Wang JW. Shock wave therapy for calcific tendinitis of the shoulder: a prospective clinical study with two-year follow-up. Am J Sports Med 2003;31:425–30.


19. Comfort TH, Arafiles RP. Barbotage of the shoulder with image-intensified fluoroscopic control of needle placement for calcific tendinitis. Clin Orthop Relat Res 1978;(135):171–8.


20. Patterson RL Jr, Darrach W. Treatment of acute bursitis by needle irrigation. J Bone Joint Surg Am 1937;19:993–1002.
21. Seil R, Rupp S, Hammer DS, Ensslin S, Gebhardt T, Kohn D. Extracorporeal shockwave therapy in tendionosis calcarea of the rotator cuff: comparison of different treatment protocols. Z Orthop Ihre Grenzgeb 1999;137:310–5.










