|
 |
- Search
| Clin Shoulder Elb > Epub ahead of print |
Abstract
Eponymization serves as a means of paying tribute to individuals who have made significant contributions to our culture. Each eponym is often linked with a story for everyone to discover. To aid in the retention of these stories, this review offers readers an overview of the individuals behind the eponymous terms, as well as their original descriptions, within the context of acromioclavicular joint pathology and orthopaedic surgery.
The word ŌĆ£eponymousŌĆØ in (orthopaedic) medicine most often relates to a condition, examination, or physical test, surgical technique, or grading system named after a person, usually the alleged physician or health care professional who first identified or described it. An eponymous term honours a person who makes a notable contribution to medicine.
Literature on the treatment of acromioclavicular (AC) injuries is rich with eponymization. Classifications for subluxation of the joint have been named after Tossy and Rockwood, while surgical techniques have been named after Mumford, Bosworth, and Wolter. Many eponyms serve as a useful placeholder until a descriptive term is formulated [1]. Even then, eponyms may be preferable to descriptive terms because they are usually shorter. Why say ŌĆ£stabilisation of the AC joint by distal clavicle excision and transfer of the coracoacromial ligamentŌĆØ when you can say ŌĆ£Weaver-Dunn procedure?ŌĆØ
An important aspect of eponyms is that they enliven medical history [1]. Each eponym is accompanied with a story to learn. To facilitate the remembrance of these stories, this review provides the reader with the background of individuals behind medical eponymous terms and their original description within AC joint pathology and orthopaedic surgery.
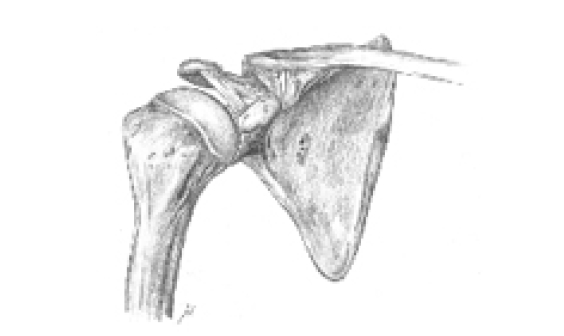
In 1941, Eugene Bishop Mumford and Fraser B. Gurd independently described resection of the distal clavicle as a surgical treatment for patients with posttraumatic, degenerative disease of the AC joint associated with osteoarthritis, fracture, separation, or shoulder impingement syndrome. Mumford published his work in the Journal of Bone and Joint Surgery.
Mumford started his article by describing the function of the clavicle. He stated that the clavicle does not have any weight-bearing function, and excellent function can be maintained in the absence of the clavicle. Mumford described resection of the distal clavicle as an alternative to other more extensive procedures. He presented a series of four patients with partial dislocation and one case of complete dislocation with an upward riding clavicle, for which Mumford suggested a fascial suture between the clavicle and the coracoid process.
Eugene Bishop Mumford was born in 1879 in Indiana, United States. He graduated from the University of Wisconsin in 1901 and from Johns Hopkins Medical School in 1905. He obtained postgraduate training at Boston ChildrenŌĆÖs Hospital and Gouverneur Hospital in New York. He returned to Indiana to establish a practice in childrenŌĆÖs orthopaedics. His practice was interrupted by World War I, in which he served as a captain in a base hospital in France. He returned to Indiana after the war and opened the Indianapolis Industrial Clinic in 1920. He later was appointed to the faculty at the Medical College of Indiana and was one of the first surgeons appointed to the James Whitcomb Riley Hospital for Crippled Children. He was also the first surgeon appointed to the VeteranŌĆÖs Administration Hospital of Indiana. Mumford was one of the founding members of the American Academy of Orthopedic Surgeons (AAOS). In addition to his clinical responsibilities, Mumford managed his familyŌĆÖs 5,800-acre farm.
Boardman Marsh Bosworth published his work leading to adaptation of the well-known Bosworth screw in the New England Journal of Medicine in 1949. He emphasized the importance of the coracoclavicular ligament because this ligament is the strongest reinforcer of the relatively fragile AC joint. For treatment of complete AC injuries, Bosworth advocated the use of a coracoclavicular screw because the operation is relatively simple and minor, performed through a small incision under local anaesthesia. He presented a series of 10 patients with follow-up varying from 4 months to 7.5 years.
Boardman Marsh Bosworth was born on June 7, 1898, in New York. Following a period of law practice, he graduated from Columbia University College of Physicians and Surgeons in 1931. He had offices in Bronxville and was on the staff of Grasslands, Lawrence, and Mount Vernon Hospitals. During World War II, Boardman Marsh Bosworth served as a major in the U.S. Army Medical Corps from 1942 to 1946 as an operating surgeon. In 1944, he was invalided back to the United States for several months during which he participated in the American College of Surgeons War Sessions program as a lecturer for the surgeon-general of the army.
On October 9, 1950, Boardman Marsh Bosworth died in a crash of his private plane in the mountainous western New Jersey. He was survived by his wife and daughter, his mother, and his two brothers, one of whom was David Marsh Bosworth (1897ŌĆō1979), after whom the Bosworth fracture of the ankle was named.
James K. Weaver and Harold K. Dunn developed a surgical technique for AC joint reconstruction and published their work in the Journal of Bone and Joint Surgery in 1972. They justified a new technique by stating that all other techniques had one or more disadvantage, such as migration or failure of fixation devices, erosion of the bone by fixation devices, recurrence of deformities, late development of joint arthralgia, and need for a second operation to remove fixation devices.
The original Weaver-Dunn procedure consisted of an oblique distal clavicle resection with a transfer of the acromial end of the coracoacromial ligament. After selection of the proper length of the coracoacromial ligament to maintain reduction, the excess ligament was cut away, and a suture of heavy, nonabsorbable material was placed in the ligament. The ligament was then pulled into the medullary canal of the clavicle, and the suture material was passed through two small drill holes in the superior cortex of the clavicle. Weaver and Dunn presented a case series of 15 patients with type III AC dislocation.
James K. Weaver was born in Fort Collins, Colorado, in 1929. After graduating from high school in 1947, he attended Harvard University. He received his medical degree from the University of Colorado Medical School in Denver, followed by a 1-year fellowship at the University of Edinburgh in Scotland. After spending several years in military service at Elgin Air Force base, he returned to the University of Colorado as an assistant professor. Later he joined the University of New Mexico in Albuquerque as the Chief of the Division of Orthopedic Surgery. He was a member of numerous orthopaedic societies and associations and president of the Western Orthopedic Society. He died September 20, 2017.
Harold K. Dunn grew up in Artesia, New Mexico, on a cattle ranch. After completing his undergraduate studies at New Mexico State University, he attended Baylor Medical School. Serving in the U.S. Army in the Vietnam War and the time spent in a General Hospital in Japan led Harold Dunn to become an orthopaedic surgeon. He performed 1 year of general surgical residency at New Mexico, finishing in 1967, where he met James Weaver, who was in the process of starting an orthopaedic residency. He completed his orthopaedic residency at Baylor in 1969 and joined the faculty of the University of Utah, where he would later become chairman, where he served as for 25 years.
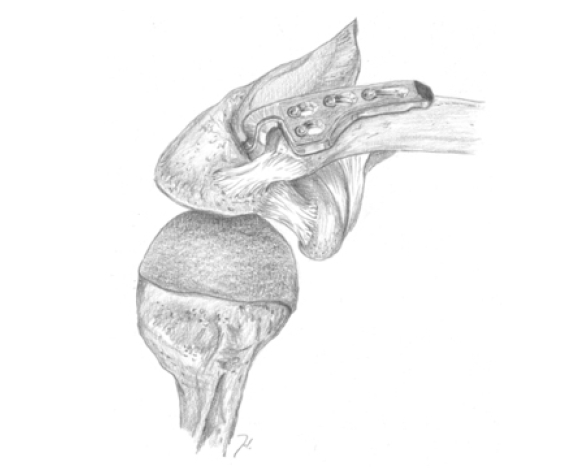
Dietmar Wolter developed his surgical technique involving an AC hook plate in 1981, and it was first performed in February 1982. Together with Christoph Eggers and Wilhelm Koch, he published this technique in ŌĆ£Abteilung f├╝r Unfall-, Wiederherstellungs- und HandchirurgieŌĆØ in 1989. The target population was patients with acute Tossy type III injuries, chronic Tossy type III injuries with failed conservative therapy, distal clavicle fractures, or distal clavicle osteoarthritis.
Typically, a four- or five-hole AC hook plate is used, followed by fixation of the plate to the distal clavicle using small fragment screws. In chronic AC dislocation, Wolter recommended the use of additional augmentation with grafts of tendons like the fascia lata. Wolter presented a case series of 84 acute AC dislocations treated with the hook-plate from 1982 to 1987.
Dietmar Wolter was born on September 27, 1941, in Klosterbr├╝ck, Germany, which is now Poland. He studied medicine in T├╝bingen and then became a resident of Martin Allg├Čwer in Basel. In 1971, he passed the U.S. Medical Licensing Examination. At 36 years of age, he was nominated as chief physician of the Department of Traumatology at the Asklepios Clinic St. Georg in Hamburg. In 1990, he was nominated as medical director and chief physician for the Department of Trauma, Plastic, and Reconstructive Surgery at the Trauma Centre in Hamburg. In his time as a surgeon, he founded several societies and a medical devices company (Litos) and launched a magazine (Trauma und Berufskrankheit). In 2002, he left his role as medical director and chief physician and concentrated on innovations of connector systems in nature, medicine, and technology.
Together with Newton C. Mead and Harley M. Sigmund, Jerome D. Tossy published the groundwork for the ŌĆ£Tossy classification in clinical orthopaedics and related researchŌĆØ in 1963. They stated that ŌĆ£the dilemmaŌĆØ (i.e., confusion as to which treatment is most suitable to any particular case) rests not in regard to any superior method, but in deciding which case is a surgical candidate. They based their classification on their experience with 49 cases at the Evanston Hospital over 10 years.
Type 1 includes sprains and contusions of the AC joint. There is no gross deformity and no more than a suggestion of separation as seen on a radiograph. In type 2, the distal clavicle may be quite prominent. On radiographs, the AC joint is separated by approximately half the normal superior-inferior depth of the joint as compared with the normal side. The increased distance between the inferior cortex of the clavicle and the superior tip of the coracoid process represents a partial tear of the conoid and trapezoid ligaments. A Type 3 separation shows a marked deformity of the distal clavicle that presents under the skin posteriorly and upwards. Radiographs show definite separation with wide separation of the coracoclavicular bone, which indicates torn conoid and trapezoid ligaments.
Jerome D. Tossy was born February 28, 1932. He was the only son of dentist Chester Tossy and theatrical singer and dancer Florence Johnson. He studied at Michigan State University then attended Wayne State University Medical School. After his orthopaedic residency, he pursued a hand surgery fellowship. After serving with the U.S. Navy, he started working at the El Camino Hospital in Mountain View, California in 1965. After practicing active orthopaedics until 1982, he consulted for 10 years. He pursued his passion for water activities by designing and building a waterfront home in the California Delta. He died on February 18, 2009.
Charles A. Rockwood Jr. revised the Tossy classification. Together with D.P. Green in 1984, he wrote the first edition of the educational book Fractures in Adults, which discussed all aspects of the AC joint from anatomy and function to diagnosis of pathology and treatment. Rockwood felt the Tossy classification needed revising because it did not consider the direction of displacement when classifying injuries. Rockwood subclassified Tossy type 3 into Rockwood types 3 to 6. Tossy types 1 and 2 correspond to the same Rockwood types.
In Rockwood type 3, the inferior border of the clavicle is elevated beyond the superior aspect of the acromion, but the coracoclavicular distance is less than twice the normal. In type 4, the AC ligaments are disrupted, and the coracoclavicular ligaments are partially or completely disrupted. The clavicle is displaced posteriorly into or through the trapezius muscle. In type 5, both the AC and coracoclavicular ligaments are disrupted with an upwards displaced clavicle. It is different from type 3 in that the upwards displaced clavicle is severe enough to ensure a coracoclavicular interspace 100%ŌĆō300% greater than that of the normal shoulder. In type 6, the AC ligaments are disrupted, and the coracoclavicular ligaments are intact or disrupted. The clavicle is displaced downwards and under either the acromion or the coracoid process.
Charles A. Rockwood Jr. was born in 1929. He graduated from Classen High School and received degrees from Oklahoma City University and the University of Oklahoma before graduating from the University of Oklahoma College of Medicine in 1956. Rockwood performed his residency at the University of Oklahoma Medical Center and served in the U.S. Air Force from 1957 to 1966, where he was the director of the Amputee and Prosthesis Clinic and chief of ChildrenŌĆÖs Orthopedics at the U.S. Air Force Medical Center in Texas. He served as editor of several textbooks, was president of the AAOS, and president of the American Shoulder and Elbow Surgeons. He served as chairman of orthopedics at the University of Texas Health Science Center for 22 years. He died on February 1, 2022.
Rockwood types I and II AC joint dislocations are generally treated nonoperatively [11]. The appropriate management of higher-grade AC separations remains unclear. Although there is some agreement among surgeons for indication for operative treatment in higher-grade dislocations, there is no high-level evidence that patients benefit from operative treatment [12-14]. The rate of return to sport after operative treatment for Rockwood types III-VI AC dislocations is high [15]. Techniques like the Bosworth screw, Weaver Dunn fixation, and the (Wolter) hook plate may be associated with higher complication and reoperation rates than more recently developed techniques [16]. Surgical interventions have shifted to more anatomic, less invasive techniques. Anatomic coracoclavicular ligament reconstruction using a tendon graft, especially in chronic cases, may be the preferred technique [17]. There also has been an increase in reoperation when using an allograft instead of an autograft [17]. When comparing open with arthroscopic AC joint reconstruction techniques, there is no difference in loss of reduction, complication rate, or revision rate based on the available literature [18].
The classification and subsequent treatment choice of AC joint dislocations remain controversial. Currently, the Tossy classification is less frequently used in clinical practice and is less accurate to guide treatment [19,20]. There is an ongoing debate about the interobserver and intraobserver reliability of the more often used original Rockwood classification [21,22]. An unreliable classification may result in inconsistent treatment outcomes among patients with similarly classified injuries and would not be a reliable guide for operative treatment.
There is no high-level evidence that operative treatment is beneficial for Rockwood type 3 injuries and no consensus among surgeons regarding the choice of treatment for these injuries, which are classified according to the Rockwood classification as disruption of both the coracoclavicular and AC ligaments. The International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine expert panel members suggest the addition of Rockwood type IIIA and type IIIB injuries to a modified Rockwood classification. Type IIIA injuries are defined by a stable AC joint without overriding of the clavicle on cross-body adduction view and without significant scapular dysfunction. The unstable type IIIB injury would be further defined by therapy-resistant scapular dysfunction and an overriding clavicle on cross-body adduction view [23].
For Rockwood type 3 injuries, there is no high-level evidence that patients benefit from surgery in higher-type AC injuries. It seems that an important issue in treatment choice is addressing the horizontal component of AC dislocations. Better appreciation of the degree of horizontal instability, especially in lower Rockwood types (II, III) of AC dislocations, may improve management of these controversial injuries [24].
Eponymous terms are common in daily orthopaedic language and AC joint pathology. When eponymous terms are used, it is crucial that all parties are aware of their true meaning. Miscommunication is a risk of variation in presumed meaning of eponymous terms [25]. Communication between colleagues with different regions of interest might especially suffer from the use of eponyms [26]. Eponymous terms should be used with caution and, when used scientifically, should be defined specifically. Because eponymous terms will most likely stay, it is necessary to ensure their uniform and consistent usage.
NOTES
REFERENCES
1. Garfield E. WhatŌĆÖs in a name? The eponymic route to immortality. Essays Inf Sci 1983;6:384ŌĆō95.
2. Mumford EB. Acromioclavicular dislocation: a new operative treatment. J Bone Joint Surg 1941;23:799ŌĆō802.
3. Homer Fauntleroy. E.B. Mumford in New Harmony, Indiana [Internet]. University of Southern Indiana [cited 2023 Mar 1]. Available from: https://digitalarchives.usi.edu/digital/collection/D_Blair/id/4209/.
4. Bosworth BM. Complete acromioclavicular dislocation. N Engl J Med 1949;241:221ŌĆō5.
5. Weaver JK, Dunn HK. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg Am 1972;54:1187ŌĆō94.


6. Villacis DC, Popkin CA, Nowell JA, et al. Standing tall on their shoulders: essential eponyms in shoulder surgery. J Shoulder Elb Arthroplast 2018;2:2471549218797723.
7. Wolter D, Eggers C, Koch W. Die operative Behandlung der akromioklavikul├żren Luxation und der distalen Klavikulafraktur oder-pseudarthrose mit der ŌĆ£AC-HakenplatteŌĆØ. Oper Orthop Traumatol 1989;1:145ŌĆō52.


8. Wikipedia contributors. Prof. Dr. Dietmar Wolter [Internet]. Wikimedia Foundation; 2012 [cited 2023 Mar 1]. Available from: https://commons.wikimedia.org/wiki/File:Prof._Dr._Dietmar_Wolter.jpg
.

9. Tossy JD, Mead NC, Sigmond HM. Acromioclavicular separations: useful and practical classification for treatment. Clin Orthop Relat Res 1963;28:111ŌĆō9.

10. Rockwood CA Jr, Williams GR Jr, Young DC. Disorders of the acromioclavicular joint. In: Rockwood CA, Matsen FA, eds. The shoulder. WB Saunders; 1998. p. 483ŌĆō553.
11. Verstift DE, Kilsdonk ID, van Wier MF, Haverlag R, van den Bekerom MP. Long-term outcome after nonoperative treatment for Rockwood I and II acromioclavicular joint injuries. Am J Sports Med 2021;49:757ŌĆō63.


12. Murray IR, Robinson PG, Goudie EB, Duckworth AD, Clark K, Robinson CM. Open reduction and tunneled suspensory device fixation compared with nonoperative treatment for type-III and type-IV acromioclavicular joint dislocations: the ACORN Prospective, Randomized Controlled Trial. J Bone Joint Surg Am 2018;100:1912ŌĆō8.

13. Rosso C, Martetschl├żger F, Saccomanno MF, et al. High degree of consensus achieved regarding diagnosis and treatment of acromioclavicular joint instability among ESA-ESSKA members. Knee Surg Sports Traumatol Arthrosc 2021;29:2325ŌĆō32.


14. Canadian Orthopaedic Trauma Society. Multicenter randomized clinical trial of nonoperative versus operative treatment of acute acromio-clavicular joint dislocation. J Orthop Trauma 2015;29:479ŌĆō87.


15. Verstift DE, Welsink CL, Spaans AJ, van den Bekerom MP. Return to sport after surgical treatment for high-grade (Rockwood III-VI) acromioclavicular dislocation. Knee Surg Sports Traumatol Arthrosc 2019;27:3803ŌĆō12.



16. Moatshe G, Kruckeberg BM, Chahla J, et al. Acromioclavicular and coracoclavicular ligament reconstruction for acromioclavicular joint instability: a systematic review of clinical and radiographic outcomes. Arthroscopy 2018;34:1979ŌĆō95.


17. Pill SG, Rush L, Arvesen J, et al. Systematic review of the treatment of acromioclavicular joint disruption comparing number of tunnels and graft type. J Shoulder Elbow Surg 2020;29(7S):S92ŌĆō100.


18. Gowd AK, Liu JN, Cabarcas BC, et al. Current concepts in the operative management of acromioclavicular dislocations: a systematic review and meta-analysis of operative techniques. Am J Sports Med 2019;47:2745ŌĆō58.


19. Feichtinger X, Dahm F, Schallmayer D, Boesmueller S, Fialka C, Mittermayr R. Surgery improves the clinical and radiological outcome in Rockwood type IV dislocations, whereas Rockwood type III dislocations benefit from conservative treatment. Knee Surg Sports Traumatol Arthrosc 2021;29:2143ŌĆō51.


20. Takase K, Hata Y, Morisawa Y, et al. Methods used to assess the severity of acromioclavicular joint separations in Japan: a survey. JSES Int 2020;4:242ŌĆō5.



21. Ringenberg JD, Foughty Z, Hall AD, Aldridge JM 3rd, Wilson JB, Kuremsky MA. Interobserver and intraobserver reliability of radiographic classification of acromioclavicular joint dislocations. J Shoulder Elbow Surg 2018;27:538ŌĆō44.


22. Schneider MM, Balke M, Koenen P, et al. Inter- and intraobserver reliability of the Rockwood classification in acute acromioclavicular joint dislocations. Knee Surg Sports Traumatol Arthrosc 2016;24:2192ŌĆō6.


23. Beitzel K, Mazzocca AD, Bak K, et al. ISAKOS Upper Extremity Committee consensus statement on the need for diversification of the Rockwood classification for acromioclavicular joint injuries. Arthroscopy 2014;30:271ŌĆō8.


24. Karargyris O, Murphy RJ, Arenas A, Bolliger L, Zumstein MA. Improved identification of unstable acromioclavicular joint injuries in a clinical population using the acromial center line to dorsal clavicle radiographic measurement. J Shoulder Elbow Surg 2020;29:1599ŌĆō605.


-
METRICS

-
- 0 Crossref
- 548 View
- 5 Download
- Related articles in Clin Should Elbow
-
Is Bending the Hook Plate Necessary in Acromioclavicular Joint Dislocation?2021 December;24(4)
Treatment of acute high-grade acromioclavicular joint dislocation2020 September;23(3)
A Clinical Analysis of Acute Acromioclavicular Dislocation 1998 June;1(1)
Operative Treatment of Distal Clavicle Fracture with Acromioclavicular Joint Injury2011 June;14(1)
Neglected Type IV Acromioclavicular Joint Injury: 2 Cases Report2008 December;11(2)