 |
 |
- Search
| Clin Shoulder Elb > Volume 26(4); 2023 > Article |
|
Abstract
Background
A precontoured plate rarely fits properly within the patient’s clavicle and must be bent intraoperatively. This study aimed to determine whether anatomical reduction could be achieved using a plate bent before surgery.
Methods
This study included 87 consecutive patients with displaced mid-shaft clavicle fractures who underwent plate fixation and were followed-up for a minimum of 1 year. After exclusions, 39 consecutive patients underwent fixation with a precontoured plate bent intraoperatively (intraoperative bending group), and 28 underwent fixation with the plate bent preoperatively (preoperative bending group). Using free software and a three-dimensional (3D) printer, ipsilateral clavicle 3D-printed models were constructed. Using plain radiographs, the distance between the edge of the lateral inferior cortex and the medial inferior cortex was measured. The angle between the line connecting the inferior cortex edge and the line passing through the flat portion of the superior cortex of the distal clavicle was measured.
Results
Mean length differences between the ipsilateral and contralateral clavicle were smaller on both anteroposterior (AP; P=0.032) and axial images (P=0.029) in the preoperative bending group. The mean angular differences on both AP (P=0.045) and axial images (P=0.008) were smaller in the preoperative bending group. No significant differences were observed between the two groups in functional scores at the last follow-up.
Conclusions
Smaller differences in length and angle between the ipsilateral and contralateral clavicle, indicative of reduction, were observed in the preoperative bending group. Using the prebending technique with low expense, the operation was performed more effectively as reflected by a shorter operation time.
Clavicle fracture is a common type of upper limb facture, accounting for 2.6%–4% of all adult fractures and 35% of shoulder girdle injuries [1]. In adults, 69%–82% of these fractures occur in the mid-shaft, and significant displacement is reported in 73% of all mid-shaft clavicle fractures [1]. Despite the high prevalence of fracture and displacement, clavicle fractures have traditionally been managed without surgical treatment on the basis of early reports suggesting that non-union and malunion are rare outcomes [2]. However, there are several studies reporting higher non-union rates with conservative treatment, ranging from 7% to 15% [3-5]. Furthermore, fracture union is commonly achieved with some degree of angulation and/or shortening. Related clinical findings after non-surgical treatment include limited range of motion, disappointing cosmetic outcomes, and residual pain [3,6]. Thus, surgical treatment for displaced clavicle fractures is increasingly performed in clinical practice [4,7].
The human clavicle has a distinct double-curved, S-shaped three-dimensional (3D) structure and shows considerable variation in terms of length, diameter, and degree of bowing [8]. Current surgical treatments include interfragmentary screw fixation, cerclage wiring, intramedullary fixation, and plate fixation [4,9-12]. Although there have been reports of reasonable results with intramedullary fixation [13,14], plate fixation is preferred in patients with displaced comminuted fractures because interposed soft tissues can impair fracture reduction [10,15]. Furthermore, plate fixation allows firm fixation via cortical bone compression and promotes resistance against rotational torque. A systematic review by Zlowodzki et al [9] demonstrated that plate fixation reduced the non-union rate for acute mid-shaft clavicle fractures to 2.2%, compared with 15.1% for conservative treatment.
There are several commercially available precontoured anatomical plates. These plates are designed to fit the natural shape of the clavicle. Pre-contoured plates were originally introduced to shorten the operation time as they eliminate the need for intraoperative plate contouring. However, the precontoured plate frequently fails to fit properly within the patient’s clavicle and must be bent intraoperatively by the surgeon.
Most assessments of clavicle fracture treatments are based on the union rate and clinical results. To our knowledge, no studies on patients with clavicle fractures have assessed the extent of anatomical reduction compared with the pre-injured state. Clavicular shortening greater than 2 cm has been used as a marker of poor clinical outcome, but this finding is controversial [3,16].
This study was performed to determine whether anatomical reduction could be achieved using a plate bent before surgery. We hypothesized that the use of pre-bent plates would result in smaller differences between the ipsilateral and contralateral clavicle, promoting more effective anatomical reduction and shorter operation times.
The study protocol was approved by the Institutional Review Board of Eunpyeong St. Mary’s Hospital (No. PC20RISI0021), which waived the requirement for informed consent due to the retrospective design. Approval was granted to “Comparison of the anatomical plate using 3D printer” (No. PIRB-20200305-005) on March 5, 2020.
The study included 87 consecutive patients with closed displaced mid-shaft clavicle fractures who underwent open reduction and internal fixation with similar products at a university hospital between January 2015 and October 2019. Plate bending was performed intraoperatively when contour mismatch was observed after reduction. After excluding 14 patients in whom plate bending was not performed intraoperatively or preoperatively, 73 patients were included. Forty-one consecutive patients underwent fixation with a precontoured plate bent intraoperatively (intraoperative bending group), and 32 consecutive patients underwent fixation with a precontoured plate bent preoperatively (preoperative bending group). After excluding two and four patients, respectively, with a less than 1-year follow-up, the final sample sizes were 39 patients in the intraoperative bending group and 28 patients in the preoperative bending group (Fig. 1). All surgeries were performed at one university hospital by the senior author. The exclusion criteria were open fracture, age younger than 17 years, previous history of fracture of the ipsilateral clavicle or shoulder, and injury of the ipsilateral side.
Demographic information is shown in Table 1. The mean patient age was 49.6±16.1 years (range, 18–76 years) in the intraoperative bending group and 53.1±19.7 years (range, 18–80 years) in the preoperative bending group (P=0.444). The Robinson classification, which is considered essential for treatment selection and prognostic assessment of mid-shaft clavicle fractures [17,18], was used to categorize patients by fracture pattern. No statistically significant difference in the Robinson classification was found between two groups (P=0.139). One patient had a zygomatic fracture, and another had scapula and glenoid fractures on the contralateral side. The mean follow-up duration was 17.3±7.3 months (range, 12–36 months) in the intraoperative bending group and 14.4±6.1 months (range, 12–42 months) in the preoperative bending group. The follow-up duration was longer in the intraoperative bending group (P=0.018).
To obtain images of the un-injured contralateral clavicle, computed tomography (CT) scans of both sides were obtained in all patients. CT axial images of both clavicles, in digital imaging and communications in medicine (DICOM) format, were obtained from the picture archiving and communication system (PACS). Free open source software, ITK SNAP (https://www.itksnap.org, ver 3.4.0), was used to reconstruct un-injured contralateral CT axial images into 3D structural images [19]. This software allowed the authors to delineate 3D anatomical structures of clavicular cortical bone. Semi-automatic segmentation was performed with this software using active contour methods. Manual segmentation was performed for thin cortical bone areas when semi-automatic segmentation was insufficient (Fig. 2).
The constructed 3D contralateral clavicle images were converted to ipsilateral clavicle images using the mirroring function in the free open source software Meshmixer (https://www.meshmixer.com, ver 3.0) (Fig. 3). Clavicular models were constructed with a fused deposition modeling type 3D printer (da Vinci 2.0A, XYZ Printing) using acrylonitrile-butadiene-styrene filaments. Each model could be printed with less than 2 U.S. dollar (USD) of filament.
For each 3D-printed clavicular model, a precontoured plate (Modular Clavicle Plate System, Synthes) was mounted on the superior aspect of the model in the best-fit position. Bending of the plate was performed to match the contour of the 3D-printed model (Fig. 4). Pre-bent plates were sterilized prior to surgery.
Each patient underwent general anesthesia and was placed in the supine position. A transverse skin incision was made over the fracture site, and soft tissue dissection was meticulously performed. After the fracture pattern had been identified, reduction was performed. In patients with comminution, interfragmentary or cerclage wiring was performed to reduce comminuted fracture fragments before placement of the plate. Reduction forceps or towel clips were occasionally used for temporary reduction maintenance. Precontoured plates (Modular Clavicle Plate System, Synthes) were used for all patients.
In the intraoperative bending group, additional plate bending was performed to match the clavicular contour. In the preoperative bending group, the pre-bent plate was mounted and fixed under the image intensifier. In both groups, a Velpeau sling was applied for 4 weeks postoperatively. Early mobilization of hand and elbow joints was initiated if the pain was tolerable. Patients were permitted to resume their normal daily activities at 6 weeks postoperatively.
Both clavicular anteroposterior (AP) and axial images were obtained immediately after the operation. The ipsilateral and contralateral lengths of the clavicle were measured in both AP and axial images. The length was measured between the edge of the lateral inferior cortex and the medial inferior cortex (Fig. 5). The clavicular angle was also measured. Specifically, the angle between the line connecting the inferior cortex edge and the line passing through the flat portion of the distal clavicular superior cortex was measured on AP images. The angle between the line passing through the flat portions of the medial and distal clavicle was measured on axial images (Fig. 6).
Length and angular differences between ipsilateral and contralateral clavicles were calculated by subtracting the ipsilateral values from contralateral values. Absolute differences were compared between the two groups. All measurements were performed independently by two orthopedic surgeons who were blinded to patient information during the measurement process (HK and HSS). Measurements were performed twice by each investigator, with a 4-week interval between measurements. Intraobserver and interobserver reliability were analyzed using intraclass correlation coefficient.
Operation times were compared between the two groups. Serial plain radiographs were collected during follow-up visits. Fracture union times and union rates were compared between the two groups. Complications were also analyzed in both groups. Non-union was defined as a radiologically visible fracture gap at six months postoperatively. Implant failure was defined as screw loosening or implant breakage without evidence of bone healing. At the last follow-up visit, functional outcomes were compared using the American Shoulder and Elbow Surgeons and Constant scoring systems.
Statistical analyses were performed using IBM SPSS statistics ver. 24.0 (IBM Corp.). Student t-test was used for comparison of radiological and clinical data between the two groups. Pearson’s chi-square test, Fisher’s exact test, and the linear by linear association test were used to compare demographic characteristics between the two groups. Mean, standard deviation, and standard error of the mean values were calculated for all variables. Statistical significance was set at P<0.05.
The mean length difference between the ipsilateral and contralateral clavicles was smaller on both AP and axial images in the preoperative bending group. The mean length difference measured on AP images was 7.9±4.8 mm in the intraoperative bending group and 5.8±3.0 mm in the preoperative bending group (P=0.032). The mean length difference measured on axial images was 8.2±5.6 mm in the intraoperative bending group and 5.3±4.3 mm in the preoperative bending group (P=0.029).
The mean angular difference between the ipsilateral and contralateral clavicle, on both AP and axial images, was smaller in the preoperative bending group. The mean angular difference measured on AP images was 4.6°±3.2° in the intraoperative bending group and 3.2°±2.1° in the preoperative bending group (P=0.045). The mean angular difference on axial image was 8.1°±6.9° in the intraoperative bending group and 4.7°±2.9° in the preoperative bending group (P=0.008).
The intraclass correlation coefficients were 0.987 (P<0.001) and 0.968 (P<0.001) for the length measurements on AP and axial images, respectively. The values were 0.911 (P<0.001) and 0.961 (P<0.001) for angulation measurements on AP and axial images, respectively.
The operation time was 85.6 minutes in the intraoperative bending group and 69.7 minutes in the preoperative bending group (P<0.001) (Table 2). One patient in the preoperative bending group exhibited delayed union. In the intraoperative bending group, one non-union, one delayed union, and two cases of screw loosening were observed. Time to union was shorter in the preoperative bending group (P=0.005). No significant difference was observed between the two groups in terms of functional scores at the last follow-up (Table 2).
When plates were pre-bent on 3D-printed models constructed using CT images of the contralateral side of the clavicle, anatomical reduction was achieved in terms of both clavicle length and angulation, which led to a shorter operation time. Surgical treatment for clavicular fractures includes interfragmentary screw fixation, cerclage wiring, intramedullary fixation, and plate fixation [20]. Leroux et al. [21] reported a revision surgery rate of 24.6%, with a non-union rate of 2.6% and malunion rate of 1.1%, among 1,350 patients who had undergone open reduction and internal fixation. Other reported complications include infection, hardware failures (e.g., plate breakage or screw pull-out), and hypertrophic scarring. Underlying neurovascular structures may also be at risk during plate fixation [22].
Most studies on clavicular fractures have been aimed at achieving fracture union, which is important for management. However, previous studies of clavicular fractures have focused on the quality of reduction and functional restoration to the preinjury state rather than anatomical reduction. Hill et al. [3] reported that the likelihood of non-union or symptomatic malunion was higher with shortening of 2 cm or more. Non-union rates of approximately 20% have been reported in patients with comminuted fractures [23,24]. van der Meijden et al. [4] proposed surgical indications including younger age, high activity level, shortening of 1.5–2 cm with or without comminution, and significant cosmetic deformity or multiple traumas.
To our knowledge, no reports have described the parameters used for assessment of clavicular fracture reduction. Therefore, we suggest that the length and angle measurements used in this study be employed (Fig. 5). Notably, operation time was shorter when using the prebending technique. Despite the commercial availability of precontoured locking plates, variations in clavicle length and angulation among individuals often lead to poorly fitting plates. Additional intraoperative bending is often necessary to match the contour and reduce the fracture gap. By prebending the plate using a 3D-printed model constructed based on the contralateral side of the clavicle, we avoided the need for additional bending of the plate during surgery. In the intraoperative bending group, more time was needed to match the contour of the plate to the temporarily fixed fracture.
Moreover, intraoperative bending did not guarantee anatomical reduction. In the absence of wide dissection, the inferior cortex could not be observed. This could complicate restoration of the clavicular angle and cause gaps in inferior fracture sites, promoting delayed union or non-union. Although there were no significant differences in complications between the two groups in this study, fewer complications may be expected with prebending of the clavicular plate due to the shorter operation time and reduced intraoperative manipulation.
This study had some limitations. First, anatomical reduction was analyzed relative to the contralateral side. Hoogervorst et al. [25] reported the potential for error when measuring the length of both clavicles side-to-side on thoracic CT. Those researchers reported that approximately 32% of patients showed asymmetry of 5 mm or more, with an absolute length difference of 3.74 mm. In that study, only length was measured on single 3D reconstructed thoracic CT images. However, the 3D position of the clavicle could cause errors in clavicular length measurements. In our study, we assessed length differences on both AP and axial images, as well as angulation on plain radiographs. Some studies have reported within-patient variation between the right and left clavicles [26-28]. We believed that the contralateral clavicle would be the most suitable reference during plate preparation. Second, the measurement methods used to assess anatomical reduction in this study have not been validated by other clinicians. Third, the plain radiographs in this study were analyzed retrospectively. Therefore, there may have been differences in methods among the technicians collecting the radiographs. Fourth, we did not determine the degree to which anatomical differences might have affected the clinical results. Notably, we found no reports discussing whether malunion affects functional outcomes. Last, this retrospective comparative study included a relatively small number of patients. However, the post hoc power was calculated to be 98.7%, with an alpha value of 0.05.
This is the first study to assess anatomical reduction relative to the contralateral side in patients with clavicular fractures. We propose a method for analyzing plain radiographs in terms of anatomical reduction in clavicular fractures. Furthermore, using free software and an entry-level 3D-printer, ipsilateral clavicle 3D-printed models were constructed. Each model could be printed with less than 2 USD of filament.
Smaller differences in length and angle between the ipsilateral and contralateral clavicles were observed in the preoperative bending group, indicative of anatomical reduction. Using the prebending technique with low expense, the operation was performed more effectively as reflected by a shorter operation time.
NOTES
Fig. 2.
Reconstruction of computed tomography (CT) axial images to three-dimensional structural images using ITK snap (version 3.4.0).
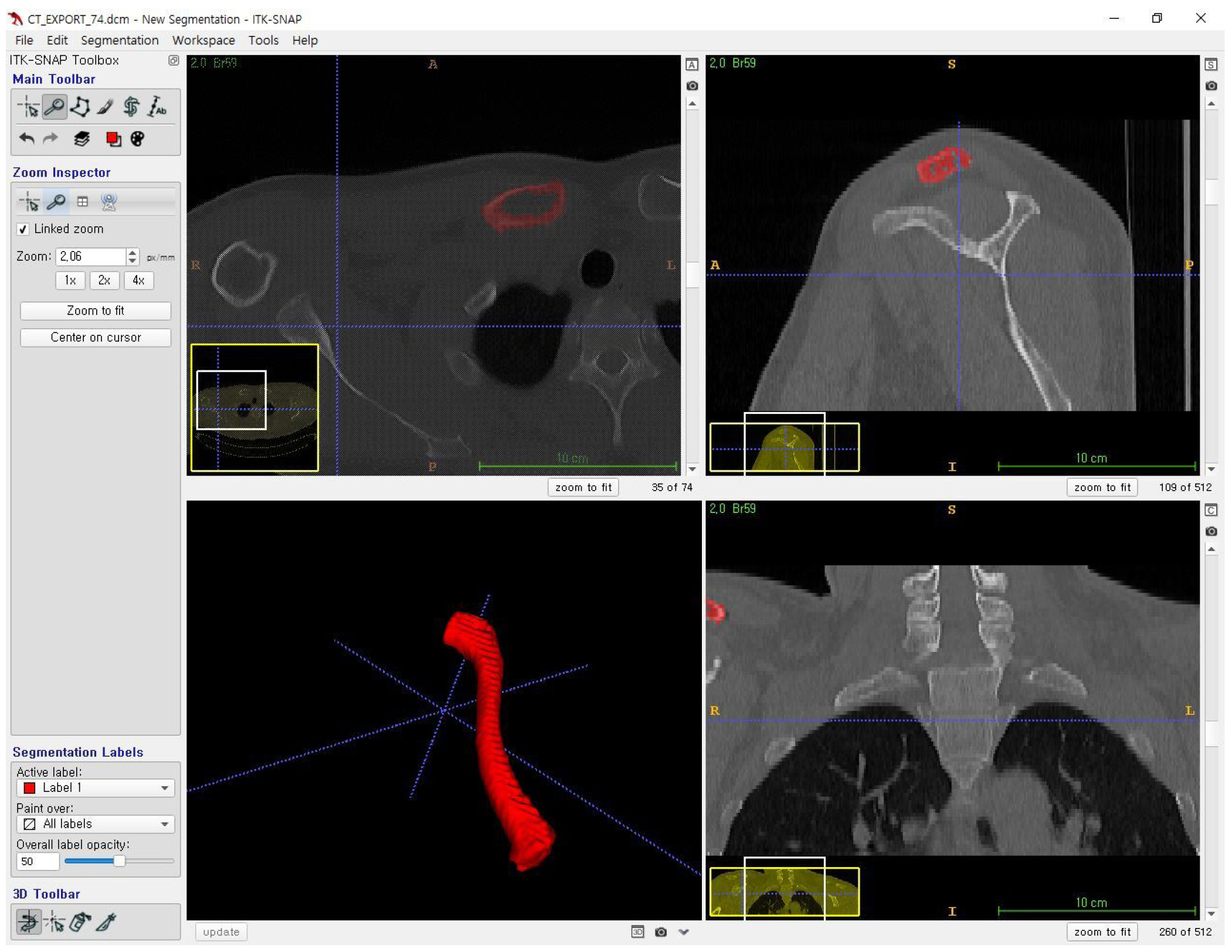
Fig. 3.
Mirroring function of Meshmixer (version 3.0) used for inversion of the contralateral clavicle.
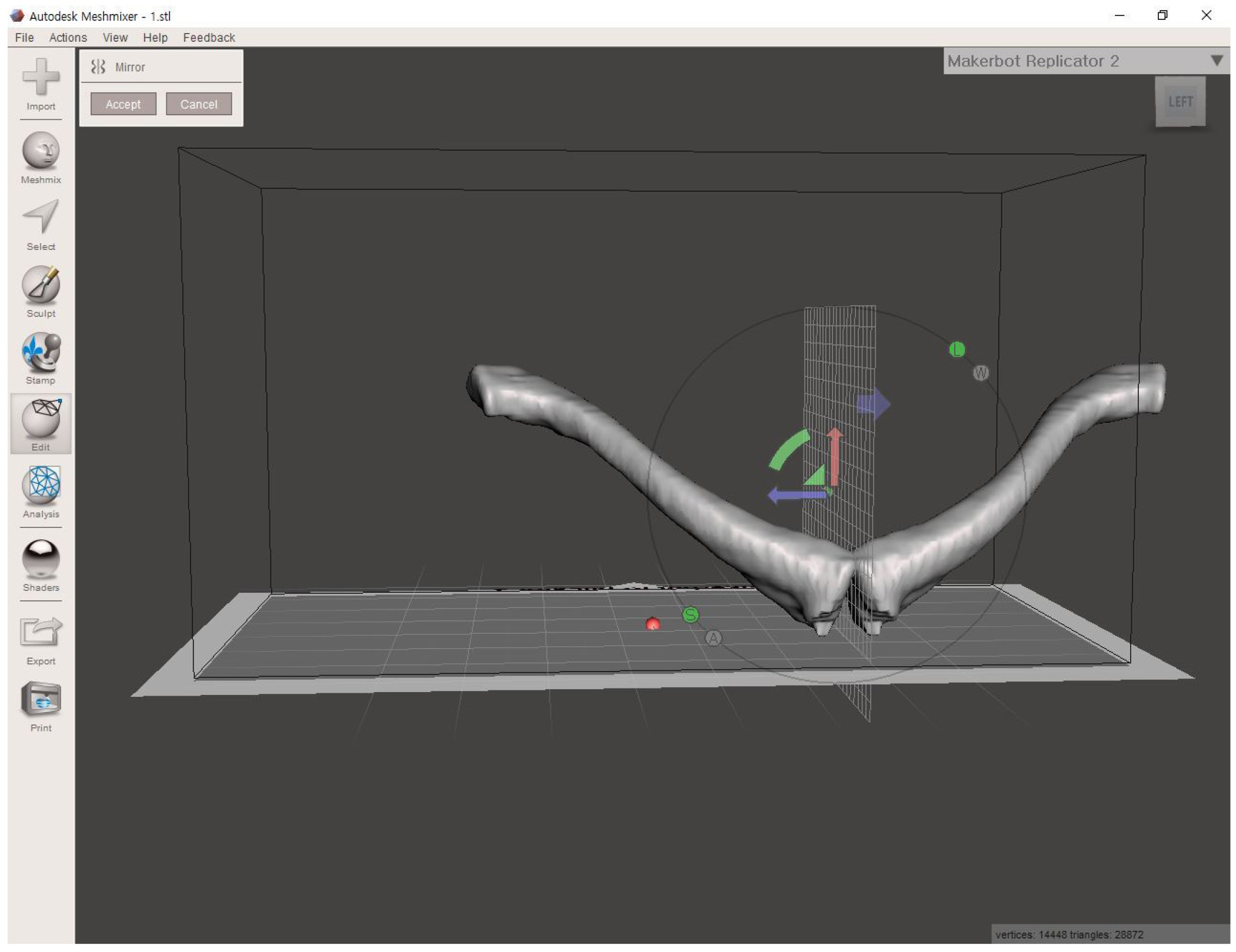
Fig. 4.
Preoperative plate bending to match the contours of the three-dimensional–printed model and plate (Synthes). A fracture line is drawn on the model. (A) Before bending (superior view and anterior view). (B) After bending (superior view and anterior view).
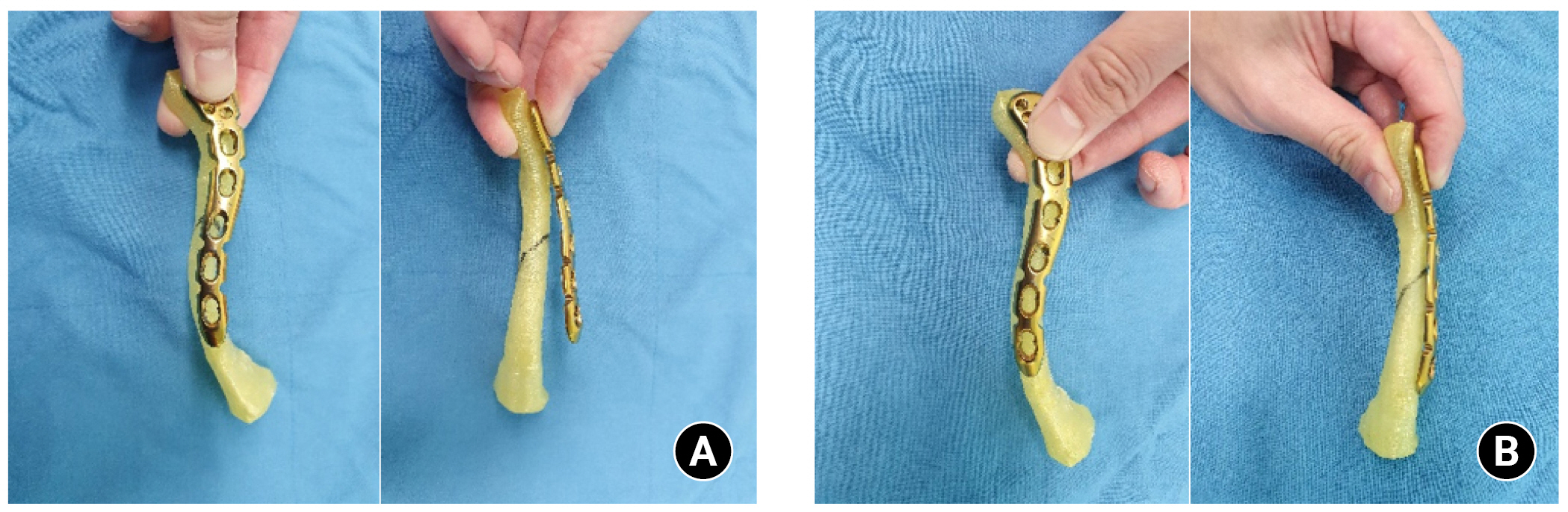
Fig. 5.
Length measurement methods. The distance between the edge of the lateral inferior cortex and the medial inferior cortex (yellow dotted line with arrows) was measured on both (A) anteroposterior and (B) axial plain radiographs. The lateral and medial border is marked with white dotted lines.
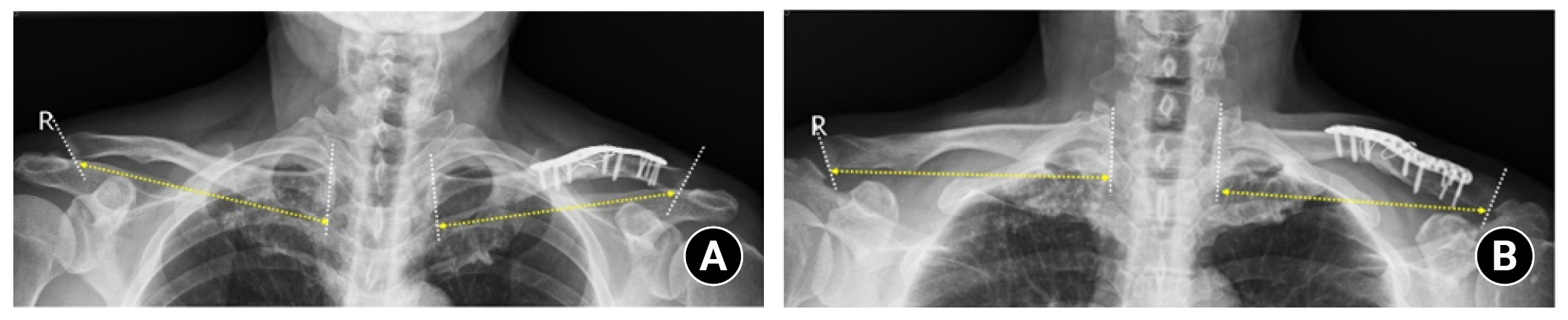
Fig. 6.
Angular measurement methods. (A) On anteroposterior images, the angle between the line connecting the inferior cortex edge and the line passing through the flat portion of the distal clavicular superior cortex was measured. (B) On axial images, the angle was measured between the line passing through the flat portion of the medial and distal clavicle.
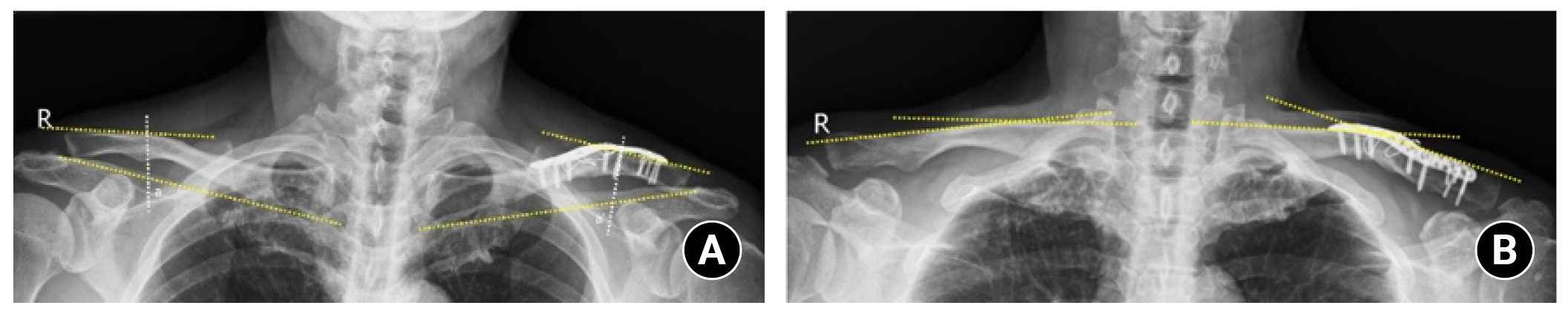
Table 1.
Patient demographic data
| Variable | Intraoperative bending group (n=39) | Preoperative bending group (n=28) | P-value |
|---|---|---|---|
| Age (yr) | 49.6±16.1 (18–76) | 53.1±19.7 (18–80) | 0.444 |
| Follow-up duration (mo) | 17.3±7.3 (12–36) | 14.4±6.1 (12–42) | 0.018 |
| Sex | 0.180 | ||
| Male | 35 | 21 | |
| Female | 4 | 7 | |
| Affected side | 0.310 | ||
| Right | 16 | 15 | |
| Left | 23 | 13 | |
| Robinson classification [18] | 0.139 | ||
| 2A2 | 4 | 4 | |
| 2B1 | 3 | 4 | |
| 2B2 | 26 | 19 | |
| 3B1 | 4 | 1 | |
| 3B2 | 2 | 0 |
Table 2.
Clinical assessment results
REFERENCES
1. Khan LA, Bradnock TJ, Scott C, Robinson CM. Fractures of the clavicle. J Bone Joint Surg Am 2009;91:447–60.


2. Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures: a multicenter, randomized clinical trial. J Bone Joint Surg Am 2007;89:1–10.
3. Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br 1997;79:537–9.


4. van der Meijden OA, Gaskill TR, Millett PJ. Treatment of clavicle fractures: current concepts review. J Shoulder Elbow Surg 2012;21:423–9.


5. Song HS, Kim H. Current concepts in the treatment of midshaft clavicle fractures in adults. Clin Shoulder Elb 2021;24:189–98.



6. Robinson CM, Goudie EB, Murray IR, et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. J Bone Joint Surg Am 2013;95:1576–84.

7. Kim HY, Yang DS, Bae JH, Cha YH, Lee KW, Choy WS. Clinical and radiological outcomes after various treatments of midshaft clavicle fractures in adolescents. Clin Orthop Surg 2020;12:396–403.



8. Huang JI, Toogood P, Chen MR, Wilber JH, Cooperman DR. Clavicular anatomy and the applicability of precontoured plates. J Bone Joint Surg Am 2007;89:2260–5.


9. Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD, Evidence-Based Orthopaedic Trauma Working Group. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma 2005;19:504–7.

10. Narsaria N, Singh AK, Arun GR, Seth RR. Surgical fixation of displaced midshaft clavicle fractures: elastic intramedullary nailing versus precontoured plating. J Orthop Traumatol 2014;15:165–71.



11. Shin WJ, Chung YW, Kim SD, An KY. Additional fixation using a metal plate with bioresorbable screws and wires for robinson type 2B clavicle fracture. Clin Shoulder Elb 2020;23:205–9.



12. Jeong JY, Chun YM. Treatment of acute high-grade acromioclavicular joint dislocation. Clin Shoulder Elb 2020;23:159–65.



13. Andrade-Silva FB, Kojima KE, Joeris A, Santos Silva J, Mattar R Jr. Single, superiorly placed reconstruction plate compared with flexible intramedullary nailing for midshaft clavicular fractures: a prospective, randomized controlled trial. J Bone Joint Surg Am 2015;97:620–6.

14. van der Meijden OA, Houwert RM, Hulsmans M, et al. Operative treatment of dislocated midshaft clavicular fractures: plate or intramedullary nail fixation?: a randomized controlled trial. J Bone Joint Surg Am 2015;97:613–9.

15. Xu B, Lin Y, Wang Z, et al. Is intramedullary fixation of displaced midshaft clavicle fracture superior to plate fixation?: evidence from a systematic review of discordant meta-analyses. Int J Surg 2017;43:155–62.


16. Wick M, Müller EJ, Kollig E, Muhr G. Midshaft fractures of the clavicle with a shortening of more than 2 cm predispose to nonunion. Arch Orthop Trauma Surg 2001;121:207–11.


17. O’Neill BJ, Hirpara KM, O’Briain D, McGarr C, Kaar TK. Clavicle fractures: a comparison of five classification systems and their relationship to treatment outcomes. Int Orthop 2011;35:909–14.


18. Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 1998;80:476–84.

19. Yushkevich PA, Piven J, Hazlett HC, et al. User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage 2006;31:1116–28.


20. Kim DW, Kim DH, Kim BS, Cho CH. Current concepts for classification and treatment of distal clavicle fractures. Clin Orthop Surg 2020;12:135–44.



21. Leroux T, Wasserstein D, Henry P, et al. Rate of and risk factors for reoperations after open reduction and internal fixation of midshaft clavicle fractures: a population-based study in Ontario, Canada. J Bone Joint Surg Am 2014;96:1119–25.

22. Collinge C, Devinney S, Herscovici D, DiPasquale T, Sanders R. Anterior-inferior plate fixation of middle-third fractures and nonunions of the clavicle. J Orthop Trauma 2006;20:680–6.


23. Jørgensen A, Troelsen A, Ban I. Predictors associated with nonunion and symptomatic malunion following non-operative treatment of displaced midshaft clavicle fractures: a systematic review of the literature. Int Orthop 2014;38:2543–9.


24. Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am 2004;86:1359–65.


25. Hoogervorst P, Appalsamy A, Franken S, van Kampen A, Hannink G. Quantifying shortening of the fractured clavicle assuming clavicular symmetry is unreliable. Arch Orthop Trauma Surg 2018;138:803–7.



26. Abdel Fatah EE, Shirley NR, Mahfouz MR, Auerbach BM. A three-dimensional analysis of bilateral directional asymmetry in the human clavicle. Am J Phys Anthropol 2012;149:547–59.


- TOOLS









