 |
 |
- Search
| Clin Shoulder Elb > Epub ahead of print |
Abstract
Background
Methods
Results
NOTES
Author contributions
Conceptualization: SKN. Data curation: AR. Formal analysis: AR, DC. Investigation: RN. Methodology: AR, SKN. Project administration: SKN, RN. Resources: AM, BKK. Software: AM, BKK, RN. Supervision: DC, SKN. Writing ŌĆō original draft: AR. Writing ŌĆō review & editing: AM, BKK, RN.
SUPPLEMENTARY MATERIALS
Supplementary┬ĀMaterial┬Ā1.
Fig.┬Ā1.

Fig.┬Ā2.
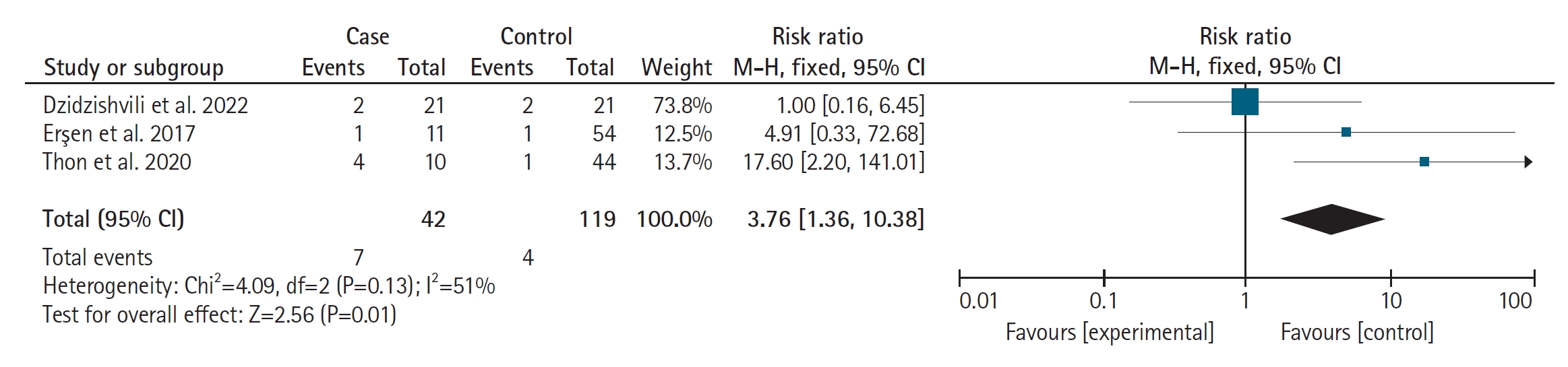
Fig.┬Ā3.

Table┬Ā1.
| Parameter | Soft tissue procedures | Latarjet operation | Bone block operation | Arthroplasty | Arthrodesis |
|---|---|---|---|---|---|
| Number of studies | 1 | 5 | 2 | 2 | 1 |
| Case/shoulder | 27/29 | 106/118 | 21/23 | 11/11 | 6/6 |
| Etiology of seizures | |||||
| ŌĆāEpilepsy | 22 | 4 | 21 | 11 | 6 |
| ŌĆāDiabetic hypoglycaemia | 3 | - | - | - | - |
| ŌĆāTramadol abuse | 2 | 1 | - | - | - |
| Bilateral case | 2 | 6 | 2 | 0 | 0 |
| Male:female | 23:4 | 39:10 | 15:6 | 9:2 | 4:2 |
| Follow-up (yr) | 3.1┬▒1.2 (2ŌĆō5) | 4.62 ┬▒ 6.5 (1ŌĆō20) | 2.65 ┬▒ 2.94 (0.75ŌĆō4) | 4.8 ┬▒ 2.26 (2ŌĆō7.5) | 3.3 ┬▒ 4.03 (1ŌĆō6.7) |
| Age at operation (yr) | 28.3┬▒6.2 (17ŌĆō42) | 29.4 ┬▒ 14.22 (19ŌĆō55) | 30.35 ┬▒ 13.64 (19.5ŌĆō46) | 39.5 ┬▒ 19.85 (17ŌĆō64) | 31 ┬▒ 11.31 (22ŌĆō38) |
| Number of dislocations before operation | 8.6┬▒2.2 (2ŌĆō12) | 12 (3ŌĆō50)a) | 46 (4ŌĆō120)b) | 4.8 ┬▒ 2.26 (2ŌĆō7.5) | - |
| Number of failed operations before inclusion into study | - | 15c) | 22 | - | 22 |
| Type of failed operation before the studied operation (shoulders) | - | Bankart = 7d) | Bankart repair = 7 | Putti-Platt = 2, allograft humeral head reconstruction = 3, Bankart repair = 2, coracoid transfer = 2, humeral head resurfacing = 1 | - |
| Bristow Latarjet = 9 | |||||
| Putti-Platt = 6 | |||||
| Mean loss of external rotation | - | - | 10┬░ŌĆō15┬░ | - | - |
| Failure/recurrence of dislocation (shoulders) | 5 (17) | 16 (13.5) | 0 | 0 | 0 |
| Recurrence of seizure in postoperative (cases) | 7 | 25 | 8e) | - | 5 |
| Revision operation for recurrence | 4 | 13 | - | - | - |
| Rowe score before operation (shoulders) | 49.1 ┬▒ 7.8 | 28.12f) | 11.3 (5ŌĆō15) | - | - |
| Rowe score after operation at latest follow-up (shoulders) | 92.1┬▒6.4 | 86.26g) | 81.8 (65ŌĆō90)h) | ||
| Oxford scores before operation | - | - | - | 11.8 ┬▒ 7.80 (5ŌĆō21) | 13 (7ŌĆō21) |
| Oxford scores after operation | - | - | - | 29.5 ┬▒ 15.08 (15ŌĆō45) | 24 (13ŌĆō36) |
| Subjective shoulder value before operation | - | - | - | 26.25 ┬▒ 36.96 (0ŌĆō80) | 37 (5ŌĆō50) |
| Subjective shoulder value after operation | 59.15 ┬▒ 29.86 (20ŌĆō90) | 42 (20ŌĆō70) |
Values are presented as mean┬▒standard deviation (range), mean (range), number (%), or mean┬▒standard deviation.
a) Four studies [3, 6,9,16] in group 2 described mean number of dislocations before operations while one study categorized cases into less than and greater than five dislocations [10].
b) One study reported the number of dislocations before operation in group 3 [13].
c) Three studies reported a number of failed operations before inclusion into the study in group 2 [3,6,16].
e) One study reported seizure recurrence in postoperative period in group 3 [13].
h) One study reported Rowe scores in group 3 [15].
Table┬Ā2.
| Parameter | Case/shoulder (37/42) | Control/shoulder (118/119) |
|---|---|---|
| Number of studies | 3 | 3 |
| Male:female | 29:8 | 53:12a) |
| Number of bilateral patients | 4 | 0 |
| Mean age (yr) | 29.73 | 29.96 |
| Mean follow-up (yr) | 4.16 | 3.46 |
| Mean number of dislocations before operation | 13.05b) | 12.3 |
| Number of failed operations before Latarjet operation (shoulder) | 4c) | 6 |
| Mean Hill-Sachs lesion size (mm, shoulders)d) | 24.7├Ś4.4 | 23.7├Ś5.2 |
| Rowe score before operation (shoulders) | 32.05e) | 34.75 |
| Rowe score after operation (shoulders) | 92.55e) | 94.45 |
| Failure/recurrence of dislocation (shoulders) | 7 | 4 |
b) One study classified cases with less than and greater than five dislocations before Latarjet operation [10]. It had 7 and 30 patients in cases and controls;
c) One study reported four failed BankartŌĆÖs operation before Latarjet procedure [6];
d) One study reported 20/21 off track Hill-Sachs lesion between cases/controls and its size [6];
REFERENCES
- TOOLS








